Abstract
Background
Cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) have been associated with significant morbidity and increased hospital length of stay (LOS). The authors report their experience after implementation of an enhanced recovery after surgery (ERAS) program for CRS-HIPEC.
Methods
Outcomes were analyzed before and after ERAS implementation. The components of ERAS included preoperative carbohydrate loading, goal-directed fluid management, multimodal pain management, minimization of narcotic use, avoidance of nasogastric tubes, and early mobilization and feeding.
Results
Of 168 procedures, 88 (52%) were in the pre-ERAS group and 80 (48%) were in the post-ERAS group. The two groups did not differ in terms of age, sex, comorbidities, peritoneal carcinomatosis index scores, completeness of cytoreduction, or operative time. The ERAS patients received fewer fluids intraoperatively (mean, 4.2 vs 6.4 L; p < 0.01). The mean LOS was 7.9 days post-ERAS compared with 10.0 days pre-ERAS (p = 0.015). Clavien–Dindo complications classified as grade ≥ 3 were lower after ERAS (23.7% vs 38.6%; p = 0.04). Moreover, the readmission rates remained the same (16.2% vs 13.6%; p = 0.635).
Conclusions
Implementation of an ERAS program for patients undergoing CRS-HIPEC is feasible and not associated with an increase in overall major complications or readmissions. These data support incorporation of ERAS protocols for CRS-HIPEC procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Management of peritoneal metastases (PM) poses unique challenges in oncology because effective treatment options that address both short- and long-term outcomes are limited.1,2 Cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) have emerged as a promising approach for treating PM in a variety of primary sites including the appendix, colon, stomach, ovaries, and mesothelium.3,4,5,6,7,8 Whereas CRS aims to extirpate visible tumor deposits through peritonectomy procedures and visceral resections, HIPEC addresses microscopic disease.9
The use of HIPEC may compound inherent surgical risks of CRS by altering intraoperative hemodynamics, augmenting fluid and electrolyte shifts, and effecting immunosuppression.10,11
Early experience with CRS-HIPEC was associated with substantial morbidity and mortality, which led to significant trepidation and slow adoption of this technique.12,13 Over time, management strategies evolved to mitigate risk, and practices such as nasogastric decompression, liberal use of intravenous fluids, delayed feeding, and triage to intensive care units (ICUs) became standard. As outcomes improved, CRS-HIPEC use increased, and currently, morbidity and mortality rates are comparable with those for other major oncologic operations.14,15,16
Recently, the Chicago Consensus on Peritoneal Surface Malignancies established guidelines to standardize practices and set clinical quality benchmarks.17 Among these, target rates for total LOS and ICU length of stay were suggested. Enhanced recovery after surgery (ERAS) protocols incorporate evidence-based interventions collectively designed to shorten recovery time.18
Originally studied in colorectal surgery, ERAS programs currently are widely adopted.19 Although specific interventions such as goal-directed fluid management and multimodal pain control have been studied in the context of CRS-HIPEC, the impact of comprehensive ERAS protocols is less well described.20,21,22,23,24,25 This study aimed to assess the feasibility of implementing an ERAS protocol for CRS-HIPEC procedures and to examine its impact on short-term outcomes.
Methods
Study Design
A single-institution retrospective analysis of a prospectively maintained database was performed. The analysis included patients older than 18 years who underwent CRS-HIPEC between 2013 and 2019. It excluded patients who underwent CRS without HIPEC and cases aborted due to disease extent discovered at the time of surgery. Institutional review board (IRB) approval was obtained, and data collection was compliant with the Health Insurance Portability and Accountability Act (HIPAA). The operations were performed by two surgical oncologists (G.S. and F.D.).
The patients were temporally stratified into pre- and post-ERAS groups as implementation took place in January 2017. Clinicopathologic data were collected prospectively as part of an ongoing research study and maintained in an electronic dataset. Variables including age, gender, perioperative serum creatinine, body mass index (BMI), American Society of Anesthesiologist (ASA) scores, and presence of existing comorbidities (defined as one or more of the following: coronary artery disease, obesity, or diabetes) were abstracted. Additional intraoperative information on peritoneal cancer index (PCI) scores, rates of completeness of cytoreduction (CC0/CC1), type of chemotherapy in perfusate, estimated blood loss (EBL), and intraoperative fluid administration were derived.
