Abstract
Background
Gastric cancer treatment initiation is a complex process. Inefficiencies in care coordination can lead to significant delays, which are often more prominent at safety net hospitals. Multidisciplinary teams (MDTs) have been proposed as an effective solution.
Methods
A retrospective review of sequential gastric cancer patients receiving treatment at Parkland Hospital (Dallas, TX) between 2013 and 2015 was performed before (n = 50) and after (n = 50) creation of a MDT and standardized care pathways. Patients undergoing urgent resection were excluded. Time to treatment (TTT) from initial endoscopy to initiation of chemotherapy was evaluated. The number of diagnostic tests performed and treatment variability also were compared.
Results
Groups were similar in terms of age, sex, stage distribution, tumor location, and type of presentation (outpatient vs. emergency room). Post-intervention, TTT decreased from 84.1 ± 12.3 to 32.5 ± 15.2 days (p < 0.02). This decrease was primarily related to parallel performance of subspecialty evaluations, staging studies, and procedures. MDT review reduced the number of unnecessary staging tests performed, leading to a decrease in the average number of studies from 3.8 per patient to 2.2 (p < 0.05). Use of diagnostic laparoscopy in patients with clinically locally advanced disease increased from 18 to 94% (p < 0.05).
Conclusions
Creation of a gastric cancer MDT and uniform care pathways at a large safety net hospital expedited initiation of treatment, reduced unnecessary tests, and promoted consistent patient management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In 2018, an estimated 27,510 individuals were diagnosed with gastric cancer in the United States.1 While there have been notable improvements in 5-year survival rates, from 15% in 1975 to 29% in 2009, the disease remains one of poor prognosis and high mortality. Patients often have significant comorbidities, and the majority present with advanced disease.2 Workup and multidisciplinary management is complex, and inefficiencies in care coordination can result in significant treatment initiation delays. These delays may be even more significant at safety-net hospitals due to limited resources, socioeconomic barriers, and health disparities.3,4,5
Multidisciplinary teams (MDTs) and clinical care pathways have gained attention in recent years, both within the United States and internationally, as a strategy to streamline care delivery and reduce delays in treatment initiation. Several single-institution studies have demonstrated the effectiveness of MDTs in improving efficiency of care delivery, as well as clinical outcomes.6,7,8 However, the effectiveness of multidisciplinary teams has yet to be studied in the safety-net setting. In December 2014, we implemented a gastric cancer multidisciplinary team and standardized care pathway at Parkland Hospital, an 862-bed public safety net hospital in Dallas, Texas. Parkland Hospital is a county-based health system funded through taxpayer assessments and is charged with caring for residents of Dallas county that meet guidelines set forth by the county. The gastric cancer MDT reorganized and reprioritized existing resources in an attempt to eliminate unnecessary or repeat testing, increase consistency of patient care, and shorten time to treatment initiation. This retrospective study examines the impact of these changes at our institution.
Methods
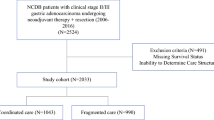
After receipt of Institutional Review Board approval, we conducted a retrospective analysis of 100 consecutive cases of newly diagnosed gastric cancer patients treated at Parkland Memorial Hospital, between January 2013 and May 2015. Patients receiving definitive or neoadjuvant chemotherapy were included. Patients treated before (n = 50) and after (n = 50) the creation of a multidisciplinary team (MDT) and standardized care pathways were selected. The MDT was a physician lead endeavor and consisted of faculty from medical oncology, surgical oncology, and gastroenterology. Given the resource constrained environment, no additional resources were available for the program and purposeful reorganization of resources and division of labor was carried out based on standard care pathways. After implementation of the MDT, patients were reviewed on a prospective basis and a unified care plan was implemented, which guided staging tests based on national guidelines, presentation, and review of imaging data.9 Surgical Oncology also began coordinating each patient’s care and expediting port placement and diagnostic laparoscopy. Patients were excluded if they required upfront urgent or emergent surgery to alleviate tumor related complications (e.g., obstruction, perforation, hemorrhage, or anemia) or did not initiate treatment (e.g., poor performance status, admitted directly to hospice). Data were collected on demographics (age, gender, and race), stage at diagnosis, presentation, and time to treatment (measured from the date of initial endoscopy to initiation of systemic therapy). Gastric cancer stage was categorized as early (T1-2N0), middle (TanyN1, T3-4Nx), and late stage (TanyNanyM1) according to the American Joint Committee on Cancer guidelines, 8th edition.10
Our primary endpoint of interest was time to treatment (TTT), defined as the number of days from initial endoscopy to initiation of systemic chemotherapy. Secondary endpoints included number of staging exams performed, variability of evaluation, and utilization of diagnostic laparoscopy in patients with clinically locally advanced disease and the absence of metastatic disease on axial imaging. Univariate analyses were performed using Chi square for categorical variables and analysis of variance or Kruskal–Wallis for continuous variables. Univariate linear regression was conducted to identify independent predictors of time to treatment. Independent variables with a significance level of P < 0.2 were included in a multivariate logistic regression model and were statistically significant at P < 0.05 in the multivariate model. All analyses were performed with SPSS (IBM Corp. Released 2017. IBM SPSS Statistics for Mac, Version 25.0. Armonk, NY).
