Abstract
Purpose
Neoadjuvant therapy (NAT) is used to treat not only advanced pancreatic cancer but also resectable lesions. The present study investigated the effectiveness of postoperative adjuvant chemotherapy for patients with pancreatic cancer who underwent surgical resection after NAT.
Methods
Patients who underwent macroscopically curative resection after NAT for pancreatic cancer were enrolled. Adjuvant chemotherapy was defined as at least 1 cycle of planned chemotherapy within 3 months after the date of surgery and included S-1, gemcitabine, or both. We retrospectively examined the effect of adjuvant chemotherapy on overall survival (OS) and recurrence-free survival (RFS) as a function of patients’ clinicopathological factors.
Results
Ninety-seven patients were included in the study, of which 68 (70.1%) underwent adjuvant chemotherapy. Administration of adjuvant chemotherapy was significantly associated with prolonged OS and RFS in patients whose elevated levels of carbohydrate antigen 19-9 or duke pancreatic monoclonal antigen type-2 did not normalize after NAT. In patients with pathological lymph node metastasis, the administration of adjuvant chemotherapy was significantly associated with longer OS but did not improve PFS.
Conclusions
Postoperative adjuvant chemotherapy was associated with prolonged postoperative survival in patients with pancreatic cancer who did not sufficiently respond to NAT as judged by tumor marker expression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Surgical resection is the only potentially curative therapy for pancreatic cancer; however, the vast majority of patients who undergo macroscopically curative resection experience relapse within 2 years.1 Two randomized, controlled trials showed that postoperative adjuvant chemotherapy using gemcitabine was associated with longer postoperative recurrence-free survival (RFS; 11.4 and 13.4 months vs. 5.6 and 6.7 months, respectively) and overall survival (OS; 22.3 and 22.8 months vs. 18.4 and 20.2 months, respectively) than surgery alone.2, 3 Several studies have since revealed the superiority of adjuvant chemotherapy using S-1, capecitabine plus gemcitabine, and modified-FOLFIRINOX (a combination of fluorouracil, leucovorin, irinotecan, and oxaliplatin) to that using gemcitabine alone.4,5,6
Although postoperative adjuvant chemotherapy is an essential component of therapeutic strategies that target pancreatic cancer, many patients cannot complete their planned courses. In previous, randomized, controlled trials that included select patients who had recovered from surgery, the rate of adjuvant chemotherapy completion was 54–79%.2,3,4,5,6 Moreover, a recent study conducted using population-based data found that only 7% of patients who underwent resection for pancreatic cancer completed their planned chemotherapy regimens, whereas 28% did not complete their courses and 65% received no adjuvant chemotherapy at all.7 Factors that potentially contributed to low adjuvant chemotherapy initiation or completion rate included high rates of postoperative complications, severe comorbidities, poor postoperative performance status (PS), and adverse effects of the treatment regimen.7
Neoadjuvant therapy (NAT) has been administered to patients with borderline resectable or unresectable pancreatic cancer to improve both resection rate and prognoses.8,9,10,11 More recently, NAT has been increasingly used for patients with resectable pancreatic cancer to improve their prognoses.12,13,14 A neoadjuvant setting ensures a higher chemotherapy completion rate than adjuvant treatment, and NAT has several potential benefits including a higher R0 resection rate following locoregional control of the primary tumor, sterilization of metastatic lymph nodes, early treatment for occult distant metastases, and identification of patients who are likely to benefit from surgical resection.15 NAT may play an important role in the treatment of patients with pancreatic cancer. However, the rate and effectiveness of adjuvant chemotherapy in patients who undergo NAT for pancreatic cancer are unknown.
Previous studies have found that lymph node metastasis, tumor size, T stage, surgical margin, histological grade, and serum carbohydrate antigen (CA) 19-9 are prognostic factors for patients with pancreatic cancer.16,17,18,19 In our earlier study, we demonstrated that elevated levels of serum CA 19-9 and its precursor duke pancreatic monoclonal antigen type 2 (DUPAN-2) were useful predictors of early hematogenous metastasis and were indications for NAT in patients with pancreatic cancer.20 Furthermore, recent studies have found that a reduction in the levels of serum tumor markers such as CA 19-9 and DUPAN-2 after NAT predicts longer survival after pancreatic cancer resection.21, 22 These prognostic factors may affect the effectiveness of postoperative adjuvant therapy in patients who underwent NAT for pancreatic cancer. The present study was designed to determine the effectiveness of postoperative adjuvant chemotherapy in patients who underwent NAT for pancreatic cancer.