The study primarily aimed to evaluate the impact of ERAS on LOS, 30-day readmission rates, and 30-day morbidity and mortality. A secondary aim was to determine rates of acute kidney injury (AKI) as defined by Kidney Disease Improving Global Outcomes (KDIGO) criteria.25,26 Clavien–Dindo classification (CD) was used to document morbidity. Minor complications were defined as any deviation from the postoperative course treated medically. Major complications (grade ≥ 3) required operative, endoscopic, or radiologic interventions or were considered life-threatening (needing ICU management, leading to single- or multi-organ dysfunction).
The components of ERAS are summarized in Table 1. Interventions were divided into three phases of care: preoperative, intraoperative, and postoperative. Individual aspects of the protocol were compiled by reviewing the literature and after multidisciplinary approval from the surgical and anesthesiology teams.
All cases intended for CRS-HIPEC were evaluated beforehand at the Tumor Board by the multidisciplinary team. Preoperatively, the patients were counseled in person and provided with a handbook detailing the anticipated course. At the time of the initial encounter with the operating surgeon, the patients with a performance status (PS)27 higher than 0 (i.e., fully active and able to perform all pre-diagnosis activities without restriction) were referred to a physical therapist. The physical therapist then prescribed formal extended prehabilitation after evaluating active range of motion, timed up-and-go,28 gait, and the Blessed Orientation Memory Concentration (BOMC) score.29
Timed Up and Go. If patients performed well on the aforementioned measures, a set of home exercises designed to improve overall fitness were recommended. Nutritional needs also were screened during the initial encounter, and a licensed clinical dietician was consulted if any of the following criteria were met: BMI lower than 20 kg/m2, unplanned weight loss greater than 10% in the previous 6 months, or a serum albumin level lower than 3.0. Specific interventions were outlined by the dietitian, including provision of a log detailing daily intake and a protein-rich diet (goal of 2.0 g of protein/kg/day) as well as nutritional supplements. The patients were encouraged to attend a preoperative class devised and conducted by nursing leaders outlining hospitalization expectations such as postoperative mobilization, pain control, and incentive spirometry. A carbohydrate-rich drink was prescribed to be consumed the night before and the morning of the operation, consistent with ASA guidelines.30
Before implementing the ERAS protocol, the operating surgeons met with the anesthesiology team and established evidence-based consensus around intraoperative components. A “core” group of anesthesiologists acquainted with the protocol and management nuances of HIPEC procedures were identified to minimize practice variation. A lung-protective ventilation strategy was used, and intravenous fluid was administered in a goal-directed manner by tracing intra-arterial waveforms to estimate pulse pressure variations (PPV).26 Sustained hypotension greater than 10% to 15% PPV generally was treated with small boluses of crystalloid or colloid solutions. Pressors were used as appropriate. Core temperature was monitored continuously, and normothermia was carefully maintained through fluid, forced-air warmers, and active cooling.
A multimodal strategy for analgesia also was used with the goal of minimizing narcotic use while facilitating postoperative ambulation and rehabilitation. We adopted a regimen after reviewing the literature for similar protocols. For example, the use of nonsteroidal anti-inflammatory agents such as ketorolac has been shown to produce analgesia superior to opioids alone and is further associated with a lower incidence of opioid-related side effects including nausea and vomiting and sedation.31
Oral acetaminophen (1000 mg) was administered preoperatively, and intravenous lidocaine was infused at 2 mg/kg/h of ideal body weight throughout the operation.32,33 At the conclusion, bilateral ultrasound-guided transversus abdominis plane (TAP) nerve blocks were administered. It should be noted that the multidisciplinary team agreed to abandon the use of epidural catheters given potential associated complications such as motor blockade, catheter malfunction, and urinary tract infections. Moreover, findings have shown that TAP nerve blockade is not inferior to epidurals in terms of pain relief.34
During the postoperative phase, pain management consisted of scheduled intravenous acetaminophen, patient-controlled analgesia (PCA), and ketorolac when not otherwise contraindicated. Decisions on maintaining nasogastric tube (NGT) decompression were made intraoperatively, and NGTs generally were avoided completely in cases with the upper abdomen spared from disease,. Alternatively, when an NGT was placed, an effort is made to remove it on postoperative day (POD) 1 if output was lower than 400 mL per 24 h. Oral intake of clear liquids was allowed on POD 1, and diet was advanced as tolerated thereafter. Intravenous ondansetron was scheduled until POD 2, when it was given on an as-needed basis.
