Abstract
Background
Clinical trials are currently ongoing to determine the safety and efficacy of active surveillance (AS) versus usual care (surgical and radiation treatment) for women with ductal carcinoma in situ (DCIS). This study aimed to determine upgrade rates of DCIS at needle biopsy to invasive carcinoma at surgery among women who meet the eligibility criteria for AS trials.
Methods
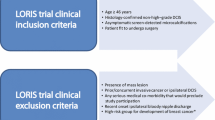
A retrospective review was performed of consecutive women at an academic medical center with a diagnosis of DCIS at needle biopsy from 2007 to 2016. Medical records were reviewed for mode of presentation, imaging findings, biopsy pathology results, and surgical outcomes. Each patient with DCIS was evaluated for AS trial eligibility based on published criteria for the COMET, LORD, and LORIS trials.
Results
During a 10-year period, DCIS was diagnosed in 858 women (mean age 58 years; range 28–89 years). Of the 858 women, 498 (58%) were eligible for the COMET trial, 101 (11.8%) for the LORD trial, and 343 (40%) for the LORIS trial. The rates of upgrade to invasive carcinoma were 12% (60/498) for the COMET trial, 5% (5/101) for the LORD trial, and 11.1% (38/343) for the LORIS trial. The invasive carcinomas ranged from 0.2 to 20 mm, and all were node-negative.
Conclusions
Women who meet the eligibility criteria for DCIS AS trials remain at risk for occult invasive carcinoma at presentation, with upgrade rates ranging from 5 to 12%. These findings suggest that more precise criteria are needed to ensure that women with invasive carcinoma are excluded from AS trials.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Ductal carcinoma in situ (DCIS) is a noninvasive form of breast cancer characterized by proliferation of malignant epithelial cells without invasion through the basement membrane.1 Surgery, radiation, and endocrine therapy can benefit women with DCIS by preventing progression to invasive carcinoma and by reducing local recurrence. However, certain patients will not progress to invasive carcinoma even without surgery.2,3,4
The heterogeneity of DCIS and the resultant challenge to predict patient outcomes have led to routine use of surgery and radiation for all patients. Ideally, patients with indolent DCIS could be spared the potential morbidities of treatment.5 In addition, many women with DCIS elect to undergo mastectomy rather than lumpectomy, which further contributes to the burden of treatment.6
Given these concerns regarding overtreatment of DCIS, active surveillance (AS) trials currently are underway. In these trials, surgical excision of DCIS is not performed, follow-up imaging to detect progression to invasive carcinoma is obtained, and endocrine therapy to decrease growth may be used. Current randomized controlled trials comparing AS with standard treatment for DCIS include the Comparison of Operative to Monitoring and Endocrine Therapy (COMET) trial for low-risk DCIS in the United States, the LOw-Risk DCIS (LORD) trial in Europe, and the LOw-RISk DCIS (LORIS) trial in the United Kingdom.7,8,9
Robust and precise patient eligibility criteria are needed for the successful implementation of AS programs.10 In particular, these criteria must be developed to exclude patients with DCIS likely to be upgraded to invasive carcinoma at the time of surgery, which occurs in approximately one fourth of patients.11 This study aimed to determine the upgrade rates of DCIS at needle biopsy to invasive carcinoma at surgery among women who meet the eligibility criteria for AS trials.
Methods
Study Population
The institutional review board exempted this Health Insurance Portability and Accountability Act (HIPAA)-compliant retrospective study from the requirement for written informed consent. We identified patients with DCIS through our institution’s mammography information system (MagView, Burtonsville, MD, USA) who presented from 1 January 2007 to 31 December 2016 with screen-detected calcifications at mammography, had DCIS diagnosed with vacuum-assisted breast biopsy, and underwent subsequent surgical excision.