Materials and Methods
Patients
Patients who underwent macroscopically curative resection after NAT for pancreatic cancer between January 2010 and December 2019 at the Department of Digestive Surgery, Breast and Thyroid Surgery, Kagoshima University, were investigated. This study was approved by the institutional ethics review board of our hospital. Written, informed consent for data analysis and publication was obtained from all subjects. Patients who did not undergo NAT were excluded from the study. Tumor’s resectability was judged according to the National Comprehensive Cancer Network guidelines.23 Tumors without arterial contact (i.e., without the celiac axis, superior mesenteric artery, or common hepatic artery) and venous contact (i.e., without the superior mesenteric vein or a portal vein of >180°) were classified as resectable. Tumors with arterial contact or venous involvement exceeding the range possible for reconstruction or those with distant metastases were classified as unresectable (UR); tumors that met neither of these criteria were considered borderline resectable (BR).
NAT and Postoperative Adjuvant Chemotherapy
NAT included chemotherapy or chemoradiotherapy (CRT). CRT was mainly performed for patients with BR or UR pancreatic cancer. Patients were considered to have undergone adjuvant chemotherapy if they had 1 cycle within 3 months after the date of surgery; treatment completion was defined as having undergone 6 cycles of planned chemotherapy within 10 months after the date of surgery. Before and after NAT, all patients underwent imaging studies including computed tomography (CT), magnetic resonance imaging (MRI), and endoscopic ultrasonography. Serum CA 19-9 and DUPAN-2 levels were measured within 2 weeks before NAT and the subsequent surgery. For all patients who recovered from surgery, we recommended receiving postoperative adjuvant chemotherapy. All resected specimens were examined histologically according to the 8th tumor-node-metastasis classification system.24 After surgery, imaging examinations including CT and MRI were performed every 4 months for the first 2 years and every 6 months for the following 3 years. The median follow-up duration was 31.0 months (mean, 35.5 months).
Statistical Analysis
Associations between different categorical variables were assessed using the χ2 or Fisher’s exact test. Survival curves were plotted using the Kaplan-Meier method and analyzed using the log-rank test. OS was calculated as the interval between surgical resection and death from any cause. RFS was calculated as the interval between surgical resection and initial recurrence. P values < 0.05 were considered statistically significant. Statistical evaluation was performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient Characteristics and Treatment Course
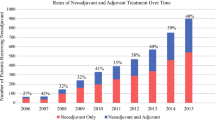
Among a total of 133 patients who underwent surgical resection for pancreatic cancer, 97 received NAT. Thirty-six patients who underwent upfront surgery were excluded from this study. All patients underwent macroscopically curative resection. The most common neoadjuvant chemotherapy (46 patients) was 2 or 3 cycles of gemcitabine (1,000 mg/m2, Days 1 and 8 of a 21-day cycle) plus S-1 (80, 100, or 120 mg/body according to body surface on Days 1 through 14 of a 21-day cycle) followed by 3 cycles of gemcitabine plus nab-paclitaxel (1,000 mg/m2 and 125 mg/m2, respectively, on Days 1, 8, and 15 of a 28-day cycle) (n = 7), gemcitabine alone (n = 4), and others (n = 5). The most common regimen of chemoradiotherapy (n = 23) included hyperfractionated accelerated radiotherapy with S-1 (56–58 Gy over 4 weeks, with S-1 at a dose of 80 mg/m2 for the first 21 days), 25 followed by chemoradiotherapy with induction chemotherapy using 2 or 3 cycles of gemcitabine plus S-1 (n = 5), 3 cycles of gemcitabine plus nab-paclitaxel (n = 5), and others (n = 2). According to the Response Evaluation Criteria in Solid Tumors (version 1.1), 1 (1.0%), 40 (41.2%), 54 (55.7%), and 2 (2.1%) patients showed complete response, partial response, stable disease, and progressive disease, respectively. In terms of surgery, pancreaticoduodenectomy was the most common procedure (n = 63), followed by distal pancreatectomy (n = 30) and total pancreatectomy (n = 4). Postoperative adjuvant chemotherapy was administered to 68 patients (70.1%), 46 (47.4%) of whom completed the planned course (Table 1). S-1 (80 mg/m2 on Days 1 through 14 of a 21-day cycle) was the most common regimen for postoperative adjuvant chemotherapy (n = 59), followed by gemcitabine alone (1,000 mg/m2 on Days 1 and 8 of a 21-day cycle, n = 7) and gemcitabine plus S-1 (n = 2). The most common reason for the nonadministration of adjuvant chemotherapy was a decline in PS after surgery (n = 11), followed by postoperative complications (n = 5), rejection (n = 5), comorbidities (n = 3), and other causes (n = 5). Additionally, reasons for the noncompletion of adjuvant chemotherapy included early recurrence (n = 11) and adjuvant chemotherapy-related adverse effects (n = 10; Table 1).
