Abstract
Introduction
Cardiopulmonary exercise testing (CPET) is an objective method of assessing functional capacity to meet the metabolic demands of surgery and has been adopted as a preoperative risk-stratification tool for patients undergoing major procedures. The two main measures are the peak rate of oxygen uptake during exercise (\(\dot{{\text{V}}}\)O2peak) and anaerobic threshold (AT), the point at which anaerobic metabolism exceeds aerobic metabolism during exercise. This systematic review and meta-analysis evaluates the predictive value of CPET for patients undergoing oesophagectomy.
Methods
A systematic literature search was conducted in databases of CINAHL, Cochrane Library, EMBASE, MEDLINE, PubMed, and Scopus to identify studies that examined associations between preoperative CPET variables and postoperative outcomes following oesophagectomy. Results were presented as standardised mean difference (SMD) with 95% confidence interval.
Results
Seven studies were included in this review. Preoperative \(\dot{{\text{V}}}\)O2peak moderately correlated with cardiopulmonary complications [SMD = − 0.43; 95% confidence interval (CI) − 0.77 to − 0.09; p = 0.013; I2 = 80.4%], unplanned ICU admissions (SMD = − 0.34; 95% CI − 0.60 to − 0.08; p = 0.011; I2 = 0.0%), and 1-year survival (SMD = 0.31; 95% CI 0.02–0.61; p = 0.045; I2 = 0.0%). Preoperative AT values moderately correlated with unplanned ICU admissions (SMD = − 0.34; 95% CI − 0.61 to − 0.07; p = 0.014; I2 = 0.0%), and 1-year survival (SMD = 0.34; 95% CI 0.00–0.68; p = 0.049; I2 = 7.4%). Neither \(\dot{{\text{V}}}\)O2peak nor AT demonstrated prognostic value for noncardiopulmonary complications.
Conclusions
\(\dot{{\text{V}}}\)O2peak and AT, where measured by preoperative CPET testing, are inversely associated with postoperative cardiopulmonary complications, unplanned ICU admissions, and 1-year survival following oesophagectomy. This meta-analysis was not able to identify an absolute cutoff value for CPET variables to discriminate between patients of varying levels of operative risk.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Oesophageal cancer is the seventh most common malignancy and the sixth leading cause of cancer-related death globally.1 The current standard of care for resectable oesophageal cancer involves multimodal therapy, combining perioperative chemotherapy or chemoradiotherapy with surgery.2,3 While surgery is the mainstay of curative treatment, even when performed in high-volume centres, oesophagectomy is associated with a high morbidity of 17–74% and mortality in up to 3–5%.4,5,6,–7
Morbidity following oesophageal resection is in part due to the substantial iatrogenic trauma of the surgery but also is related to the overall fitness of patients undergoing treatment.8 Clinicians therefore consider physical health status, particularly cardiopulmonary fitness, as a key determinant of suitability for such a major operation.9
Accurate preoperative risk stratification is important to predict and manage postoesophagectomy outcomes.10 Risk stratification plays an important role in patient selection for surgery and guiding preoperative optimisation.11 While several prognostic tools have been developed to predict adverse events after major surgery, not all of these have demonstrated good discriminative ability.12,13,14,15,–16
Cardiopulmonary exercise testing (CPET) is an objective method of assessing physical fitness based on cardiopulmonary function.17 This test measures the patient’s peak oxygen uptake (\(\dot{{\text{V}}}\)O2peak) as well as their sustainable aerobic activity, defined as the physiological point at which anaerobic metabolism exceeds aerobic metabolism (AT). In theory, CPET determines the ability to meet the metabolic demands of surgery based on recording oxygen delivery and utilisation in response to a graded increase in exercise intensity.18 Previous systematic reviews have demonstrated that a low \(\dot{{\text{V}}}\)O2peak and AT value correlate strongly with increased morbidity and mortality risk across other surgical disciplines.11,19,20 However, despite a growing number of centres implementing CPET before planning an oesophageal resection, its predictive value for postoperative outcomes in this setting has not yet been validated in a systematic review.
The objective of this review is to measure the predictive value of \(\dot{{\text{V}}}\)O2peak and AT as determined by CPET in the prediction of postoperative complications, unplanned intensive care unit (ICU) admissions, and 1-year survival in patients undergoing oesophagectomy.
Methods
Search Strategy
A review of the literature was conducted in October 2019 to search for articles relevant to the association between preoperative CPET variables, \(\dot{{\text{V}}}\)O2peak and AT, and postoperative outcomes following oesophagectomy. The CINAHL, Cochrane Library, EMBASE, MEDLINE, PubMed, and Scopus databases were included. The following key search terms were applied in multiple different combinations: “Cardiopulmonary exercise testing”; “CPEX”; “CPET”; “\(\dot{{\text{V}}}\)O2peak”; “Anaerobic threshold”; “Esophagectomy”; and “Oesophagectomy.” A complete search strategy for a single database defined with all keywords and subject headings is included (Supplementary data, Appendix S1). A manual search was performed on references of relevant published studies. Screening of articles and their selection was performed by two authors (JS, HS).