All the included patients underwent mammography-guided vacuum-assisted breast biopsy with a 9-gauge needle (Eviva; Hologic, Marlborough, MA, USA) performed by dedicated breast imaging radiologists, supervised fellows, or senior residents. Six to eight samples were acquired in most cases, and specimen radiographs were obtained to confirm the presence of calcifications. Histopathology slides were reviewed by dedicated breast pathologists. All the patients showed pure DCIS on core biopsy with no evidence of invasion or microinvasion. Core biopsies with missing nuclear grade or missing hormone receptor status were excluded.
Data Collection
From the electronic medical record system, the following information was extracted: patient age, race, risk factors for breast cancer (e.g., family history and personal history of breast cancer), and history of chemoprevention use. The core biopsy pathology reports were reviewed for nuclear grade of DCIS, hormone receptor status, and presence or absence of comedonecrosis. The surgical pathology reports were reviewed for the presence or absence of invasive carcinoma. If invasive carcinoma was present, size, grade, hormone receptor status, and nodal status were recorded.
Case Classification and Statistical Analysis
Each patient with DCIS was evaluated for AS trial eligibility based on the published criteria for the COMET, LORD, and LORIS trials7,8,9 (Table 1). Notably, patients with masses on imaging at the site of biopsy for DCIS are not eligible for any of the trials.7,8,9
For the COMET trial, two clinical pathologists (not required to be at the same institution) must agree that the pathologic features fulfill the eligibility criteria.9 In cases of disagreement, a third pathology review is required.9 To be eligible for the LORD trial, histologic confirmation of unilateral low-grade DCIS by a local pathologist is necessary.7 For the LORIS trial, a central histopathology review process is required, with each case reviewed by a minimum of two pathologists.8 The eligibility criteria for the LORIS trial include low nuclear grade or lower half of the intermediate-grade category (“where low grade has been considered in the diagnostic categorization”), no comedonecrosis, no more than occasional mitoses (no more than 1 per 3 duct cross-section), and nuclei with minimal pleomorphism and not more than 2.5 red blood cells in diameter.8 For the LORIS trial, only patients who meet these criteria are eligible for randomization.8
Upgrade rates over time, by patient risk factors (including age, family history of breast cancer in a first-degree relative, and personal history of breast cancer), and by pathologic features at biopsy (including nuclear grade, comedonecrosis, and estrogen receptor status) were calculated and compared using unpaired t tests for continuous variables and Chi square tests for categorical variables. In addition, upgrade rates for cases that met published eligibility criteria for the COMET, LORD, and LORIS trials were calculated and compared using Chi square tests. Data were analyzed with statistical software (R, version 3.5.1; R Foundation for Statistical Computing, Vienna, Austria). All p values lower than 0.05 were considered statistically significant.
Results
Study Population
During a 10-year period, the core biopsy resulted in a diagnosis of unilateral DCIS in 1009 patients and bilateral DCIS in 7 patients, yielding a total of 1016 patients with 1023 cases of DCIS. Cases with missing nuclear grade at core biopsy (8.9%, 91/1023) or missing hormone receptor status (6.5%, 67/1023) were excluded from the study. The study cohort therefore comprised 851 patients with unilateral DCIS and 7 patients with bilateral DCIS, for a total of 858 patients with 865 cases of DCIS. For the seven patients with bilateral DCIS, the higher grade or otherwise more aggressive DCIS was included in the analysis.
The mean age of the patients was 58 years (range 28–89 years), and the majority were white women (91.3%, 773/847) (Table 2). More than half of the patients had intermediate-grade DCIS (55.4%, 475/858), and the vast majority were estrogen receptor (ER)-positive (90.7%, 778/858) (Table 2). Nearly one third of the patients had comedonecrosis at biopsy (31.1%, 267/858) (Table 2).
The overall rate of upgrade to invasive carcinoma was 14.8% (127/858) (Table 2), with 115 patients (90.6%) upgraded to invasive ductal carcinoma (IDC), 10 patients (7.9%) upgraded to invasive lobular carcinoma (ILC), and 2 patients (1.6%) upgraded to invasive carcinoma with ductal and lobular features. The tumors ranged from 0.2 to 22 mm in size (Table 2), with 35.4% (45/127) upgraded to microinvasive disease (≤ 1 mm) (Table 2). Only 1.9% (2/105) of the patients were node-positive (Table 2). Nine additional cases (8.6%, 9/105) had isolated tumor cells in one to three lymph nodes.