Relationship Between Clinicopathological Factors and Prognosis
Table 2 shows the relationship between clinicopathological factors and survival after surgery. Pathological tumor size of more than 20 mm and lymph node metastasis were associated with significantly shorter OS and RFS.
Effect of Postoperative Adjuvant Chemotherapy on Survival After Surgery
The administration rate of adjuvant chemotherapy was significantly higher in patients aged ≤ 70 years and with resectable pancreatic cancer. It tended to be higher in those whose CA 19-9 and DUPAN-2 levels were not normalized before surgery following NAT (Table 3). The completion rate of adjuvant chemotherapy was significantly higher in patients aged ≤ 70 years (Supplementary Table 1). In patients who underwent NAT, the median OS and RFS times were 47.7 and 20.5 months, respectively (Supplementary Fig. 1). There were no significant differences in postoperative OS and RFS between patients who received adjuvant chemotherapy after undergoing NAT plus macroscopically curative resection of pancreatic cancer and those who did not receive adjuvant chemotherapy (Fig. 1). However, patients who completed their planned adjuvant chemotherapy regimen showed significantly longer OS and RFS than did those who either skipped this therapy or did not complete it (Supplementary Fig. 2). We analyzed the effect of postoperative adjuvant chemotherapy on survival after surgery as a function of various prognostic factors (Tables 4 and 5); because only six patients underwent R1 resection, they were excluded from this analysis. Among patients with elevated serum levels of CA 19-9 (>37 U/mL) or DUPAN-2 (>150 U/mL) before surgery following NAT, administration of adjuvant chemotherapy—regardless of whether it was completed or not—was associated with significantly longer OS and RFS. In patients with pathological lymph node metastasis, administration of adjuvant chemotherapy was associated with significantly longer OS but did not significantly influence PRS. The remaining clinicopathological factors were not associated with the effect of adjuvant chemotherapy on postoperative survival.
Kaplan-Meier survival curves showing overall survival (OS) and recurrence-free survival (RFS) after surgery in patients who underwent macroscopically curative pancreatic cancer resection after neoadjuvant therapy. There was no significant difference in OS (a) or RFS (b) between patients who underwent postoperative adjuvant chemotherapy and those who did not. CI confidence interval; NA not achieved
Discussion
Previous pivotal studies have demonstrated that adjuvant chemotherapy is essential for improving the postoperative prognosis of patients with pancreatic cancer.2,3,4,5,6 However, NAT also has recently come to play an important role as a therapeutic strategy for this disease.12,13,14 The effectiveness of postoperative adjuvant chemotherapy in the era of NAT has remained unknown. In the present study, we demonstrated that the administration of postoperative adjuvant chemotherapy did not significantly influence OS or RFS among patients who underwent pancreatic cancer resection after NAT. However, patients in whom elevated serum CA 19-9 or DUPAN-2 levels did not normalize before surgery following NAT experienced significantly improved postoperative OS and RFS when treated with postoperative adjuvant chemotherapy. Moreover, patients with pathological lymph node metastasis who underwent adjuvant chemotherapy had significantly improved OS (but not RFS) compared with those who did not undergo such therapy.
It was previously reported that the omission or inability to complete postoperative adjuvant chemotherapy is not uncommon, and mainly occurred because of postoperative complications, unrecovered PS, and early recurrence after surgery.7 Previous studies found that the rates of adjuvant chemotherapy administration among patients who underwent NAT were 63–90%.9,12,14,26 In our current study, the rates of administration and completion of adjuvant chemotherapy were 70.1% and 47.4%, respectively. Patients who completed their planned courses experienced significantly longer OS and RFS than those who did not; 11 patients were unable to complete adjuvant chemotherapy due to early recurrence. In this study, we focused on investigating the effectiveness of adjuvant chemotherapy administration but not necessarily its completion. The most common reason for the lack of adjuvant chemotherapy administration was a decline in PS after surgery. We normally hesitate to administer adjuvant chemotherapy to patients who do not desire it or to those who did not sufficiently recover from their surgeries, despite receiving NAT. As such, it would be useful to identify patients with pancreatic cancer who could benefit from receiving postoperative adjuvant chemotherapy after undergoing NAT followed by surgical resection.