All the patients were evaluated by physical therapy, and early mobility was instituted. The goals for discharge included ability to tolerate an adequate oral diet, ability to function independently, and pain control with oral medications. Follow-up evaluation was established within less than a week from the date of discharge.
Statistical Analysis
The χ2 test was used to compare categorical variables, and an independent-samples t test was used for continuous variables. To examine the association between the implementation of ERAS and the occurrence of grade 3 or 4 morbidity and AKI, multivariate linear regression analysis was performed. Results were considered statistically significant at a p value lower than 0.05. All statistical analyses were performed using SPSS, version 26 (IBM SPSS Statistics for Macintosh, version 24.0; IBM Corp, Armonk, NY, USA).
Results
Demographics and Intraoperative Details
After application of the inclusion and exclusion criteria, 168 cases were included in the study. These 168 cases included 72 (42.9%) involving an appendiceal primary, 40 (23.8%) involving a colonic site, 19 (11.3%) involving an ovarian site, 6 (3.6%) involving a gastric site, and 50 (29.8%) involving other sites. Of the 168 patients, 88 (52.4%) were pre-ERAS, and 80 (47.6%) were post-ERAS. The patients did not differ in terms of age, gender distribution, BMI, ASA class, associated comorbidities, or baseline renal function. Moreover, the PCI scores, rates of CC0/CC1 resections, operative time, and type of HIPEC chemotherapy were similar before and after ERAS (p > 0.05 for all). Notably, after ERAS, a significant decrease in intravenous fluid administration (4.2 vs 6.4 L) and EBL (216 vs 362 mL) was observed (p < 0.01) (Table 2).
Outcomes
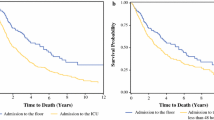
The mortality rate in the entire cohort was 1.8%, and 53 patients (31.5%) experienced a grade 3 or 4 complication. After implementation of ERAS, the median hospital LOS decreased (7.9 vs 10.0 days; p = 0.015), whereas readmission rates remained the same (16.2% vs 13.6%; p = 0.635). Similarly, the post-ERAS group had fewer grade ≥ 3 complications (23.7% vs 38.6; p = 0.04) and a lower AKI (7.5% vs 18.2%; p = 0.04) (Table 3).
Multivariable Analysis
For a better understanding of the impact that ERAS implementation has on the occurrence of grades 3 and 4 morbidity and AKI, multivariable linear regression analyses were performed. Clinically relevant variables were selected to construct both models, and the independent impact of ERAS was estimated. An increase in grades 3 and 4 morbidity was associated with operative time (odds ratio [OR] 1.005), EBL (OR 1.002) and intraoperative IVF (OR 1.158). Notably, implementation of ERAS emerged as a protective factor for grades 3 and 4 morbidity (OR 0.48; 95% confidence interval [CI] 0.24–0.97) (Table 4).
Similarly, the impact of ERAS implementation on AKI rates was estimated. The multivariable analysis identified an association of PCI (OR 1.105; 95% CI 1.023–1.194), EBL (OR 1.002; 95% CI 1.000–1.004), and use of cisplatin in perfusate (OR 5.518; 95% CI 1.292–23.556) with an increase AKI rates. Implementation of ERAS did not affect AKI occurrence. Given the known effect of cisplatin on AKI, the pre- and post-ERAS outcomes for the patients not receiving cisplatin in perfusate were compared. For 65 of the pre-ERAS patients and 52 of the post-ERAS patients, LOS remained lower after ERAS implementation (7.0 vs 10.0 days; p = 0.022) (Table 5).
Discussion
Although ERAS programs have consistently been shown to improve short-term outcomes for a variety of surgical procedures, its effect on patients undergoing CRS-HIPEC is less well established. In this retrospective study of a prospectively maintained database that included 168 patients undergoing CRS/HIPEC, implementation of a comprehensive ERAS program was associated with a significant decrease in LOS and 30-day morbidity without having an adverse impact on the rates of AKI or readmission. These results confirm the safety of ERAS after CRS-HIPEC and further suggest that ERAS may lessen morbidity in this population.