Results
During a 20-month period, 124 patients were diagnosed with gastric adenocarcinoma and referred to the oncology program at Parkland Hospital. Of those, 117 referrals (94%) were internal. Patients requiring upfront resection related to obstruction or bleeding (n = 6) and those who did not received systemic therapy secondary to prohibitive functional status (n = 12), patient choice (n = 2), or hospice referral (n = 4) were excluded. The final cohort consisted of 100 consecutively treated patients, with 50 patients in the pre and post intervention groups. The median age of the patient cohort was 54.9 years, 72% were male, and the overwhelming majority were Hispanic (68%).
In assessing clinical stage, no patients in our study presented with early stage disease. Middle stage disease was most common (54%), but a significant proportion of patients (45%) presented with late-stage tumors. Two-thirds of our patients initially presented in the emergency department setting with symptomatic complaints, such as pain, bleeding, or obstruction related to the prevalence of late-stage tumors. There were no significant differences between pre- and postintervention groups regarding patient demographics (age, sex, race), clinical stage, tumor location, or setting of initial presentation (Table 1).
Prior to the implementation of the MDT, there were significant delays associated with treatment initiation related to the serial nature of the process which relied on completion of one task before initiation of the next. Figure 1 depicts this process and demonstrates the average time between key steps. Notable delays included prolonged wait times for interventional radiology and medical oncology.
Implementation of a multidisciplinary team led to a statistically significant decrease in TTT from 84.1 to 32.5 days (Table 2). While there was no difference in time from endoscopy to pathologic confirmation, time from endoscopy to completion of staging studies, referrals, port placement, and diagnostic laparoscopy all decreased significantly (p < 0.05). Additionally, the time from medical oncology visit to initiation of chemotherapy decreased from 62.3 ± 9.8 to 12.1 ± 4.3 days (p < 0.05; Fig. 1). After creation of the MDT, centralized coordination of services decreased the number of serial evaluations and allowed for multiple steps to be performed simultaneously (e.g., port placement at time of diagnostic laparoscopy).
MDT review also led to improved standardization in work-up and fewer unnecessary staging tests being performed (Table 3). Before MDT review, only 86% of patients received contrast enhanced staging CT chest/abdomen/pelvis scans. This number increased to 100% postintervention. In addition, the use of diagnostic laparoscopy in clinically locally advanced patients improved from 20% of patients to 94% (p < 0.05). The rate of detection of peritoneal disease by laparoscopy was similar in both groups (pre 40% vs. post 35%; p > 0.05). Although the formation of the MDT did not change the effectiveness of laparoscopy, it did have a dramatic impact on the appropriate utilization of laparoscopy. Clinical management was changed more often in the post-MDT group secondary to more accurate staging (8% vs. 24%, respectively; p < 0.05). Unnecessary testing, including the routine use of head CT/MRI and bone scans, was decreased (p < 0.05).
Discussion
Time to treatment is a composite quality measure of oncologic care that is affected by numerous factors, including institutional resources, regional practice patterns, and patient factors, including preference, and the treatment complexity related to the individual cancer type. Overall time to treatment initiation has increased over recent years and has been associated with an increase in mortality of 0.5–2.3% per week of delay in curative settings, such as early-stage breast, lung, and pancreas cancers.11,12,13
Gastric cancer is a heterogenous disease that requires integrated multidisciplinary care coordination to assure optimal outcomes.14 The use of neoadjuvant therapy in middle-stage disease has increased, requiring a higher level of coordination of staging studies and medical specialties, which is likely responsible for increasing TTT.2 Current time to treatment initiation for gastric cancer reported in nonsafety net hospitals is between 19 and 49 days and is associated with treatment sequencing, treatment facility designation, and cancer stage.11
Beyond the complexity of multidisciplinary gastric cancer care, safety-net hospitals face additional challenges related to patient access and inefficient care delivery secondary to limited hospital and patient resources, which may adversely increase TTT.15 In this study, we focused on patients that were able to access our safety net health system and attempted to address fragmentation of care and lack of parallel efficiencies through the implementation of an MDT and care pathways for patients with newly diagnosed gastric cancer.