Elevated serum levels of tumor markers and the presence of lymph node metastasis status, which are predictors of poor prognosis in patients with pancreatic cancer, have been reported to decrease in incidence after NAT.8,11,26 In the present study, we measured serum DUPAN-2 level in addition to serum CA 19-9 level given that patients with the Lewis phenotype Lea–b- (who account for 5–10% of the population) do not have CA 19-9 production. 27 DUPAN-2 is reported to be a useful tumor marker for patients with pancreatic cancer who have the Lewis phenotype La–b-. 28 Recent studies demonstrated that patients in whom serum CA 19-9 or DUPAN-2 levels did not decrease after NAT had poor postoperative prognoses, 21,22 indicating that the persistence of elevated tumor markers after NAT is indicative of aggressive tumor biology. A recent study demonstrated that adjuvant chemotherapy after neoadjuvant FOLFIRINOX and resection of pancreatic cancer was associated with improved survival in patients with pathological lymph node metastasis, consistent with our results. 29 Adjuvant chemotherapy may be necessary to improve postoperative prognosis in patients with pancreatic cancer who did not have normalized tumor markers before surgery and who had pathologically positive lymph nodes due to the insufficient antitumor effect of NAT.
The present study had several limitations. First, given the retrospective nature of the study, the NAT regimens were not uniform among the patients included. Second, the number of patients who underwent surgical resection after NAT was relatively small, and the number of patients with pathological lymph node metastasis and nondeclined tumor marker after NAT particularly so. Hence, a prospective study with a larger sample size is required for further confirmation. Despite these limitations, this study demonstrated that the effect of adjuvant chemotherapy on the postoperative prognoses of patients with pancreatic cancer depends on the therapeutic efficacy of NAT.
Conclusions
Our findings demonstrated that postoperative adjuvant chemotherapy was associated with improved postoperative survival among patients with pancreatic cancer who maintain high serum levels of tumor markers (CA 19-9 >37 U/mL or DUPAN-2 >150 U/mL) or harbor pathological lymph node metastases after NAT.
References
Sener SF, Fremgen A, Menck HR, Winchester DP. Pancreatic cancer: a report of treatment and survival trends for 100,313 patients diagnosed from 1985–1995, using the National Cancer Database. J Am Coll Surg. 1999;189:1–7.
Ueno H, Kosuge T, Matsuyama Y, et al. A randomised phase III trial comparing gemcitabine with surgery-only in patients with resected pancreatic cancer: Japanese Study Group of Adjuvant Therapy for Pancreatic Cancer. Br J Cancer. 2009;101:908–15.
Oettle H, Neuhaus P, Hochhaus A, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013;310:1473–81.
Uesaka K, Boku N, Fukutomi A, et al. Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet. 2016;388:248–57.
Neoptolemos JP, Palmer DH, Ghaneh P, et al. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet. 2017;389:1011–24.
Conroy T, Hammel P, Hebbar M, et al. FOLFIRINOX or gemcitabine as adjuvant therapy for pancreatic cancer. N Engl J Med. 2018;379:2395–406.
Altman AM, Wirth K, Marmor S, et al. Completion of adjuvant chemotherapy after upfront surgical resection for pancreatic cancer is uncommon yet associated with improved survival. Ann Surg Oncol. 2019;26:4108–16.
Ferrone CR, Marchegiani G, Hong TS, et al. Radiological and surgical implications of neoadjuvant treatment with FOLFIRINOX for locally advanced and borderline resectable pancreatic cancer. Ann Surg. 2015;261:12–7.
Rose JB, Rocha FG, Alseidi A, et al. Extended neoadjuvant chemotherapy for borderline resectable pancreatic cancer demonstrates promising postoperative outcomes and survival. Ann Surg Oncol. 2014;21:1530–7.
Kurahara H, Shinchi H, Ohtsuka T, et al. Significance of neoadjuvant therapy for borderline resectable pancreatic cancer: a multicenter retrospective study.Langenbecks Arch Surg. 2019;404:167–74.
Nagakawa Y, Sahara Y, Hosokawa Y, et al. Clinical impact of neoadjuvant chemotherapy and chemoradiotherapy in borderline resectable pancreatic cancer: analysis of 884 patients at facilities specializing in pancreatic surgery.Ann Surg Oncol. 2019;26:1629–36.
Eguchi H, Takeda Y, Takahashi H, et al. A Prospective, open-label, multicenter phase 2 trial of neoadjuvant therapy using full-dose gemcitabine and S-1 concurrent with radiation for resectable pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2019;26:4498–505.