Upgrade Rates by Year, Patient Risk Factors, and Pathologic Features at Biopsy
There were no significant differences in upgrade rates of DCIS to invasive carcinoma over time (12.5–19.4% when calculated over 2-year intervals, p = 0.36–0.86 when compared with the first 2-year interval). The patients who were upgraded to invasive carcinoma did not differ significantly from those who were not in terms of patient age (58 vs 58 years; p = 0.69), family history of breast cancer in a first-degree relative (24.4% [31/127] vs 28.9% [211/731]; p = 0.30), or personal history of breast cancer (18.1% [23/127] vs 13.5% [99/731]; p = 0.17). The overall upgrade rate to invasive carcinoma was 7.9% (10/127) for the patients with low-grade DCIS, 14.7% (70/475) for those with intermediate-grade DCIS, and 18.4% (47/256) for those with high-grade DCIS. The upgrade rate for intermediate-grade DCIS was higher than for low-grade DCIS (p = 0.04). The upgrade rate for high-grade DCIS was higher than for low-grade DCIS (p < 0.01) but not intermediate-grade DCIS (p = 0.20). The presence of comedonecrosis at biopsy was not associated with risk of upgrade (37.0% [47/127] vs 30.1% [220/731]; p = 0.12), nor was estrogen receptor status (10.2% [13/127] vs 9.2% [67/731]; p = 0.70).
Trial-Eligible Patients
Based on published eligibility criteria, 498 patients (58%, 498/858) were eligible for the COMET trial, 101 patients (11.8%, 101/858) for the LORD trial, and 343 patients (40%, 343/858) for the LORIS trial (Table 2). The rates of upgrade to invasive carcinoma were 12% (60/498) for the COMET trial, 5% (5/101) for the LORD trial, and 11.1% (38/343) for the LORIS trial (Table 2). The upgrade rate for the COMET trial was higher than for the LORD trial (p = 0.04). The upgrade rate for the LORIS trial trended toward being higher than for the LORD trial (p = 0.07), and the upgrade rates for the COMET and LORIS trials did not differ significantly (p = 0.67).
Invasive Carcinoma Characteristics
Among the patients in our study who would have been eligible for one of the three trials, 63 patients had invasive carcinoma at surgery (Table 2), and 54 (85.7%) were upgraded to IDC, 8 (12.7%) to ILC, and 1 (1.6%) to invasive carcinoma with ductal and lobular features. The tumors ranged from 0.2 to 20 mm in size. Of the patients with invasive disease, 28.6% (18/63) had only microinvasive disease (≤ 1 mm). Of the invasive carcinomas, 20.6% (13/63) were grade 1, 50.8% (32/63) were grade 2, 15.9% (10/63) were grade 3, and 12.7% (8/63) had no grade reported.
In terms of ER status, 81% (51/63) of the patients were ER-positive, 9.5% (6/63) were ER-negative, and 9.5% (6/63) had unknown ER status. Regarding progesterone receptor (PR) status, 65.1% (41/63) were PR-positive, 23.8% (15/63) were PR-negative, and 11.1% (7/63) had unknown PR status. With respect to human epidermal growth factor receptor 2 (HER2) status, 20.6% (13/63) of the patients were HER2-positive, 68.3% (43/63) were HER2-negative, and 11.1% (7/63) had unknown HER2 status. None of the 48 patients who had undergone a sentinel node biopsy showed a macrometastasis or micrometastasis, but four patients (8.3%) showed isolated tumor cells in one lymph node.