Eligibility Criteria
For inclusion in the review, studies were required to meet the following selection criteria: (a) involve subjects undergoing CPET before an oesophagectomy; (b) measurement of outcomes of interest, including both cardiopulmonary complications and noncardiopulmonary complications, unplanned ICU admissions, and 1-year survival; (c) report on comparisons between preoperative CPET variables and outcomes of interest; (d) be an original paper with independent data; and (e) be published as full-text articles in a peer-reviewed journal in English. Studies were excluded according to the following criteria: (a) clinical data unavailable for the study; (b) research data repeated with other studies; and (c) editorial letters and conference abstracts. No study design restriction was used.
Critical Appraisal
Two authors (JS, HS) independently assessed the quality of the methodology and the risk of bias for eligible studies using the Quality in Prognosis Studies (QUIPS) tool,21 with any discrepancies resolved with discussion and consensus. This scale assesses the quality of prognostic studies across six domains: study participation, attrition, prognostic factor measurement, outcome measurement, study confounding, and statistical analysis and reporting.
Data Extraction
Data extraction was conducted by the lead investigator (JS). The recorded data included study design, patient characteristics, method of CPET, type of procedure, mean values for \(\dot{{\text{V}}}\)O2peak and AT, as well as the incidence for any outcomes of interest. Outcomes of interest included cardiopulmonary complications, noncardiopulmonary complications, unplanned ICU admissions, and survival at 1 year postoperatively. Authors were contacted to obtain an original data set to improve the uniformity of the results.
Statistical Analysis
Data were analysed using an inverse-variance random-effects model. We decided a priori to use the random-effects model for meta-analyses because we assumed clinical heterogeneity across the included studies. Results were presented as standardised mean difference (SMD) with 95% confidence interval and described using a forest plot. SMD is used as a standardisation statistic that accounts for the variable methods of reporting the same outcome across the multiple studies. This expresses the size of the intervention effect in each study relative to the variability observed in that study. Where possible, individual data for included studies was analysed to ensure normal distribution of data using histograms and Quantile–Quantile (Q–Q) plots. We assessed heterogeneity between studies by calculating tau-squared (τ2) and I-squared (I2). Tau-squared indicated the variance of the true effect sizes and the I2 statistic indicates the proportion (as expressed through percentage) of variance remaining if sampling error is removed. Values of 24%, 50%, and 75% could be considered low, moderate, and high, respectively. All calculations were performed using Stata 15.1 (Stata Corporation, College Station, TX).
Standards of Reporting
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.22 The review protocol was registered in the PROSPERO international prospective register of systematic reviews (CRD42019147102) on September 11, 2019.
Results
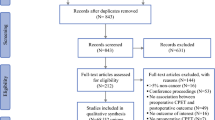
The search strategy yielded 410 studies, and after the removal of 58 duplicates, and exclusion of 204 articles based on abstract screening, 148 full-text publications were reviewed (Fig. 1). A total of 7 consecutive cohort publications, with a combined sample size of 912 patients undergoing oesophagectomy, were deemed suitable for the qualitative analysis (Table 1).23,24,25,26,27,28,–29 One study was conducted in Japan, whereas the remainder were undertaken in the United Kingdom. Corresponding authors of three studies were able to provide individual patient data.27,28,–29 Patel et al. also were able to provide an updated dataset of an additional 43 patients that had been analysed since their original publication, which has been included in this analysis.27
All seven papers studied the role of CPET for preoperative risk assessment in patients undergoing oesophagectomy. One study combined this cohort with patients also undergoing gastrectomy, and to account for this, a sensitivity analysis was performed to assess for any discernible effect when this study was excluded.26 CPET variables, AT and \(\dot{{\text{V}}}\)O2peak, were reported in all studies, whereas the ventilatory equivalents for carbon dioxide (\(\dot{{\text{V}}}\)E/\(\dot{{\text{V}}}\)CO2) was only measured in two studies and therefore not included in this analysis. Across all seven studies, CPET was performed with a stationary cycle ergometer and involved an incremental exercise protocol until the patient’s maximum tolerated level was reached. In two studies,25,27\(\dot{{\text{V}}}\)O2peak was determined from the highest or average value achieved in the final 30 s of the test. Another two studies defined it as the maximum \(\dot{{\text{V}}}\)O2peak value during the entire exercise program 23,26; and three studies did not specifically report how this was value was derived.24,28,29 The value for AT was determined using the V-slope method in five studies,23,24,–25,27,28,30 whereas two studies did not detail how this value was achieved.26,29 While all other studies presented values for CPET variables in standard units of mL/kg/min, Nagamatsu et al. divided these values by the square meters (m2) of body surface area to minimise any variability due to difference in physiques.23 CPET was undertaken preoperatively in all studies; four of them reported performing the test at the time of diagnosis prior starting neoadjuvant therapy,24,26,28,31 one study performed the test immediately prior to surgery and after the completion of any neoadjuvant systemic therapy,29 and two studies did not disclose the specific timing of CPET.23,25