The reported risk of AKI after CRS-HIPEC ranges from 4 to 40%.35,36,37,38,39 This risk is related to the HIPEC chemotherapy agent used, especially cisplatin, and correlates with an increased risk for major morbidity.26,40 The mechanism of cisplatin nephrotoxicity is multifactorial. It is both filtered and actively taken up into the cells lining the proximal tubules, causing DNA crosslinking in both the nucleus and the mitochondria that leads to apoptosis.41 As part of ERAS protocols is decreased, there may be concern that perioperative fluid will increase this risk of AKI. However, prior studies investigating restrictive fluid therapy alone did not see an increase in the rate of AKI or the comprehensive complication index that encompasses it.42,43 This study evaluated the rate of AKI as a secondary end point and found a significant reduction from 18.2 to 7.5% when all chemotherapy agents were included after implementation of ERAS.
Because the rate of AKI varies dramatically between chemotherapy agents, the current study also evaluated AKI with cisplatin excluded from the analysis. In this group excluding patients who received cisplatin, 9.2% had an AKI similar to that after implementation of ERAS, indicating that patients receiving cisplatin had the greatest benefit. Supporting this conclusion, the multivariate analysis found cisplatin administration strongly associated with AKI before ERAS but not afterward. Several aspects of ERAS may contribute to this improvement. Preoperatively, decreased NPO time may improve the patient’s baseline hydration status. In the operating room, increased hemodynamic control provided by intraoperative goal-directed therapy may increase renal perfusion, whereas use of sodium thiosulfate and magnesium blunts the nephrotoxic effect of cisplatin.
A literature review identified four additional studies on the topic.22,23,24,25 To date, the current study represents the largest series to investigate the use of an ERAS protocol for patients undergoing CRS-HIPEC. Webb et al.25 analyzed the primary end points of 30-day morbidity and mortality as well as the secondary end points of 30-day readmission and LOS, finding a significant reduction in morbidity and mortality, from 33 to 21%, as well as a decreased median LOS, from 13.1 to 9.5 days, for their patients undergoing open HIPEC.
Duzgun et al.22 found a decrease from 15 to 8% in morbidity, from 2.3 to 1.1 days in ICU stay, from 10 to 7 days in LOS, and from $3300 to $2100 in cost after implementing their ERAS protocol, which also included a restrictive IVF approach and perhaps a slightly sicker ERAS group based on PCI, nutritional risk score, and age. Siddharthan et al.24 found a reduction in LOS from 11 to 7 days, but found no differences in morbidity or mortality. Lu et al.23 found a decrease in LOS and postoperative ICU admissions, but after considering AKI and ARF as primary end points, did not find any incident of either in their study with 31 patients using MM-C, which is less likely to cause AKI than platinum-based agents.40
This study had several important limitations. First, its retrospective nature was indeed susceptible to selection bias. Although this was minimized through prospective data collection and by inclusion of all HIPEC operations during the study period, it is possible that for patients, this may be inadequate. Second, the “before-and-after” design of the studies also may be viewed as problematic because the ERAS group possibly benefited from this additional experience of both the surgery teams and the system as a whole. Third, adherence to ERAS was not reported in our dataset, and conclusions regarding the exact effect of the protocol were difficult to discern. Finally, it should be noted that our findings may not be generalizable because the data were from a high-volume single institution and included two surgeons in their learning curve.
Due to the historic high morbidity associated with CRS-HIPEC, surgeons may be hesitant to implement a full ERAS protocol compared with more conservative methods. This is not dissimilar from the resistance with which ERAS was met in the past, including its use in colorectal surgery, for which it was adopted early.19 This mentality also likely plays a role in the reluctance of outside physicians to refer patients that could benefit from the procedure.16
The results of this study add to a growing body of evidence that an ERAS protocol is feasible for patients undergoing CRS-HIPEC and may offer a significant improvement in outcomes, as observed for other major surgeries. Decreasing complication rates and LOS could assuage some of these concerns regarding indication of CRS-HIPEC procedures for appropriately selected patients. Furthermore, the Chicago Consensus Working Group17 has issued quality standards for centers performing HIPEC, and ERAS might help centers reach the goals outlined, which include LOS and complication rate.
To help elucidate which interventions are most effective, more data would be beneficial, and a prospective trial would help to eliminate the temporal factor that is a common limitation of the evidence to date.