Discussion
In our cohort of patients with DCIS at core biopsy, the overall upgrade rate to invasive carcinoma at surgery was 14.8% (127/858). When we applied the eligibility criteria for the COMET, LORD, and LORIS trials to our cohort, the upgrade rates were reduced to 12% (60/498) for COMET, 5% (5/101) for LORD, and 11.1% (38/343) for LORIS. The LORD trial has the most stringent eligibility criteria, with only 11.8% (101/858) of our patients qualifying, and also the lowest upgrade rate. These findings suggest that more precise criteria are needed to determine eligibility for AS trials to ensure that women with occult invasive carcinoma are not included in the trials.
The reported upgrade rates of DCIS to invasive carcinoma range from less than 10% to greater than 40%.11,12,13,14,15,16,17,18,19,20,21,22 For example, a meta-analysis of 52 studies reported an overall upgrade rate of 25.9%.11 Our lower overall upgrade rate of 14.8% may have been due to patient selection. Our cohort included only patients who presented with screen-detected calcifications at mammography and had their diagnoses determined with a 9-gauge vacuum-assisted breast biopsy. The meta-analysis, however, included patients who presented with various findings found on imaging (including mammographic masses), with palpable abnormalities, and with diagnoses determined using various biopsy techniques (including smaller-gauge biopsy devices), all of which could contribute to a higher upgrade rate.11
To our knowledge, our study is the largest to date that compared eligibility criteria for all three current AS trials. In a study from Duke University Medical Center, the upgrade rates were 6.2% (5/81) for the COMET trial, 10.0% (1/10) for the LORD trial, and 6.8% (5/74) for the LORIS trial.23 We found higher upgrade rates with the COMET and LORIS trials and a lower upgrade rate with the LORD trial. These differences in upgrade rates may be related to patient numbers, pathologists’ interpretations of DCIS, or both. With regard to patient numbers, for example, the Duke study included only 10 patients with DCIS who were eligible for the LORD trial, which limits our ability to make direct comparisons and draw conclusions from the data. Regarding pathology, a study that included clinical practices in eight U.S. states demonstrated a lack of diagnostic concordance, with overall agreement between individual pathologists and an expert consensus panel at 75.3%.24 The highest level of concordance was for invasive carcinoma, with lower levels of concordance for DCIS and atypia.24 Recognizing this lack of diagnostic concordance, the COMET trial requires two clinical pathologists to agree that the pathologic features fulfill the eligibility criteria, and the LORIS trial requires a central histopathology review process, with each case reviewed by a minimum of two pathologists.8,9
A study from the Memorial Sloan Kettering Cancer Center reported an upgrade rate of 19.6% (58/296) among women eligible for the LORIS trial, which is higher than the upgrade rate of 11.1% that we found.25 In contrast, a smaller study from the UK reported an upgrade rate of 0% among 19 women eligible for the LORIS trial.26 This study included only patients with low-grade DCIS, although the eligibility criteria for the LORIS trial include both low-grade DCIS and the lower half of intermediate-grade DCIS (“where low grade has been considered in the diagnostic categorization”).8 In a study from Vanderbilt University and the University of Louisville Hospital, 20 (19.0%) of 105 upgraded cases met the criteria for the LORIS trial, whereas only 3 (2.9%) of 105 upgraded cases met the criteria for the LORD trial.27
Our findings suggest that more precise criteria are needed to ensure that women with invasive carcinoma are excluded from AS trials. In fact, in a risk analysis predicting disease-specific cumulative mortality for AS versus standard treatment, the variable with the greatest risk of mortality was understaging of invasive carcinoma at the time of diagnosis.28 However, as the criteria become stricter, the proportion of patients who are eligible for AS decreases. For example, the LORD trial has the most stringent eligibility criteria (and thus the lowest proportion of eligible patients) and also the lowest upgrade rate. Notably, more patients were eligible for the COMET trial than for the LORIS trial, but the upgrade rates did not differ significantly. One difference in the eligibility criteria between the two trials is that COMET allows patients with comedonecrosis to enroll, but LORIS does not.8,9 However, among all the patients in our study cohort, the presence of comedonecrosis at biopsy was not associated with risk of upgrade. Ultimately, better tools, such as contrast-enhanced magnetic resonance imaging (MRI), genomic tests, and deep learning algorithms, are needed to identify more precisely the patients with DCIS who may benefit from less aggressive therapies.29,30,31,32,33
In our patient cohort, the occult invasive carcinomas ranged from 0.2 to 20 mm in size at surgery, and approximately 29% were microinvasive disease (≤ 1 mm). The outcomes for these women with occult invasive carcinomas had they opted for active surveillance are not known. Their risk is not the probable outcome associated with the invasive carcinomas we report, but rather the prognosis associated with cancers in the future when ultimately found and treated, which would depend in part on the frequency and sensitivity of follow-up imaging. The current AS trials will provide insight into patient outcomes and specifically whether delays in invasive carcinoma diagnoses are clinically meaningful.