Mean values for \(\dot{{\text{V}}}\)O2peak and AT are presented for each study outcome in Table 2. All outcomes were defined from the time of surgery until follow up or death. The seven studies used a variety of classifications for defining complications, including the Common Terminology Criteria for Adverse Events,24,26,32 Clavien-Dindo classification,25,27,33,34 Accordion score,28,35 or otherwise a self-defined measure of adverse cardiac or respiratory events dependent on whether treatment was required.23 Where overall complications were recorded, these were further divided by their organ system to be defined as cardiopulmonary or noncardiopulmonary. One study did not detail the definition or classification system for recording complications.29 Given that standard practice is for esophagectomy patients to be managed in critical care postoperatively as Level 2 or 3 care, unplanned ICU admissions were defined as a return to ICU after discharge from critical care. The quality of included studies was assessed using the QUIPS tool (Table 3). All studies were considered to be of good quality; however, there was moderate risk of confounding bias in a majority of them.
The studies included in the meta-analysis contain large sample sizes per group and therefore can assume normal distribution based on the Central Limit Theorem.36 For the three original datasets provided,27,28,–29 histogram assessments approximating a normal curve and Q–Q plots demonstrate data points relatively close to the straight line, indicative of normality (Supplementary data, Appendix S2).
Cardiopulmonary Complications
The results from seven studies were pooled to examine the relationship between \(\dot{{\text{V}}}\)O2peak levels and the incidence of cardiopulmonary complications (Fig. 2).23,24,25,26,27,28,–29 Mean \(\dot{{\text{V}}}\)O2peak values in those that developed cardiopulmonary complications was significantly lower compared with those that did not develop cardiopulmonary complications (SMD = − 0.43; 95% CI − 0.77 to − 0.09; test for overall effect: z = − 2.476; p = 0.013), although significant heterogeneity was noted (I2 = 80.4%; τ2 = 0.19). Because the study from Moyes et al. included results from gastrectomy patients as well as oesophagectomy patients, a sensitivity analysis was conducted where the model was conducted again without this study. The results were very similar to those found from the model including all studies (SMD = − 0.45; 95% CI − 0.84 to − 0.05; test for overall effect: z = − 2.206; p = 0.027; I2 = 83.6%; τ2 = 0.19). Mean AT levels from six studies were pooled to determine the summative effect of AT levels and cardiopulmonary complications (Fig. 2).23,24,–25,27,28,–29 The mean value for AT in those that developed cardiopulmonary complications was not found to be significantly different compared with those that did not develop cardiopulmonary complications (SMD = − 0.17; 95% CI − 0.42 to 0.09; test for overall effect: z = − 1.248; p = 0.212), with moderate heterogeneity detected (I2 = 62.0%; τ2 = 0.06).
Noncardiopulmonary Complications
As demonstrated from the five studies in Fig. 3,24,25,27,28,–29\(\dot{{\text{V}}}\)O2peak in patients who developed noncardiopulmonary complications was not significantly different to those who did not develop noncardiopulmonary complications (SMD = − 0.02; 95% CI − 0.18 to 0.13; test for overall effect: z = − 0.303; p = 0.762; I2 = 0.0%; τ2 = 0.0). This same group of studies were used to compare AT levels in patients that did and did not develop noncardiopulmonary complications.24,25,27,28,–29 AT was not significantly different between either group (SMD = 0.01; 95% CI − 0.15 to 0.17; test for overall effect: z = 0.107; p = 0.915; I2 = 0.0%; τ2 = 0.0).
Unplanned Return to ICU
Figure 4 shows that in three studies \(\dot{{\text{V}}}\)O2peak was significantly lower in those that required an unplanned admission to ICU compared with those that did not (SMD = − 0.34; 95% CI − 0.60 to − 0.08; test for overall effect: z = − 2.555; p = 0.011; I2 = 0.0%; τ2 = 0.0).24,27,28 Similarly, these studies also showed that AT levels in patients that did have an unplanned return to ICU were significantly lower compared with their counterparts (SMD = − 0.34; 95% CI − 0.61 to − 0.07; test for overall effect: z = − 2.543; p = 0.014; I2 = 0.0%; τ2 = 0.0).24,27,28 No heterogeneity was determined in either test for this outcome.