Motoi F, Kosuge T, Ueno H, et al. Randomized phase II/III trial of neoadjuvant chemotherapy with gemcitabine and S-1 versus upfront surgery for resectable pancreatic cancer (Prep-02/JSAP05). Jpn J Clin Oncol. 2019;49:190–4.
Barbour AP, Samra JS, Haghighi KS, et al. The AGITG GAP Study: A phase II study of perioperative gemcitabine and nab-paclitaxel for resectable pancreas cancer. Ann Surg Oncol. 2020;27:2506–15.
Katz MH, Pisters PW, Lee JE, Fleming JB. Borderline resectable pancreatic cancer: what have we learned and where do we go from here? Ann Surg Oncol. 2011;18:608–10.
Ballehaninna UK, Chamberlain RS. The clinical utility of serum CA 19–9 in the diagnosis, prognosis and management of pancreatic adenocarcinoma: an evidence based appraisal. J Gastrointest Oncol. 2012;3:105–19.
Paniccia A, Hosokawa P, Henderson W, et al. Characteristics of 10-year survivors of pancreatic ductal adenocarcinoma. JAMA Surg. 2015;150:701–10.
Qiu M, Qiu H, Jin Y, et al. Pathologic diagnosis of pancreatic adenocarcinoma in the United States: Its status and prognostic value. J Cancer. 2016;7:694–701.
Kurahara H, Maemura K, Mataki Y, et al. A therapeutic strategy for resectable pancreatic cancer based on risk factors of early recurrence. Pancreas. 2018;47:753–8.
Kurahara H, Maemura K, Mataki Y, et al. Clinical significance of serum carbohydrate antigen 19.9 and duke pancreatic monoclonal antigen type 2 for the prediction of hematogenous metastases in patients with pancreatic ducal adenocarcinoma. Pancreatology. 2016;16:1051–6.
Sunagawa Y, Yamada S, Sato Y, et al. Novel prognostic implications of DUPAN-2 in the era of initial systemic therapy for pancreatic cancer. Ann Surg Oncol. 2020;27:2081–9.
Aoki S, Motoi F, Murakami Y, et al. Decreased serum carbohydrate antigen 19–9 levels after neoadjuvant therapy predict a better prognosis for patients with pancreatic adenocarcinoma: a multicenter case-control study of 240 patients. BMC Cancer. 2019;19:252.
Tempero MA, Malafa MP, Al-Hawary M, et al. Pancreatic adenocarcinoma version NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2017;15:1028–61.
Chun YS, Pawlik TM, Vauthey JN. 8th Edition of the AJCC Cancer staging manual: pancreas and hepatobiliary cancers. Ann Surg Oncol. 2018;25:845–7.
Shinchi H, Maemura K, Mataki Y, et al. A phase II study of oral S-1 with concurrent radiotherapy followed by chemotherapy with S-1 alone for locally advanced pancreatic cancer. J Hepatobiliary Pancreat Sci. 2012;19:152–8.
Motoi F, Ishida K, Fujishima F, et al. Neoadjuvant chemotherapy with gemcitabine and S-1 for resectable and borderline pancreatic ductal adenocarcinoma: results from a prospective multi-institutional phase 2 trial. Ann Surg Oncol. 2013;20:3794–801.
Park JK, Paik WH, Ryu JK, et al. Clinical significance and revisiting the meaning of CA 19–9 blood level before and after the treatment of pancreatic ductal adenocarcinoma: analysis of 1,446 patients from the pancreatic cancer cohort in a single institution. PLoS One. 2013;8:e78977.
Kawa S, Tokoo M, Oguchi H, et al. Epitope analysis of SPan-1 and DUPAN-2 using synthesized glycoconjugates sialyllact-N-fucopentaose II and sialyllact-N-tetraose. Pancreas. 1994;9:692–7.
van Roessel S, van Veldhuisen E, Klompmaker S, et al. Evaluation of adjuvant chemotherapy in patients with resected pancreatic cancer after neoadjuvant FOLFIRINOX treatment. JAMA Oncol. 2020. https://doi.org/10.1001/jamaoncol.2020.3537.
Acknowledgment
This study was funded by a Grants-in-Aid for Scientific Research (18K08626) from the Japan Society for the Promotion of Science, which is under the direction of the Ministry of Health, Labor, and Welfare, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
DISCLOSURE
The authors declare that they have no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Kurahara, H., Mataki, Y., Idichi, T. et al. Effectiveness of Adjuvant Therapy in Patients with Pancreatic Cancer Who Underwent Neoadjuvant Therapy. Ann Surg Oncol 28, 6238–6245 (2021). https://doi.org/10.1245/s10434-021-09712-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09712-6