Our study had several limitations. It was conducted at an academic institution with dedicated breast imaging radiologists and pathologists, and the results therefore might not be generalizable to all institutions. Furthermore, our population was fairly homogeneous, limiting our ability to generalize our findings to non-Caucasian women. Although all cases were interpreted by specialized breast pathologists at our institution, no consensus review or centralized pathology review was performed, as required by the COMET and LORIS trials. In addition, the LORD trial has stringent requirements for vacuum-assisted biopsies of calcifications (6 or more samples with an 8- or 9-gauge needle or 12 or more samples with a 10- or 11-gauge needle).7 Although data about the exact number of core biopsy samples acquired per case were not available for our analysis, the biopsy protocol at our institution (6–8 samples with a 9-gauge needle) are in keeping with the requirements of the LORD trial.
The success of the ongoing active surveillance programs depends on robust and precise patient eligibility criteria. Our results demonstrate that patients who meet the current eligibility criteria for DCIS active surveillance trials remain at risk for occult invasive carcinoma at presentation, with upgrade rates ranging from 5 to 12%. These findings suggest that more precise criteria are needed to ensure that women with invasive carcinoma are excluded from AS trials.
References
Yamada T, Mori N, Watanabe M, et al. Radiologic-pathologic correlation of ductal carcinoma in situ. Radiographics. 2010;30:1183–98. https://doi.org/10.1148/rg.305095073.
Mitchell KB, Kuerer H. Ductal carcinoma in situ: treatment update and current trends. Curr Oncol Rep. 2015;17:48. https://doi.org/10.1007/s11912-015-0473-x.
Pang JM, Gorringe KL, Fox SB. Ductal carcinoma in situ: update on risk assessment and management. Histopathology. 2016;68:96–109. https://doi.org/10.1111/his.12796.
Rosso KJ, Weiss A, Thompson AM. Are there alternative strategies for the local management of ductal carcinoma in situ? Surg Oncol Clin North Am. 2018;27:69–80. https://doi.org/10.1016/j.soc.2017.08.002.
Bruce J, Thornton AJ, Scott NW, et al. Chronic preoperative pain and psychological robustness predict acute postoperative pain outcomes after surgery for breast cancer. Br J Cancer. 2012;107:937–46. https://doi.org/10.1038/bjc.2012.341.
Miller ME, Muhsen S, Olcese C, et al. Contralateral breast cancer risk in women with ductal carcinoma in situ: is it high enough to justify bilateral mastectomy? Ann Surg Oncol. 2017;24:2889–97. https://doi.org/10.1245/s10434-017-5931-2.
Elshof LE, Tryfonidis K, Slaets L, et al. Feasibility of a prospective, randomised, open-label, international multicentre, phase III, non-inferiority trial to assess the safety of active surveillance for low risk ductal carcinoma in situ: the LORD study. Eur J Cancer. 2015;51:1497–510. https://doi.org/10.1016/j.ejca.2015.05.008.
Francis A, Thomas J, Fallowfield L, et al. Addressing overtreatment of screen detected DCIS; the LORIS trial. Eur J Cancer. 2015;51:2296–303. https://doi.org/10.1016/j.ejca.2015.07.017.
