Abstract
Background
As tumor biology takes precedence over anatomic staging to determine breast cancer (BC) prognosis, there is growing interest in limiting axillary surgery. There is a need for tools to identify patients at the lowest risk of harboring axillary lymph node (ALN) disease, to determine when omission of sentinel lymph node biopsy (SLNB) may be appropriate. We examined whether a nomogram using preoperative axillary ultrasound (axUS) findings, clinical tumor size, receptor status, and grade to calculate the probability of nodal metastasis (PNM) has value in surgical decision making.
Methods
This was a retrospective analysis of female patients (February 2011–October 2014) with invasive BC who underwent preoperative axUS and axillary surgery. Cases with locally advanced BC, neoadjuvant treatment, or bilateral BC were excluded. PNM was calculated for each case. Using various PNM thresholds, the proportion of cases with ALN metastasis on pathology was examined to determine an optimal PNM cut-point to predict ALN negativity.
Results
Of 357 included patients, 72% were node-negative on surgical staging, and 69 (19.6%) had a PNM < 9.3%. Of these 69 patients, 6 had ALN metastasis on surgical pathology, yielding a false negative rate (FNR) of 8.7% for predicting negative ALN when a PNM threshold of < 9.3% was used.
Conclusion
A nomogram incorporating axUS findings and tumor characteristics identified a sizeable subgroup (19.6%) in whom ALN was predicted to be negative, with an 8.7% FNR. Surgeons can use this nomogram to quantify the probability of ALN metastasis and select patients who may benefit from omitting SLNB.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Surgical axillary staging is the standard of care for breast cancer (BC) management as it aids in establishing prognosis and influences adjuvant treatment recommendations. Axillary surgery has evolved from the morbid axillary lymph node dissection (ALND), associated with lymphedema rates ranging from 8.4 to 21.4%,1 to sentinel lymph node biopsy (SLNB) for patients without palpable adenopathy. Still, SLNB carries morbidities: lymphedema is reported in 2–6% of patients,1,2 and 9% experience long-term paresthesias.2
Many studies suggest that for patients with a low likelihood of having axillary nodal metastasis, it is unlikely that omission of SLNB would directly impact survival or lead to unacceptably high local recurrence rates. In the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-04 trial,3 25-year outcomes revealed no survival decrement from omission of axillary staging (via ALND) in clinically node-negative patients. This is despite a 40% prevalence of nodal involvement seen in the radical mastectomy (control) group. In the Cancer and Leukemia Group B (CALGB) 93434 study of patients > 70 years of age with cT1N0M0 hormone receptor-positive BC treated with partial mastectomy, subset analysis showed that the omission of both radiation and axillary surgery was associated with an only 3% axillary recurrence rate. Similarly, in a trial of patients aged 65–80 years with cT1N0M0 disease randomized to ALND versus no axillary surgery, Martelli et al.5 found no survival difference between the groups, and a 5-year axillary recurrence rate of only 1.8% in the no ALND group. This low axillary recurrence rate was observed despite a 23% prevalence of nodal involvement in the ALND group.
Based on these findings, the Choosing Wisely6 campaign recommends against the routine use of SLNB in women > 70 years of age with hormone receptor-positive invasive BC. In a healthy septuagenarian, surgeons would be more comfortable omitting SLNB if the risk of positive SLN could be determined to be very low; however, surgeons do not currently have the tools to identify patients’ risk of nodal metastasis.
We undertook a study to determine whether a nomogram incorporating axillary ultrasound (axUS) features and tumor characteristics could be useful to identify patients with < 10% risk of positive SLNB. In 2016, researchers at the Shantou University Medical College in China reported an ultrasound-based nomogram, herein referred to as the Shantou nomogram, to predict the probability of nodal metastasis (PNM) in the axilla.7 Unlike other nomograms that use only surgical pathology data, the Shantou nomogram also incorporates preoperative axUS characteristics and core biopsy results (Table 1) to predict the PNM. However, it was unknown whether this nomogram could be used in our North American patient population to determine a subgroup with < 10% likelihood of positive SLNB.