Creation of a gastric cancer MDT resulted in significant improvements in TTT. Before our intervention, patients progressed through their workup in a serial fashion, where all steps in one stage were completed prior to moving on to the next (Fig. 1). For example, a patient evaluated with GI would not have their staging CT scans ordered until after pathologic confirmation was obtained. Serial steps led to significant aggregate delays, prolonging TTT. Postintervention, the care pathway promoted parallel efficiency through prospective case review to determine needed staging studies and treatment plan. The responsibility for coordination of these studies and diagnostic tests was consolidated within a single service with the greatest capacity. By streamlining care delivery into fewer service lines and developing professional relationships with ancillary services, we were able to decrease TTT from 84.1 to 32.5 days, which is in line with national averages.11,13 Additionally, by having the Surgical Oncology team place a port at the time of diagnostic laparoscopy, we obviated the need for patients to see another subspecialty service and undergo a second procedure which is often burdensome for patients with limited resources. There were a several fixed limitations in our system, such as infusion capacity for chemotherapy.
As an additional benefit, MDT review decreased variability in staging tests and increased the use of evidence-based assessment. Prior to implementation of a gastric cancer MDT, variable practice patterns encouraged the use of nonevidence-based tests, such as routine head CT/MRI and bone scans. Improved standardization and less variability were seen after implementation of the MDT. The use of EUS and PET scan decreased post-intervention. EUS use decreased as our patient population presented frequently with advanced and locally advanced disease where regional lymphadenopathy or advanced disease was apparent on cross-sectional imaging. In addition, PET scan was used more selectively given its low sensitivity in diffuse type cancers related to low baseline avidity.16 Importantly, diagnostic laparoscopy with biopsy/peritoneal lavage increased from 29 to 97% of patients with no evidence of distant disease on cross-sectional imaging. Diagnostic laparoscopy was critical in obtaining accurate pretreatment staging, as previous studies conducted at our institution showed that laparoscopy discovered occult disease in more than 30% of our high-risk patients.17 Although formation of the MDT did not alter the effectiveness of laparoscopy, it did dramatically increase the routine use in locally advanced patients which translated to more patients being accurately staged and having clinically appropriate care. Improved pretreatment staging accuracy allowed for more informed discussions regarding chemotherapeutic agent choice, improved operating room allocation efficiency due to decreased aborted laparotomy secondary to distant disease discovered on the day of surgery, and better ability to provide patients with realistic expectations.
As expected in a safety net hospital system caring for a high-risk, low-resource population, many of our patients presented with late-stage gastric cancers. Early detection of gastric cancer is difficult given the lack of standardized screening protocols in the Western hemisphere. This is further compounded by the lack of resources, increased barriers to access, and lower health literacy rates often found in safety net hospital patients. Our institutional goal is to utilize our gastric cancer MDT experience to identify ways to reach patients earlier in the disease process.
Our experience demonstrates that implementation of MDTs and care pathways in a safety net health system are feasible and potentially effective in reducing TTT and treatment variation. Although this project was instituted on a small scale, development of national pathways with MDT review in gastric cancer have been successful.7 However, given the retrospective format of this study, there are certain limitations. As a single-institution study with a unique set of patient demographics, barriers, and resource limitations, our results may not be widely generalizable. In addition, given the closed nature of our safety-net hospital system, the great majority of the referrals were internal. This is not common of other published data regarding TTT where inefficiencies are related to fragmentation of care relate to gathering of outside information.
Conclusions
Inefficiencies exist in the delivery of cancer care at safety-net hospitals. Many of these inefficiencies are related to lack of standardization and coordination between subspecialties involved. Implementation of an MDT led to expedited time to initiation of chemotherapy, fewer unnecessary staging tests, and increased treatment consistency. Quality of care also was improved due increased use of evidence-based tests and more accurate pretreatment staging accuracy secondary to more consistent diagnostic laparoscopy use.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34. https://doi.org/10.3322/caac.21551.