One-Year Survival
A survival assessment was also performed by comparing preoperative CPET variables in patients that were alive at 1-year post-oesophagectomy. While other studies measured survival as an outcome, this was not reported in their final publication due to the low number of mortality events available for analysis.24,25 As a result, only three studies with individual patient data provided by authors were able to be assessed.27,28,–29 Presented in Fig. 5, \(\dot{{\text{V}}}\)O2peak levels in patients that survived until one year postoperatively were significantly higher than those who had not survived to this point (SMD = 0.31; 95% CI 0.02–0.61; test for overall effect: z = 2.003; p = 0.045), with no heterogeneity present (I2 = 0.0%; τ2 = 0.0). The association between survival and AT followed a similar trend; AT in those who had survived was significantly higher compared with those that had mortality within 1-year postoperatively (SMD = 0.34; 95% CI 0.00–0.68; test for overall effect: z = 1.969; p = 0.049), with low heterogeneity noted (I2 = 7.4%; τ2 = 0.01).
Discussion
Preoperative CPET is a dynamic assessment of functional capacity that measures gas exchange during exercise.37 This evaluates the integrated function of cardiac, circulatory, respiratory, and metabolic systems during physiological stress.38 Its role was originally defined in cardiothoracic surgery but is now being implemented in many centres as part of a risk stratification tool before undergoing major abdominal and thoracic surgery.
The physiological principle underpinning the association between CPET and post-oesophagectomy outcomes is that surgery places a significant burden on the patient’s cardiopulmonary reserve. Oxygen demand increases by 40–50% in the early postoperative period, requiring an increase in ventilation and cardiac output.39 Patients who are unable to compensate for this demand are thought to be at an increased risk of cardiopulmonary complications.40,41 Preoperative measurement of cardiopulmonary reserve may help to stratify how well patients tolerate the physiological insult of an oesophageal resection and reconstruction. The two key CPET variables in our study assess the cardiopulmonary reserve through recording the patient’s efficiency in delivering oxygen from the environment to cellular mitochondria (\(\dot{{\text{V}}}\)O2peak) and the ability to cope with increased peripheral oxygen requirements without entering a state of anaerobic metabolism (AT).19 While these two variables may correlate with one another, they also are distinct measures as \(\dot{{\text{V}}}\)O2peak relates to performance during maximum activity and AT relates to endurance during sustained nonmaximum activity.42
This meta-analysis demonstrates that with respect to patients undergoing oesophagectomy, preoperative CPET variables correlate with postoperative cardiopulmonary complications, unplanned critical care admissions, and survival at 1 year after surgery.
Cardiopulmonary-specific complications are common following oesophagectomy in part due to the physiological stress of surgery on the patient’s cardiopulmonary reserve. The Esophageal Complications Consensus Group (ECCG) reported the postoperative incidence of cardiac and pulmonary complications as 16.8% and 27.8%, respectively.7 The most common of these complications include new-onset arrhythmias and pneumonias, often occurring in combination with each other.7 The predictive value of CPET for cardiopulmonary complications demonstrated by this meta-analysis is consistent with findings using CPET in other surgical disciplines. A systematic review on the role of CPET in hepato-pancreatico biliary surgery demonstrated a strong correlation between a low AT value and increased incidence of complications, although this did not specifically evaluate cardiopulmonary complications.43 There was limited data available in the included studies to appropriately evaluate the effect of \(\dot{{\text{V}}}\)O2peak on postoperative morbidity. A systematic review and quantitative analysis of colorectal cancer surgery patients undergoing preoperative CPET identified low anaerobic threshold as predictive of cardiovascular and pulmonary complications.44 A low \(\dot{{\text{V}}}\)O2peak was able to predict for postoperative complications in general; however, no analysis was performed with respect to cardiopulmonary complications.
Postoperative cardiopulmonary complications also are the largest factor contributing to unplanned ICU admissions following oesophagectomy.45,46 This is likely to account for the relationship between CPET variables and unplanned ICU admissions. The findings of the present analysis also may suggest that CPET variables may be an indicator of patients’ physiological capacity for tolerating complications and therefore predict the likelihood of returning to ICU. Prior reviews in hepato-pancreatico biliary surgery and colorectal surgery have failed to report on the prognostic value CPET-derived metrics and unplanned ICU admissions. However, a prospective consecutive series study from Older et al. evaluating patients undergoing major intra-abdominal surgery validated AT as a robust predictor of whether patients may be safely managed on the ward compared with requiring a critical care bed.47 In a recent survey of centres in the United Kingdom with CPET facilities, many report already using the results to determine allocation of appropriate postoperative level of care across all surgical disciplines.48
The ability for \(\dot{{\text{V}}}\)O2peak and AT to prognosticate survival also is partially explained by the fact that cardiopulmonary complications account for up to 70% of mortality events after oesophagectomy procedures.49 In comparison, both \(\dot{{\text{V}}}\)O2peak and AT were found in a previous systematic review to be beneficial in predicting mortality for patients undergoing hepatic resection for cancer.50 With regards to pancreatic cancer surgery, preoperative AT exhibited no significant relationship with mortality, and \(\dot{{\text{V}}}\)O2peak was not assessed in any available studies.50 A meta-analysis assessing CPET in patients undergoing surgery for colorectal cancer was unable to determine its efficacy in predicting mortality due to the low number of events.44 Although poor physical status, as represented by \(\dot{{\text{V}}}\)O2peak and AT, are directly linked with poor survival postoperatively,51 recognising this relationship between CPET and mortality may have reduced relevance given the low incidence of deaths.