The objective of the present study was to determine if a nomogram incorporating axUS features and tumor characteristics could be used in a North American patient population to identify a subset with < 10% risk of ALN metastasis, with a goal of guiding surgeons in deciding whether SLNB may be omitted. This is the first independent analysis of the Shantou nomogram, and the first study to examine whether this tool can be used in a heterogeneous patient population characteristic of North American cancer centers to identify a subset of patients with < 10% risk of ALN metastasis.
Methods
This retrospective analysis of newly diagnosed female BC patients treated at the Rebecca Fortney Breast Center (RFBC) at Anne Arundel Medical Center was approved by the Institutional Review Board. Cases from February 2011 through October 2014 were selected. All patients with invasive BC who had a preoperative axUS and underwent SLNB and/or ALND were included in the study. Patients were excluded if they had locally advanced BC, neoadjuvant treatment, bilateral BC, previous ipsilateral axillary surgery, or if no lymph node was seen on axUS. These criteria were similar to those used to develop the nomogram.7 Locally advanced disease was defined as N2-3 disease on physical examination. At the RFBC, patients with newly diagnosed or suspected BC routinely undergo axUS as part of their preoperative work-up, regardless of the clinical axillary examination. If one or more suspicious lymph nodes are identified on preoperative axUS, an ultrasound-guided core biopsy of the node is recommended prior to surgery. A sonographically suspicious lymph node is defined by diffuse or focal cortical thickening > 3 mm, focal cortical nodule, or loss of fatty hilum.
Data Collection
Patient data, including ethnicity, age at diagnosis, Nottingham grade, estrogen receptor (ER) status, progesterone receptor (PR) status, human epidermal growth factor receptor 2 (HER2), and clinical tumor size were collected from the electronic medical record. Information for histologic grade and ER, PR, and HER2 status were obtained from the core biopsy specimen. The clinical tumor size was taken from the surgeon’s estimate of tumor size, based on imaging available at the time of initial consultation (typically mammogram and ultrasound) and physical examination findings. For multifocal tumors, the size of the largest tumor was recorded. Staging was performed according to the tumor, node, metastasis (TNM) 7th edition American Joint Committee on Cancer (AJCC) classification system. We categorized ER, PR, and HER2 according to staining percentage, using categories defined by Qiu et al.7
Sonographic ALN measurements were collected retrospectively from static images captured at the time of diagnostic imaging. Ultrasound examinations were performed by trained radiology technicians and radiologists using GE Logic 9 and Acuson S2000 ultrasound units. When multiple lymph nodes were visualized, the suspicious LN targeted for core biopsy was used to obtain LN measurements. If LN core biopsy was not performed, the most suspicious LN was chosen for measurement collection. Nodes with loss of fatty hilum were considered most suspicious, followed by those with thickened cortex. If no suspicious feature was observed, then the lymph node with the longest axis was chosen for measurement. Hilum presence or absence was considered as a binary variable; if any hilum was visible, it was recorded as present. The LN features were collected by the breast surgical oncology fellow (HT), after being trained by a breast radiologist (DP) and a breast surgeon (RJ). Any uncertain cases were reviewed with the breast radiologist (DP).
Statistical Analysis
Shantou nomogram predictions were calculated using the formula published by Qiu et al.7 The implementation was verified by comparing the PNM computed for the study with the Evidencio website’s implementation of the Shantou nomogram (https://app.evidencio.com/models/show/170).7 The JMP 9.0.2 statistical package (SAS Institute, Cary, NC, USA) was used to compute descriptive statistics for the clinicopathological characteristics and the receiver operating characteristic (ROC) curve for the risk predictions. Various PNM cut-offs were selected, and, for each cut-off, the sensitivity, specificity, and false negative rate (FNR) for predicting ALN metastasis were calculated. The FNR at each threshold was calculated as follows:
Specifically, we sought to identify a PNM threshold that would yield an FNR of approximately 8.4%, as this is the acceptable FNR for SLNB according to American Society of Clinical Oncology guidelines.8 Sensitivity and specificity were calculated similarly, using standard definitions, for each PNM threshold.