Change history
19 February 2021
A Correction to this paper has been published: https://doi.org/10.1245/s10434-021-09737-x
References
Paul Olson TJ, Pinkerton C, Brasel KJ, Schwarze ML. Palliative surgery for malignant bowel obstruction from carcinomatosis: a systematic review. JAMA Surg. 2014;149:383–92.
Tseng J, Bryan DS, Poli E, Sharma M, Polite BN, Turaga KK. Under-representation of peritoneal metastases in published clinical trials of metastatic colorectal cancer. Lancet Oncol. 2017;18:711–2.
Bonnot PE, Piessen G, Kepenekian V, et al. Cytoreductive surgery with or without hyperthermic intraperitoneal chemotherapy for gastric cancer with peritoneal metastases (CYTO-CHIP study): a propensity score analysis. J Clin Oncol. 2019;37:2028–40.
Votanopoulos KI, Shen P, Skardal A, Levine EA. Peritoneal metastases from appendiceal cancer. Surg Oncol Clin North Am. 2018;27:551–61.
van Driel WJ, Koole SN, Sikorska K, et al. Hyperthermic intraperitoneal chemotherapy in ovarian cancer. N Engl J Med. 2018;378:230–40.
Cashin PH, Mahteme H, Spang N, et al. Cytoreductive surgery and intraperitoneal chemotherapy versus systemic chemotherapy for colorectal peritoneal metastases: a randomised trial. Eur J Cancer. 2016;53:155–62.
Spiliotis J, Halkia E, Lianos E, et al. Cytoreductive surgery and HIPEC in recurrent epithelial ovarian cancer: a prospective randomized phase III study. Ann Surg Oncol. 2015;22:1570–5.
Yan TD, Deraco M, Baratti D, et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for malignant peritoneal mesothelioma: multi-institutional experience. J Clin Oncol. 2009;27:6237–42.
Sugarbaker PH. Peritonectomy procedures. Ann Surg. 1995;221:29–42.
Sheshadri DB, Chakravarthy MR. Anaesthetic considerations in the perioperative management of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Indian J Surg Oncol. 2016;7:236–43.
Webb CA, Weyker PD, Moitra VK, Raker RK. An overview of cytoreductive surgery and hyperthermic intraperitoneal chemoperfusion for the anesthesiologist. Anesth Analg. 2013;116:924–31.
Kecmanovic DM, Pavlov MJ, Ceranic MS, Sepetkovski AV, Kovacevic PA, Stamenkovic AB. Treatment of peritoneal carcinomatosis from colorectal cancer by cytoreductive surgery and hyperthermic perioperative intraperitoneal chemotherapy. Eur J Surg Oncol. 2005;31:147–52.
Jacquet P, Stephens AD, Averbach AM, et al. Analysis of morbidity and mortality in 60 patients with peritoneal carcinomatosis treated by cytoreductive surgery and heated intraoperative intraperitoneal chemotherapy. Cancer. 1996;77:2622–9.
Ellis RJ, Schlick CJR, Yang AD, Barber EL, Bilimoria KY, Merkow RP. Utilization and treatment patterns of cytoreduction surgery and intraperitoneal chemotherapy in the United States. Ann Surg Oncol. 2020;27:214–21.
Gani F, Conca-Cheng AM, Nettles B, Ahuja N, Johnston FM. Trends in outcomes after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. J Surg Res. 2019;234:240–8.
Foster JM, Sleightholm R, Patel A, et al. Morbidity and mortality rates following cytoreductive surgery combined with hyperthermic intraperitoneal chemotherapy compared with other high-risk surgical oncology procedures. JAMA Netw Open. 2019;2:e186847.
Chicago Consensus Working G. The Chicago Consensus on Peritoneal Surface Malignancies: Standards. Ann Surg Oncol. 2020;27:1743–52.
Kehlet H, Mogensen T. Hospital stay of 2 days after open sigmoidectomy with a multimodal rehabilitation programme. Br J Surg. 1999;86:227–30.
Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg. 2017;152:292–8.
Hendrix RJ, Lambert LA. ASO Author Reflections: intraoperative fluid restriction during CRS-HIPEC–less is more. Ann Surg Oncol. 2019;26(Suppl 3):575–6.
Osseis M, Weyrech J, Gayat E, et al. Epidural analgesia combined with a comprehensive physiotherapy program after cytoreductive surgery and HIPEC is associated with enhanced postoperative recovery and reduces intensive care unit stay: a retrospective study of 124 patients. Eur J Surg Oncol. 2016;42:1938–43.
