Abstract
Background
Among numerous systemic inflammatory biomarkers, it remains unclear which is the most prognostic for patients with stage II/III colon cancer. We aimed to compare the prognostic significance of systemic inflammatory biomarkers among patients with stage II/III colon cancer.
Methods
We included 1303 patients with stage II/III colon cancer who underwent potentially curative resection from July 2004 to December 2013. Sixteen systemic inflammatory biomarkers—derived from combinations of neutrophils, lymphocytes, monocytes, platelets, C-reactive protein (CRP), and albumin—were compared to identify the biomarker most associated with overall survival (OS) and disease-free survival (DFS) using receiver operating characteristic (ROC) curve analysis.
Results
Nine inflammatory biomarkers were predictive for OS, among which lymphocyte-to-CRP ratio (LCR), CRP-to-albumin ratio (CAR), neutrophil × CRP, monocyte × CRP, and platelet × CRP were also predictive for DFS. Among these five inflammatory biomarkers, the area under the curve (AUC) value was highest (0.630) for LCR, being significantly higher than that for neutrophil × CRP (P = 0.010), monocyte × CRP (P = 0.007), or platelet × CRP (P = 0.010) for OS. When the prognostic impact of LCR and CAR were analyzed by multivariate analysis, only LCR was an independent predictor of both OS [hazard ratio (HR), 1.77; 95% confidence interval (CI), 1.23–2.60; P = 0.002] and DFS (HR, 1.29; 95% CI, 1.00–1.66; P = 0.048).
Conclusions
LCR may be the most useful predictive factor for OS and DFS in patients with stage II or III colon cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Colorectal cancer is the third leading cause of cancer death in the world.1 Although surgical procedures and chemotherapy have improved, relapse after curative resection and mortality from colorectal cancer remain high. The tumor–node–metastasis (TNM) stage is widely recognized as the primary prognostic factor, but it is not precise, especially in patients with localized disease.2 Therefore, it is necessary to identify which patients have high possibility of recurrence, and which biomarker is most associated with poor survival.
In patients with stage I–IV colorectal cancer, preoperative systemic inflammatory response is generally predictive of disease progression and outcomes,3 with numerous serum systemic inflammatory biomarkers and other indices associated with poor outcomes: blood neutrophil-to-lymphocyte ratio (NLR),4,5 lymphocyte-to-monocyte ratio (LMR),6 platelet-to-lymphocyte ratio (PLR),7 C-reactive protein (CRP)-to-albumin ratio (CAR),8 modified Glasgow prognostic score (mGPS),9,10,11,12 systemic inflammation score (SIS),13 and prognostic nutritional index (PNI).14 Patients with stage IV colorectal cancer who also present with an inflammatory response carry tumors with more aggressive biological behavior and a higher rate of recurrence.15 However, the relation between systemic inflammatory response and prognosis in patients with stage II or III colon cancer is not well defined. Furthermore, it is unclear which systemic inflammatory biomarker is most associated with prognosis.
The aim of this study is to compare various preoperative systemic inflammatory biomarkers in terms of prognostic significance in a cohort of patients with stage II or III colon cancer undergoing curative resection.
Patients and Methods
Study Population
From July 2004 to December 2013, 1449 patients with pathological stage II or III colon cancer, including rectosigmoid cancer, underwent elective curative resection at the Department of Gastroenterological Surgery of the Cancer Institute Hospital (CIH). The exclusion criteria were preoperative chemotherapy or radiation (n = 16), bowel obstruction (n = 11), multiple cancers (n = 75), neuroendocrine carcinoma (n = 4), and inadequate records of biomarkers (n = 40). Finally, 1303 patients were included in the present study. Tumors were staged according to the 7th edition of the American Joint Committee on Cancer (AJCC) Cancer staging manual.16 Ethical approval for this study was granted by the Ethics Committee of the CIH (reference no. 2016-1090).
Serum Inflammatory Markers
Counts of whole white blood cells, neutrophils, lymphocytes, monocytes, and platelets, as well as levels of C-reactive protein (CRP) and albumin were recorded within a 30-day period before surgery. Inflammatory response is characterized by an increase in the proportion of neutrophils, monocytes, platelets, and CRP (i.e., inflammatory parameters) and a decrease in the proportion of lymphocytes and albumin (i.e., antiinflammatory parameters).17 Thus, when any two of these six serum inflammatory and antiinflammatory parameters are assessed together, there is a total of 15 possible combinations (Table 1). When the grouped serum parameters are both inflammatory or both antiinflammatory, they are multiplied; when there is one from each group, they are divided. In addition, PNI was calculated as albumin (g l−1) + 0.005 × total lymphocyte count.14 Among the 16 inflammatory biomarkers listed in Table 1, six systemic inflammatory biomarkers are well characterized as markers: NLR, LMR, PLR, CAR, PNI, and lymphocyte-to-CRP ratio (LCR).18
Survival Data
Data regarding patient survival were collected and used to calculate patient overall survival (OS), defined as time from date of first surgery to date of death from any cause. Data regarding disease recurrence were collected from radiological, histopathological, and endoscopic records. Disease-free survival (DFS) was defined as time from date of first surgery to date on which disease recurrence, either local or distant, was first detected or death from any cause. Those patients who experienced no events were censored at last follow-up. The follow-up protocol was standardized within the Colorectal Surgery Department at CIH: patients were tested for tumor markers every 3 months during the first 3 years then every 6 months thereafter; computed tomography (chest to pelvis) was performed every 6 months for 5 years.