CPET is a risk prediction tool that supplements preoperative clinical assessment, because it identifies patients who may require further optimization or prehabilitation in the form of inspiratory muscle training and endurance exercises and also may support sensible decision making for patients who should avoid oesophageal surgery if their operative risk exceeds potential benefit from surgery.52,53 Several international guidelines have endorsed the implementation of CPET as a preoperative stratification tool and have provided recommendations for its appropriate use and interpretation across all surgical disciplines.54,55,56,–57
Despite the predictive value of CPET, several shortcomings limit the universal application as part of routine workup before oesophagectomy. First, no single benchmark value is able to delineate between positive and negative outcomes following oesophagectomy. In this meta-analysis, this could not be defined due to the lack of individual patient data available for a pooled analysis, as well as the lack of consistent thresholds between studies in defining an abnormal CPET result. The cutoff values for defining high-risk patients from articles in the present review include an AT value of 9–11 mL/kg/min and \(\dot{{\text{V}}}\)O2peak value of 14 mL/kg/min; however, these values were selected after use in nonsurgical studies.58,59 To improve the clinical applicability of CPET to surgical patients, future research should define an optimal decision threshold for CPET variables based on a receiver operating characteristic curve analysis. While other articles across all surgical disciplines have adopted an arbitrary cutoff of 11 mL/kg/min for AT and 14 mL/kg/min for \(\dot{{\text{V}}}\)O2peak to predict favourable outcomes following surgery, there is no definitive evidence that these individual values are useful in discriminating high-risk from low-risk patients.9,24,26,60,61
Second, as neoadjuvant therapy frequently forms part of the treatment paradigm for oesophageal cancer, especially for patients with locally advanced disease,2,62,63 this may be a potential confounder for the clinical application of CPET. Previous studies have demonstrated that systemic treatment in this cohort diminishes preoperative cardiopulmonary reserve with a significant reduction in \(\dot{{\text{V}}}\)O2peak and AT in patients who underwent neoadjuvant chemotherapy.64,65,–66 With regards to the seven studies included in this review, CPET was performed at variable timepoints in the preoperative period, either before or after neoadjuvant chemotherapy. This emphasises the importance of performing CPET at an appropriate and standardised time in the patient’s treatment pathway.
Finally, it also is important to consider that performing this test is relatively time consuming and expensive.67 This is due to need for equipment and trained staff who can perform the test as well as interpret the results. These costs should be weighed against the potential savings of reducing complications in this cohort.68 As a result of these expenses, there is commonly poor access to CPET facilities outside of high-volume centres.48
The results of this study should be interpreted in the setting of several limitations. Most of the studies were from centres in the United Kingdom, and as such, these population differences may be a potential source of selection bias. This may restrict the external validity of our findings to other centres worldwide. Four of the included studies were retrospective in and thus subject to potential observational bias in the data collection process. All articles did provide strict guidelines for their data collection process in an attempt to minimise this bias. There was variation in the classification method for postoperative complications between studies, and this also may contribute to the risk of bias in comparing these studies. This meta-analysis yielded high heterogeneity with regards to evaluating cardiopulmonary complications, and this may have been due to the differences in the study cohorts relating to demographics, comorbidities, and operative approach. This was accommodated for through the use of a random effects model. While \(\dot{{\text{V}}}\)O2peak and AT are the emphasis of CPET research studies, CPET also involves the routine collection of other cardiorespiratory variables—the ventilatory equivalents for oxygen (\(\dot{{\text{V}}}\)E/\(\dot{{\text{V}}}\)O2) and carbon dioxide (\(\dot{{\text{V}}}\)E/\(\dot{{\text{V}}}\)CO2)—and spirometry variables. A future analysis that incorporates a combination of these variables to determine a patient’s fitness for surgery may be more reliable than solely assessing \(\dot{{\text{V}}}\)O2peak and AT.