Hwang ES, Hyslop T, Lynch T, et al. The COMET (Comparison of Operative versus Monitoring and Endocrine Therapy) trial: a phase III randomised controlled clinical trial for low-risk ductal carcinoma in situ (DCIS). BMJ Open. 2019;9:e026797. https://doi.org/10.1136/bmjopen-2018-026797.
Grimm LJ, Shelley Hwang E. Active surveillance for DCIS: the importance of selection criteria and monitoring. Ann Surg Oncol. 2016;23:4134–6. https://doi.org/10.1245/s10434-016-5596-2.
Brennan ME, Turner RM, Ciatto S, et al. Ductal carcinoma in situ at core-needle biopsy: meta-analysis of underestimation and predictors of invasive breast cancer. Radiology. 2011;260:119–28. https://doi.org/10.1148/radiol.11102368.
Brem RF, Schoonjans JM, Goodman SN, et al. Nonpalpable breast cancer: percutaneous diagnosis with 11- and 8-gauge stereotactic vacuum-assisted biopsy devices. Radiology. 2001;219:793–6. https://doi.org/10.1148/radiology.219.3.r01jn34793.
Jackman RJ, Burbank F, Parker SH, et al. Stereotactic breast biopsy of nonpalpable lesions: determinants of ductal carcinoma in situ underestimation rates. Radiology. 2001;218:497–502. https://doi.org/10.1148/radiology.218.2.r01fe35497.
Wahedna Y, Evans AJ, Pinder SE, et al. Mammographic size of ductal carcinoma in situ does not predict the presence of an invasive focus. Eur J Cancer. 2001;37:459–62. https://doi.org/10.1016/s0959-8049(00)00397-x.
Goyal A, Douglas-Jones A, Monypenny I, et al. Is there a role of sentinel lymph node biopsy in ductal carcinoma in situ? Analysis of 587 cases. Breast Cancer Res Treat. 2006;98:311–4. https://doi.org/10.1007/s10549-006-9167-2.
Houssami N, Ciatto S, Ellis I, Ambrogetti D. Underestimation of malignancy of breast core-needle biopsy: concepts and precise overall and category-specific estimates. Cancer. 2007;109:487–95. https://doi.org/10.1002/cncr.22435.
Houssami N, Ambrogetti D, Marinovich ML, et al. Accuracy of a preoperative model for predicting invasive breast cancer in women with ductal carcinoma in situ on vacuum-assisted core needle biopsy. Ann Surg Oncol. 2011;18:1364–71. https://doi.org/10.1245/s10434-010-1438-9.
Kim J, Han W, Lee JW, et al. Factors associated with upstaging from ductal carcinoma in situ following core needle biopsy to invasive cancer in subsequent surgical excision. Breast. 2012;21:641–5. https://doi.org/10.1016/j.breast.2012.06.012.
Trentin C, Dominelli V, Maisonneuve P, et al. Predictors of invasive breast cancer and lymph node involvement in ductal carcinoma in situ initially diagnosed by vacuum-assisted breast biopsy: experience of 733 cases. Breast. 2012;21:635–40. https://doi.org/10.1016/j.breast.2012.06.009.
Schulz S, Sinn P, Golatta M, et al. Prediction of underestimated invasiveness in patients with ductal carcinoma in situ of the breast on percutaneous biopsy as rationale for recommending concurrent sentinel lymph node biopsy. Breast. 2013;22:537–42. https://doi.org/10.1016/j.breast.2012.11.002.
Parikh U, Chhor CM, Mercado CL. Ductal carcinoma in situ: the whole truth. AJR Am J Roentgenol. 2018;210:246–55. https://doi.org/10.2214/ajr.17.18778.
Lamb LR, Lehman CD, Oseni TO, Bahl M. Ductal carcinoma in situ (DCIS) at breast MRI: predictors of upgrade to invasive carcinoma. Acad Radiol. 2019. Epub ahead of print. https://doi.org/10.1016/j.acra.2019.09.025.
Grimm LJ, Ryser MD, Partridge AH, et al. Surgical upstaging rates for vacuum-assisted biopsy-proven DCIS: implications for active surveillance trials. Ann Surg Oncol. 2017;24:3534–40. https://doi.org/10.1245/s10434-017-6018-9.