Results
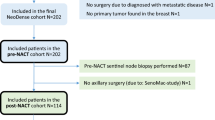
There were 947 patients with newly diagnosed invasive BC in the axUS database. Of these, 357 patients met the criteria as described above (Fig. 1). A comparison of clinicopathological characteristics between the Shantou modeling cohort,7 the Dutch study9 population (used in a previous validation study), and the RFBC study population is provided in Table 2. The RBFC cohort consisted of 79.6% Caucasians, 14.3% African Americans, 0.8% Asians, and 5.3% in which ethnicity was not reported. When compared with the Shantou cohort, the RBFC cohort had more favorable tumor biology, smaller tumor size, and older age at presentation. The Shantou cohort had more axUS abnormalities, including a larger median LN cortical thickness (4.0 mm vs. 2.2 mm) and a lower proportion of patients with present LN hilum (60.9% vs. 96.4%), compared with the RFBC group. The proportion of patients with ALN metastasis on resected specimen was greater in the Shantou cohort compared with the RBFC cohort (50.6% vs. 28.0%). In general, the Dutch and RBFC cohorts had similar tumor biology but differed in ethnicity.
When applied to the RBFC cohort, the Shantou nomogram had fair discrimination, with an area under the ROC curve (AUC) of 0.70 (95% confidence interval 0.64–0.76).
Sensitivity, specificity, and FNR using various PNM thresholds are displayed in Table 3. No case with PNM < 4.6% had ALN metastasis on surgical pathology. The subgroup with PNM < 9.3% comprised 19.6% of the study cohort (n = 69), and, in this subgroup, only six patients had ALN metastasis on surgical pathology. Thus, when using a PNM of < 9.3% to predict negative ALN, the FNR was 8.7% (6/69). The characteristics of these six patients with false negative PNM prediction are summarized in Table 4. All had small, low-grade, hormone receptor-positive tumors and non-suspicious axUS features.
Discussion
As tumor biology has taken precedence over anatomic staging for determining BC prognosis and need for adjuvant therapy, there has been growing interest in limiting the extent and morbidity of BC surgery. Increasingly, there is interest in omitting even SLNB in patients at low risk of harboring nodal metastasis,3,4,–5,10,11,–12 but limited information is available to define which patients are at lowest risk of occult nodal metastasis. In this study, we demonstrated that a preoperative ultrasound-based nomogram can accurately identify patients with < 10% likelihood of harboring ALN metastasis. We believe that this nomogram is a useful tool for surgeons as they seek to select appropriate patients for SLNB omission.
The Shantou nomogram was published in 2016 and showed good discrimination to predict the likelihood of ALN metastasis.7 However, it was unknown whether this nomogram would be useful in our ethnically heterogeneous patient population, characteristic of many North American community cancer centers, specifically for the use of identifying a subgroup of patients with < 10% likelihood of ALN metastasis. First, the Chinese population in which the nomogram was developed was presumably more ethnically homogeneous and not representative of our patient population. Additionally, the development cohort had more advanced disease than is characteristic of our patients. Furthermore, the nomogram has never been independently validated. Although a validation study was conducted in a Dutch population,9 the first author of both studies was the same. Independent validation was particularly important in this case, since ultrasound is a highly user-dependent modality. For all of these reasons, independent analysis of the nomogram was critical, both for overall validation and to determine whether the nomogram could be used in a typical North American community cancer center for the use we were interested in—identifying patients with a very low likelihood of ALN metastasis. In our cohort, the Shantou nomogram had fair predictive ability, but, impressively, was able to identify nearly 20% of our patients who had a < 9.3% risk of ALN metastasis with an FNR of 8.7%. This use of the nomogram has not been previously demonstrated.