Conclusions
Preoperative CPET is a useful predictor of adverse postoperative outcomes following oesophagectomy, including cardiopulmonary complications, unplanned ICU admissions, and 1-year mortality. CPET can play a role as part of multidisciplinary preoperative assessment and optimisation before oesophagectomy. The clinical usefulness of CPET testing is limited by the lack of a defined cutoff value for \(\dot{{\text{V}}}\)O2peak and AT to delineate between high-risk and low-risk patients.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20.
van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366(22):2074–84.
Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. Ne Engl J Med. 2011;364(22):2128–37.
Markar S, Gronnier C, Duhamel A, Bigourdan JM, Badic B, du Rieu MC, et al. Pattern of postoperative mortality after esophageal cancer resection according to center volume: results from a large european multicenter study. Ann Surg Oncol. 2015;22(8):2615–23.
Lapar DJ, Stukenborg GJ, Lau CL, Jones DR, Kozower BD. Differences in reported esophageal cancer resection outcomes between national clinical and administrative databases. J Thorac Cardiovasc Surg. 2012;144(5):1152–7.
Low DE, Kuppusamy MK, Alderson D, Cecconello I, Chang AC, Darling G, et al. Benchmarking complications associated with esophagectomy. Ann Surg 2019;269(2):291–8.
Feeney C, Hussey J, Carey M, Reynolds JV. Assessment of physical fitness for esophageal surgery, and targeting interventions to optimize outcomes. Dis Esophagus. 2010;23(7):529–39.
Older P, Hall A. Cardiopulmonary exercise testing in preoperative risk assessment and patient management. Br J Anaesth. 2017;119(4):837–8.
Snowden CP, Prentis J, Jacques B, Anderson H, Manas D, Jones D, et al. Cardiorespiratory fitness predicts mortality and hospital length of stay after major elective surgery in older people. Ann Surg. 2013;257(6):999–1004.
Hennis PJ, Meale PM, Grocott MP. Cardiopulmonary exercise testing for the evaluation of perioperative risk in non-cardiopulmonary surgery. Postgrad Med J. 2011;87(1030):550–7.
Tekkis PP, McCulloch P, Poloniecki JD, Prytherch DR, Kessaris N, Steger AC. Risk-adjusted prediction of operative mortality in oesophagogastric surgery with O-POSSUM. Br J Surg. 2004;91(3):288–95.
Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–51.
Murray P, Whiting P, Hutchinson SP, Ackroyd R, Stoddard CJ, Billings C. Preoperative shuttle walking testing and outcome after oesophagogastrectomy. Br J Anaesth. 2007;99(6):809–11.
Hightower CE, Riedel BJ, Feig BW, Morris GS, Ensor JE, Jr., Woodruff VD, et al. A pilot study evaluating predictors of postoperative outcomes after major abdominal surgery: Physiological capacity compared with the ASA physical status classification system. Br J Anaesth. 2010;104(4):465–71.
Reeh M, Metze J, Uzunoglu FG, Nentwich M, Ghadban T, Wellner U, et al. The PER (Preoperative Esophagectomy Risk) score: a simple risk score to predict short-term and long-term outcome in patients with surgically treated esophageal cancer. Medicine (Baltimore). 2016;95(7):e2724.
Struthers R, Erasmus P, Holmes K, Warman P, Collingwood A, Sneyd JR. Assessing fitness for surgery: a comparison of questionnaire, incremental shuttle walk, and cardiopulmonary exercise testing in general surgical patients. Br J Anaesth. 2008;101(6):774–80.
Ridgway ZA, Howell SJ. Cardiopulmonary exercise testing: a review of methods and applications in surgical patients. Eur J Anaesthesiol. 2010;27(10):858–65.
Smith TB, Stonell C, Purkayastha S, Paraskevas P. Cardiopulmonary exercise testing as a risk assessment method in non cardio-pulmonary surgery: a systematic review. Anaesthesia. 2009;64(8):883–93.
Lam S, Hart A. Cardiopulmonary exercise testing for predicting early outcomes after major cancer resection: a systematic review. J Anesth Periop Med. 2018;5:136–48.
Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–6.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Nagamatsu Y, Shima I, Yamana H, Fujita H, Shirouzu K, Ishitake T. Preoperative evaluation of cardiopulmonary reserve with the use of expired gas analysis during exercise testing in patients with squamous cell carcinoma of the thoracic esophagus. J Thorac Cardiovasc Surg. 2001;121(6):1064–8.
Forshaw MJ, Strauss DC, Davies AR, Wilson D, Lams B, Pearce A, et al. Is cardiopulmonary exercise testing a useful test before esophagectomy? Ann Thorac Surg. 2008;85(1):294–9.
Lam S, Alexandre L, Hardwick G, Hart AR. The association between preoperative cardiopulmonary exercise-test variables and short-term morbidity after esophagectomy: a hospital-based cohort study. Surgery. 2019;166(1):28–33.