Elmore JG, Longton GM, Carney PA, et al. Diagnostic concordance among pathologists interpreting breast biopsy specimens. JAMA. 2015;313:1122–32. https://doi.org/10.1001/jama.2015.1405.
Pilewskie M, Stempel M, Rosenfeld H, et al. Do LORIS trial eligibility criteria identify a ductal carcinoma in situ patient population at low risk of upgrade to invasive carcinoma? Ann Surg Oncol. 2016;23:3487–93. https://doi.org/10.1245/s10434-016-5268-2.
Soumian S, Verghese ET, Booth M, et al. Concordance between vacuum-assisted biopsy and postoperative histology: implications for the proposed Low-Risk DCIS Trial (LORIS). Eur J Surg Oncol. 2013;39:1337–40. https://doi.org/10.1016/j.ejso.2013.09.028.
Podoll MB, Reisenbichler ES, Roland L, et al. Feasibility of the less-is-more approach in treating low-risk ductal carcinoma in situ diagnosed on core needle biopsy: ten-year review of ductal carcinoma in situ upgraded to invasion at surgery. Arch Pathol Lab Med. 2018;142:1120–6. https://doi.org/10.5858/arpa.2017-0268-oa.
Ryser MD, Worni M, Turner EL, et al. Outcomes of active surveillance for ductal carcinoma in situ: a computational risk analysis. J Natl Cancer Inst. 2015;108. https://doi.org/10.1093/jnci/djv372.
Shi B, Grimm LJ, Mazurowski MA, et al. Can occult invasive disease in ductal carcinoma in situ be predicted using computer-extracted mammographic features? Acad Radiol. 2017;24:1139–47. https://doi.org/10.1016/j.acra.2017.03.013.
Lin CY, Mooney K, Choy W, et al. Will oncotype DX DCIS testing guide therapy? A single-institution correlation of oncotype DX DCIS results with histopathologic findings and clinical management decisions. Mod Pathol. 2018;31:562–8. https://doi.org/10.1038/modpathol.2017.172.
Shi B, Grimm LJ, Mazurowski MA, et al. Prediction of occult invasive disease in ductal carcinoma in situ using deep learning features. J Am Coll Radiol. 2018;15(3 Pt B):527–34. https://doi.org/10.1016/j.jacr.2017.11.036.
Lehman CD, Gatsonis C, Romanoff J, et al. Association of magnetic resonance imaging and a 12-gene expression assay with breast ductal carcinoma in situ treatment. JAMA Oncol. 2019;5:1036–42. https://doi.org/10.1001/jamaoncol.2018.6269.
Zhu Z, Harowicz M, Zhang J, et al. Deep learning analysis of breast MRIs for prediction of occult invasive disease in ductal carcinoma in situ. Comput Biol Med. 2019;115:103498. https://doi.org/10.1016/j.compbiomed.2019.103498.
Acknowledgement
This work was supported by the Agfa HealthCare/Radiological Society of North America (RSNA) Research Scholar Grant (Principal Investigator (PI): Dr. Manisha Bahl) and the Electronic Space Systems Corporation (ESSCO)-MGH Breast Cancer Research Fund (PI: Dr. Manisha Bahl and Dr. Tawakalitu O. Oseni).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Constance D. Lehman has served as an advisory board member for GE Healthcare, and her institution has received research support from GE Healthcare. Tawakalitu O. Oseni, Barbara L. Smith, Charmi A. Vijapura, Niveditha Pinnamaneni, and Manisha Bahl declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Oseni, T.O., Smith, B.L., Lehman, C.D. et al. Do Eligibility Criteria for Ductal Carcinoma In Situ (DCIS) Active Surveillance Trials Identify Patients at Low Risk for Upgrade to Invasive Carcinoma?. Ann Surg Oncol 27, 4459–4465 (2020). https://doi.org/10.1245/s10434-020-08576-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08576-6