In current practice, nomograms that predict ALN metastasis based on tumor characteristics have largely fallen out of favor, being replaced by imaging, either axUS or MRI, to assess the axilla preoperatively. However, imaging alone underestimates nodal disease, compared with the nomogram presented here. Previous studies have shown that a negative axUS alone has a 16–29%13,14,15,16,–17 FNR of predicting negative ALN. When a nomogram cut-off of < 9.3% was used to predict negative ALN, the FNR was 8.7%—substantially lower than shown with axUS alone. This FNR is similar to the average FNR of 8.4% that several studies8,18 have used as an acceptable FNR to accept SLNB for clinical situations in which ALND was previously the standard of care.
In our cohort, six patients had a false negative nomogram prediction, when a predicted likelihood of < 9.3% was used as the test cut-off. Each of these six patients had favorable tumor biology and early-stage disease (Table 4). Despite having a positive lymph node, current National Comprehensive Cancer Network guidelines would allow for multigene assay testing to determine the benefit of chemotherapy in these six node-positive patients. Additionally, in the CALGB 9343 study,4 patients in whom both axillary surgery and axillary radiation were omitted experienced only a 3% rate of axillary recurrence in 15-years of follow up. This suggests that if the nomogram was used to select patients for SLNB omission, the axillary recurrence rate due to missed opportunity for axillary radiation would be very low. Therefore, in patients with a very low likelihood of having ALN metastasis on the Shantou nomogram, performing a SLNB would likely not substantially affect local recurrence or overall survival.
The primary limitation of this study was its retrospective nature. At the RFBC, patients with suspicious breast imaging who undergo breast ultrasound also routinely undergo axUS. Although an image of any lymph node deemed suspicious is generally captured, the practice of image capture is not standardized. This is most likely to affect the measurement of the longest LN axis, as, in our practice, LN length is usually not considered in interpreting axUS since this feature has not been consistently associated with nodal positivity. Fortunately, the other axUS features used in the nomogram (cortical thickness, status of the hilum) are very likely to be captured in the recorded static images, since, in our practice, we do consider these morphologic features in determining if a lymph node is suspicious.
For patients with apparent early-stage BC, SLNB results often do not influence treatment recommendations. This can happen because the SLNB is negative or because similar care (e.g. genomic assay to determine adjuvant treatment) is offered regardless of a positive SLN result. In fact, a negative SLNB could be considered a non-therapeutic operation, since the finding of a negative SLN does not add to treatment options for a patient. Although SLNB for early-stage BC is the standard of care today, it is important that surgeons move the field forward, by looking for safe ways to eliminate non-therapeutic procedures. Currently, ongoing randomized controlled clinical trials are evaluating the impact of omission of SLNB in patients with early-stage BC. The SOUND trial,19 which has completed enrollment, randomized patients with cT1N0 BC and a negative axUS to SLNB versus no SLNB, with a primary endpoint of distant disease-free survival. The INSEMA trial20 is a non-inferiority study that is randomizing patients with cT1-2N0 disease to either SLNB versus no SLNB, with a primary endpoint of invasive disease-free survival after breast-conserving surgery. While awaiting the results of these trials, SLNB for patients with early-stage BC will remain the standard of care. However, for select patients, especially older patients or patients at high risk for lymphedema (e.g. obese patients), surgeons should initiate multidisciplinary discussions about the risk–benefit ratio of SLNB. We found that the preoperative ultrasound-based Shantou nomogram is a useful tool to inform such discussions. For patients with a nomogram value of predicted risk < 9.3%, it is unlikely that omission of SLNB would meaningfully affect survival. For such patients, if chemotherapy is not an option, or if multigene assay will be considered even in the setting of a positive SLNB, serious consideration should be given to omission of SLNB after appropriate patient counseling.
References
DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14(6):500–15.
Lucci A, McCall LM, Beitsch PD, et al. Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group trial Z0011. J Clin Oncol. 2007;25(24):3657–63.
Fisher B, Jeong J-H, Anderson S, Bryant J, Fisher ER, Wolmark N. Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. N Engl J Med. 2002;347(8):567–75.