Moyes LH, McCaffer CJ, Carter RC, Fullarton GM, Mackay CK, Forshaw MJ. Cardiopulmonary exercise testing as a predictor of complications in oesophagogastric cancer surgery. Ann Royal Coll Surg Engl. 2013;95(2):125–30.
Patel N, Powell AG, Wheat JR, Brown C, Appadurai IR, Davies RG, et al. Cardiopulmonary fitness predicts postoperative major morbidity after esophagectomy for patients with cancer. Physiol Rep. 2019;7(14):e14174.
Sinclair RCF, Phillips AW, Navidi M, Griffin SM, Snowden CP. Pre-operative variables including fitness associated with complications after oesophagectomy. Anaesthesia. 2017;72(12):1501–7.
Whibley J, Peters CJ, Halliday LJ, Chaudry AM, Allum WH. Poor performance in incremental shuttle walk and cardiopulmonary exercise testing predicts poor overall survival for patients undergoing esophago-gastric resection. Eur J Surg Oncol. 2018;44(5):594–9.
Beaver WL, Wasserman K, Whipp BJ. A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol (Bethesda, Md: 1985). 1986;60(6):2020–7.
Patel N, Wheat J, Brown C, Powell A, Abdelrahman T, Davies R, et al. Prognostic value of cardiopulmonary exercise testing for morbidity risk and survival after oesophagectomy for cancer. United Eur Gastroenterol J. 2017;5 (5 Supplement 1):A709.
Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, et al. CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Sem Radiat Oncol. 2003;13(3):176–81.
Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111(5):518–26.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg. 2009;250(2):177–86.
Kwak SG, Kim JH. Central limit theorem: the cornerstone of modern statistics. Korean J Anesthesiol. 2017;70(2):144–56.
Older PO, Levett DZH. Cardiopulmonary Exercise Testing and Surgery. Ann Am Thorac Soc. 2017;14(Supplement_1):S74–83.
Levett DZ, Grocott MP. Cardiopulmonary exercise testing, prehabilitation, and Enhanced Recovery After Surgery (ERAS). Canadian J Anaesth. 2015;62(2):131–42.
Older P, Smith R, Courtney P, Hone R. Preoperative evaluation of cardiac failure and ischemia in elderly patients by cardiopulmonary exercise testing. Chest. 1993;104(3):701–4.
Kusano C, Baba M, Takao S, Sane S, Shimada M, Shirao K, et al. Oxygen delivery as a factor in the development of fatal postoperative complications after oesophagectomy. Br J Surg. 1997;84(2):252–7.
Hall A, Older P. Cardiopulmonary Exercise Testing Accurately Predicts Risk of Major Surgery Including Esophageal Resection: Letter 1. Ann Thorac Surg. 2009;87(2):670–1.
Ney M, Haykowsky MJ, Vandermeer B, Shah A, Ow M, Tandon P. Systematic review: pre- and post-operative prognostic value of cardiopulmonary exercise testing in liver transplant candidates. Aliment Pharmacol Ther. 2016;44(8):796–806.
Kumar R, Garcea G. Cardiopulmonary exercise testing in hepato-biliary and pancreas cancer surgery: a systematic review. Are we any further than walking up a flight of stairs? Int J Surg (London, Engl). 2018;52:201–7.
Lee CHA, Kong JC, Ismail H, Riedel B, Heriot A. Systematic review and meta-analysis of objective assessment of physical fitness in patients undergoing colorectal cancer surgery. Dis Colon Rectum. 2018;61(3):400–9.
Robertson SA, Skipworth RJ, Clarke DL, Crofts TJ, Lee A, de Beaux AC, et al. Ventilatory and intensive care requirements following oesophageal resection. Ann Royal Coll Surg Engl. 2006;88(4):354–7.
Park DP, Welch CA, Harrison DA, Palser TR, Cromwell DA, Gao F, et al. Outcomes following oesophagectomy in patients with oesophageal cancer: a secondary analysis of the ICNARC Case Mix Programme Database. Crit Care (London, Engl). 2009;13 Suppl 2:S1.
Older P, Hall A, Hader R. Cardiopulmonary exercise testing as a screening test for perioperative management of major surgery in the elderly. Chest. 1999;116(2):355–62.
Huddart S, Young EL, Smith RL, Holt PJ, Prabhu PK. Preoperative cardiopulmonary exercise testing in England—a national survey. Periop Med (London, Engl). 2013;2(1):4.
Congedo E, Aceto P, Petrucci R, Mascia A, Gualtieri E, De Cosmo G. Preoperative anesthetic evaluation and preparation in patients requiring esophageal surgery for cancer. Rays. 2005;30(4):341–5.