Duzgun O. Evaluation of enhanced recovery after following a surgical protocol for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis. Med Arch. 2019;73:331–7.
Lu PW, Fields AC, Shabat G, et al. Cytoreductive surgery and HIPEC in an enhanced recovery after surgery program: a feasibility study. J Surg Res. 2020;247:59–65.
Siddharthan R, Dewey E, Billingsley K, Gilbert E, Tsikitis VL. Feasibility and benefits of an enhanced recovery after surgery protocol for patients undergoing cytoreductive surgery and heated intraperitoneal chemotharpy: a single-institution experience. Am J Surg. 2020;219:1073–5.
Webb C, Day R, Velazco CS, et al. Implementation of an enhanced recovery after surgery (ERAS) program is associated with improved outcomes in patients undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 2020;27:303–12.
Naffouje SA, Tulla KA, Chorley R, Armstrong N, Salti GI. Acute kidney injury increases the rate of major morbidities in cytoreductive surgery and HIPEC. Ann Med Surg London. 2018;35:163–8.
Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–55.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8.
Mohile SG, Dale W, Somerfield MR, Hurria A. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology summary. J Oncol Pract. 2018;14:442–6.
American Society of Anesthesiologists C. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters. Anesthesiology. 2011;114:495–511.
Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 2017;152:691–7.
McCarthy GC, Megalla SA, Habib AS. Impact of intravenous lidocaine infusion on postoperative analgesia and recovery from surgery: a systematic review of randomized controlled trials. Drugs. 2010;70:1149–63.
Warren JA, Stoddard C, Hunter AL, et al. Effect of multimodal analgesia on opioid use after open ventral hernia repair. J Gastrointest Surg. 2017;21:1692–9.
Torgeson M, Kileny J, Pfeifer C, Narkiewicz L, Obi S. Conventional epidural vs transversus abdominis plane block with liposomal bupivacaine: a randomized trial in colorectal surgery. J Am Coll Surg. 2018;227:78–83.
Cata JP, Zavala AM, Van Meter A, et al. Identification of risk factors associated with postoperative acute kidney injury after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy: a retrospective study. Int J Hyperthermia. 2018;34:538–44.
Dagel T, Misirlioglu S, Tanju S, et al. Hyperthermic intraperitonal chemotherapy is an independent risk factor for development of acute kidney injury. J BUON. 2018;23:1528–33.
Hakeam HA, Breakiet M, Azzam A, Nadeem A, Amin T. The incidence of cisplatin nephrotoxicity post hyperthermic intraperitoneal chemotherapy (HIPEC) and cytoreductive surgery. Ren Fail. 2014;36:1486–91.
Sin EI, Chia CS, Tan GHC, Soo KC, Teo MC. Acute kidney injury in ovarian cancer patients undergoing cytoreductive surgery and hyperthermic intra-peritoneal chemotherapy. Int J Hyperthermia. 2017;33:690–5.
Ye J, Ren Y, Wei Z, et al. Nephrotoxicity and long-term survival investigations for patients with peritoneal carcinomatosis using hyperthermic intraperitoneal chemotherapy with cisplatin: a retrospective cohort study. Surg Oncol. 2018;27:456–61.
Tan GHC, Shannon NB, Chia CS, Soo KC, Teo MCC. Platinum agents and mitomycin C-specific complications in cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC). Int J Hyperthermia. 2018;34:595–600.
Manohar S, Leung N. Cisplatin nephrotoxicity: a review of the literature. J Nephrol. 2018;31:15–25.
Eng OS, Dumitra S, O’Leary M, et al. Association of fluid administration with morbidity in cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. JAMA Surg. 2017;152:1156–60.
Hendrix RJ, Damle A, Williams C, et al. Restrictive intraoperative fluid therapy is associated with decreased morbidity and length of stay following hyperthermic intraperitoneal chemoperfusion. Ann Surg Oncol. 2019;26:490–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
White, B., Dahdaleh, F., Naffouje, S.A. et al. Impact of Enhanced Recovery After Surgery on Postoperative Outcomes for Patients Undergoing Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy. Ann Surg Oncol 28, 5265–5272 (2021). https://doi.org/10.1245/s10434-020-09476-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09476-5