Hughes KS, Schnaper LA, Bellon JR, et al. Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. J Clin Oncol. 2013;31(19):2382–87.
Martelli G, Boracchi P, De Palo M, et al. A randomized trial comparing axillary dissection to no axillary dissection in older patients with T1N0 breast cancer: results after 5 years of follow-up. Ann Surg. 2005;242(1):1–6.
Choosing Wisely. SSO – Sentinel node biopsy in node negative women 70 and over. 2016. Available at: http://www.choosingwisely.org/clinician-lists/sso-sentinel-node-biopsy-in-node-negative-women-70-and-over/. Accessed 19 Jun 2019.
Qiu SQ, Zeng HC, Zhang F, et al. A nomogram to predict the probability of axillary lymph node metastasis in early breast cancer patients with positive axillary ultrasound. Sci Rep. 2016;6:21196.
Lyman GH, Giuliano AE, Somerfield MR, et al. American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol. 2005;23(30):7703–20.
Qiu S-Q, Aarnink M, van Maaren MC, et al. Validation and update of a lymph node metastasis prediction model for breast cancer. Eur J Surg Oncol. 2018;44(5):700–07.
Martelli G, Miceli R, Daidone MG, et al. Axillary dissection versus no axillary dissection in elderly patients with breast cancer and no palpable axillary nodes: Results after 15 years of follow-up. Ann Surg Oncol. 2011;18(1):125–33.
Veronesi U, Orecchia R, Zurrida S, et al. Avoiding axillary dissection in breast cancer surgery: a randomized trial to assess the role of axillary radiotherapy. Ann Oncol. 2005;16(3):383–8.
Rudenstam CM, Zahrieh D, Forbes JF, et al. Randomized trial comparing axillary clearance versus no axillary clearance in older patients with breast cancer: first results of International Breast Cancer Study Group trial 10-93. J Clin Oncol. 2006;24(3):337–44.
Jackson RS, Mylander C, Rosman M, et al. Normal axillary ultrasound excludes heavy nodal disease burden in patients with breast cancer. Ann Surg Oncol. 2015;22(10):3289–95.
Schipper RJ, van Roozendaal LM, de Vries B, et al. Axillary ultrasound for preoperative nodal staging in breast cancer patients: is it of added value? Breast. 2013;22(6):1108–13.
Choi JS, Kim MJ, Moon HJ, Kim EK, Yoon JH. False negative results of preoperative axillary ultrasound in patients with invasive breast cancer: correlations with clinicopathologic findings. Ultrasound Med Biol. 2012;38(11):1881–6.
Johnson S, Brown S, Porter G, et al. Staging primary breast cancer. Are there tumour pathological features that correlate with a false-negative axillary ultrasound? Clin Radiol. 2011;66(6):497–9.
Stachs A, Göde K, Hartmann S, et al. Accuracy of axillary ultrasound in preoperative nodal staging of breast cancer—size of metastases as limiting factor. Springerplus. 2013;2(1):350.
Veronesi U, Panganelli G, Viale G, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med. 2003:546–53.
European Insitute of Oncology. Comparison of axillary sentinel lymph node biopsy versus no axillary surgery. ClinicalTrials.gov. 2015: Available at: https://clinicaltrials.gov/show/NCT02466737.
German Cancer Aid, German Breast Group. Comparison of axillary sentinel lymph node biopsy versus no axillary surgery (INSEMA). ClinicalTrials.gov. Available at: https://clinicaltrials.gov/ct2/show/NCT02466737.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Hanh-Tam Tran, Daina Pack, Charles Mylander, Laura Martino, Martin Rosman, Lorraine Tafra, and Rubie Sue Jackson have no financial disclosures to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tran, HT., Pack, D., Mylander, C. et al. Ultrasound-Based Nomogram Identifies Breast Cancer Patients Unlikely to Harbor Axillary Metastasis: Towards Selective Omission of Sentinel Lymph Node Biopsy. Ann Surg Oncol 27, 2679–2686 (2020). https://doi.org/10.1245/s10434-019-08164-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-08164-3