Moran J, Wilson F, Guinan E, McCormick P, Hussey J, Moriarty J. Role of cardiopulmonary exercise testing as a risk-assessment method in patients undergoing intra-abdominal surgery: a systematic review. Br J Anaesth. 2016;116(2):177–91.
Garcia DO, Thomson CA. Physical activity and cancer survivorship. Nutr Clin Pract. 2014;29(6):768–79.
Wijeysundera DN, Pearse RM, Shulman MA, Abbott TEF, Torres E, Ambosta A, et al. Assessment of functional capacity before major non-cardiac surgery: an international, prospective cohort study. Lancet (London, Engl). 2018;391(10140):2631–40.
Doganay E, Moorthy K. Prehabilitation for esophagectomy. J Thorac Dis. 2019;11(Suppl 5):S632–8.
Arena R, Myers J, Williams MA, Gulati M, Kligfield P, Balady GJ, et al. Assessment of functional capacity in clinical and research settings: a scientific statement from the American Heart Association Committee on Exercise, Rehabilitation, and Prevention of the Council on Clinical Cardiology and the Council on Cardiovascular Nursing. Circulation. 2007;116(3):329–43.
Palange P, Ward SA, Carlsen KH, Casaburi R, Gallagher CG, Gosselink R, et al. Recommendations on the use of exercise testing in clinical practice. Eur Respir J. 2007;29(1):185–209.
Levett DZH, Jack S, Swart M, Carlisle J, Wilson J, Snowden C, et al. Perioperative cardiopulmonary exercise testing (CPET): consensus clinical guidelines on indications, organization, conduct, and physiological interpretation. Br J Anaesth. 2018;120(3):484–500.
Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, et al. Clinician’s Guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(2):191–225.
Herdy AH, Ritt LE, Stein R, Araujo CG, Milani M, Meneghelo RS, et al. Cardiopulmonary exercise test: background, applicability and interpretation. Arquivos Brasil Cardiol. 2016;107(5):467–81.
Weber KT, Janicki JS. Cardiopulmonary exercise testing for evaluation of chronic cardiac failure. Am J Cardiol. 1985;55(2):22a–31a.
Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof E, Fleischmann KE, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery): developed in collaboration with the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation. 2007;116(17):e418–99.
Wilson RJ, Davies S, Yates D, Redman J, Stone M. Impaired functional capacity is associated with all-cause mortality after major elective intra-abdominal surgery. Br J Anaesth. 2010;105(3):297–303.
Sjoquist KM, Burmeister BH, Smithers BM, Zalcberg JR, Simes RJ, Barbour A, et al. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol. 2011;12(7):681–92.
Allum WH, Stenning SP, Bancewicz J, Clark PI, Langley RE. Long-term results of a randomized trial of surgery with or without preoperative chemotherapy in esophageal cancer. J Clin Oncol. 2009;27(30):5062–7.
Navidi M, Phillips AW, Griffin SM, Duffield KE, Greystoke A, Sumpter K, et al. Cardiopulmonary fitness before and after neoadjuvant chemotherapy in patients with oesophagogastric cancer. Br J Surg. 2018;105(7):900–6.
Thomson IG, Wallen MP, Hall A, Ferris R, Gotley DC, Barbour AP, et al. Neoadjuvant therapy reduces cardiopulmunary function in patients undegoing oesophagectomy. Int J Surg (London, Engl). 2018;53:86–92.
von Dobeln GA, Nilsson M, Adell G, Johnsen G, Hatlevoll I, Tsai J, et al. Pulmonary function and cardiac stress test after multimodality treatment of esophageal cancer. Pract Radiat Oncol. 2016;6(3):e53–e9.
Goodyear SJ, Yow H, Saedon M, Shakespeare J, Hill CE, Watson D, et al. Risk stratification by pre-operative cardiopulmonary exercise testing improves outcomes following elective abdominal aortic aneurysm surgery: a cohort study. Periop Med (London, Engl). 2013;2(1):10.
Leclerc K. Cardiopulmonary exercise testing: a contemporary and versatile clinical tool. Cleveland Clin J Med. 2017;84(2):161–8.
Acknowledgements
The authors acknowledge the substantial contribution of investigators who kindly provided additional data requested from their original manuscripts: Dr. Arfon Powell (Cardiff University School of Medicine, Cardiff) and Dr. Christopher Peters (Imperial College London, St Mary’s Hospital, London).
Funding
No Grant support or financial assistance was sought.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
No conflict of interest to declare from any of the above authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sivakumar, J., Sivakumar, H., Read, M. et al. The Role of Cardiopulmonary Exercise Testing as a Risk Assessment Tool in Patients Undergoing Oesophagectomy: A Systematic Review and Meta-analysis. Ann Surg Oncol 27, 3783–3796 (2020). https://doi.org/10.1245/s10434-020-08638-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08638-9