Mokdad A, Ali A, Nassour I, et al. Treatment trends in gastroesophageal and gastric cancers in the United States. J Clin Oncol. 2017;35:136. https://doi.org/10.1200/jco.2017.35.4_suppl.136.
Morgan R, Cassidy M, DeGeus SW, Tseng J, McAneny D, Sachs T. Presentation and survival of gastric cancer patients at an urban academic safety-net hospital. J Gastrointest Surg. 2019;23:239–46. https://doi.org/10.1007/s11605-018-3898-3.
Millas SG, Alawadi ZM, Wray CJ, et al. Treatment delays of colon cancer in a safety-net hospital system. J Surg Res. 2015;198:311–6. https://doi.org/10.1016/j.jss.2015.03.078.
Millas SG, Wray C, Alawadi Z, et al. Treatment of colon cancer in a safety-net hospital system: where are the delays? J Surg Res. 2014;186:505. https://doi.org/10.1016/j.jss.2013.11.216.
Di L, Wu H, Zhu R, et al. Multi-disciplinary team for early gastric cancer diagnosis improves the detection rate of early gastric cancer. BMC Gastroenterol. 2017;17:147. https://doi.org/10.1186/s12876-017-0711-9.
Groene O, Chadwick G, Riley S, et al. Re-organisation of oesophago-gastric cancer services in England and Wales: a follow-up assessment of progress and remaining challenges. BMC Res Notes. 2014;7:24. https://doi.org/10.1186/1756-0500-7-24.
MacDermid E, Hooton G, MacDonald M, McKay G, Grose D, Mohammed N, Porteous C. Improving patient survival with the colorectal cancer multi-disciplinary team. Colorectal Dis. 2009;11:291–5. https://doi.org/10.1111/j.1463-1318.2008.01580.x.
Ajani JA, D’Amico TA, Almhanna K, et al. Gastric cancer, version 3.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2016;14:1286–312. https://doi.org/10.6004/jnccn.2016.0137.
Ajani JA, In H, Sano T, et al. AJCC cancer staging manual. New York: Springer; 2016. p. 203–20. https://doi.org/10.1007/978-3-319-40618-3_17.
Bilimoria KY, Ko CY, Tomlinson JS, et al. Wait times for cancer surgery in the United States. Ann Surg. 2011;253:779–85. https://doi.org/10.1097/sla.0b013e318211cc0f.
Murphy CT, Galloway TJ, Handorf EA, et al. Survival impact of increasing time to treatment initiation for patients with head and neck cancer in the United States. J Clin Oncol. 2015;34:169–78. https://doi.org/10.1200/jco.2015.61.5906.
Khorana AA, Tullio K, Elson P, et al. Time to initial cancer treatment in the United States and association with survival over time: an observational study. PLoS ONE. 2019;14:e0213209. https://doi.org/10.1371/journal.pone.0213209.
Sanjeevaiah A, Cheedella N, Hester C, Porembka MR. Gastric cancer: recent molecular classification advances, racial disparity, and management implications. J Oncol Pract. 2018;14:217–24. https://doi.org/10.1200/jop.17.00025.
Zaidi MY, Rappaport JM, Ethun CG, et al. Identifying the barriers to gastric cancer care at safety-net hospitals: a novel comparison of a safety-net hospital to a neighboring quaternary referral academic center in the same healthcare system. J Surg Oncol. 2019;119:64–70. https://doi.org/10.1002/jso.25299.
Lehmann K, Eshmuminov D, Bauerfeind P, et al. 18FDG-PET-CT improves specificity of preoperative lymph-node staging in patients with intestinal but not diffuse-type esophagogastric adenocarcinoma. Eur J Surg Oncol EJSO. 2017;43:196–202. https://doi.org/10.1016/j.ejso.2016.08.020.
Nassour I, Fullington H, Hynan LS, et al. The yield of staging laparoscopy in gastric cancer is affected by racial and ethnic differences in disease presentation. Ann Surg Oncol. 2017;24:1787–94. https://doi.org/10.1245/s10434-017-5805-7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
None of the authors have conflicts of interest to disclose. SCW is a Disease Oriented Clinical Scholar at UTSW. MRP is a Dedman Family Scholar in Clinical Care at UTSW.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ju, M., Wang, S.C., Syed, S. et al. Multidisciplinary Teams Improve Gastric Cancer Treatment Efficiency at a Large Safety Net Hospital. Ann Surg Oncol 27, 645–650 (2020). https://doi.org/10.1245/s10434-019-08037-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-08037-9