Statistical Analysis
Data are presented as median (range) for continuous variables and number of patients (percentage) for categorical variables. Continuous variables were compared using the Mann–Whitney U-test, and categorical variables were compared using Fisher’s exact test. Receiver operating characteristic (ROC) curves for OS and DFS were analyzed for each inflammatory biomarker, with the Youden index used to determine the cut-off value. Two ROC curves were compared using the DeLong test and bootstrap test.19 Survival analysis was performed using the Kaplan–Meier method with the log-rank test. Univariate and multivariate Cox proportional hazard models were used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs). All statistical analyses were performed using GraphPad Prism 7 software (GraphPad, San Diego, CA), JMP software V 10.0.2 (SAS Institute Inc.; Cary, NC), or R software v3.5.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient Characteristics
The clinicopathological features of patients enrolled in this study are summarized in Table 2. The patient group included 689 men and 614 women with median age of 65 years (range 26–93 years). The median pretreatment CEA was 3.0 (range 0.5–31.3). The tumor was located on the left side in 61% of patients. About 50% of patients were stage II, and 46.1% of patients underwent adjuvant chemotherapy.
ROC Curve Analysis for OS and DFS
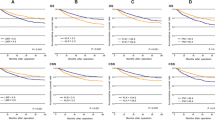
The median follow-up period for survivors was 60.2 months (range 3–106 months; interquartile range 50.7–65.7 months). There were 139 deaths and 224 recurrences. The five-year OS and DFS for the entire cohort were 89.5% and 79.3%, respectively. Among 16 inflammatory biomarkers, only five (CAR, LCR, neutrophil × CRP, monocyte × CRP, and platelet × CRP) had significantly higher area under the curve (AUC) values (> 0.5) in predicting DFS (Fig. 1). In predicting OS, these five biomarkers as well as four additional biomarkers (NLR, LMR, PNI, and lymphocyte × Alb) had significantly higher AUC (> 0.5) in predicting OS (Fig. 2), with LCR having the highest AUC value (0.630). We then compared the AUC values for LCR with another four biomarkers that were potential predictors for both OS and DFS (Fig. 3). Using the DeLong test, the AUC value for LCR was significantly higher than that for neutrophil × CRP (P = 0.0097), monocyte × CRP (P = 0.0072), and platelet × CRP (P = 0.0103), and tended to be higher than that for CAR (P = 0.1248). We performed 2000 bootstrap replicates and obtained similar P values (0.0092 for LCR versus neutrophil × CRP; 0.0065 for LCR versus monocyte × CRP; 0.011 for LCR versus platelet × CRP; and 0.1229 for LCR versus CAR). In contrast, the AUC value for CAR was not significantly different from that of neutrophil × CRP (P = 0.1387) or platelet × CRP (P = 0.0600) (DeLong test, data not shown). Subsequent analyses were focused on LCR and CAR, with optimal cut-offs for DFS of 12,980 for LCR and 0.02558 for CAR. Under these cut-offs, the sensitivity and specificity of LCR were 58.2% and 53.7%, respectively for predicting DFS, and 69.1% and 53.7%, respectively, for predicting OS. Likewise, the sensitivity and specificity of CAR were 64.0% and 46.8%, respectively, for predicting DFS, and 72.7% and 46.7%, respectively, for predicting OS (Figs. 1, 2).
Receiver operating characteristic curve analysis to evaluate the predictive value of 16 inflammatory biomarkers for overall survival (OS). Nine biomarkers were predictive of OS, including the five inflammatory biomarkers that were predictive for disease-free survival and four others. Lymphocyte-to-C-reactive protein ratio (LCR) had the highest area under the curve value
Comparison of receiver operating characteristic curve (ROC) analysis for overall survival (OS). Among five inflammatory biomarkers predictive for disease-free survival (DFS), the area under the curve value for lymphocyte-to-C-reactive protein ratio (LCR; yellow) was significantly higher than that for other inflammatory biomarkers (all in blue), except C-reactive protein (CRP)-to albumin ratio (CAR)
Correlation Between Clinicopathological Factors and LCR or CAR
Table 3 summarizes the association between clinicopathological factors and LCR or CAR. High LCR (> 12,980) and low CAR (≤ 0.02558) were significantly associated with younger age, female sex, lower CEA levels (< 5), less undifferentiated histology, reduced pT4 rates, and higher percentage of lymph node metastasis and adjuvant chemotherapy. LCR and CAR were also significantly associated with each other.
Relationship Between LCR or CAR and Survival
Kaplan–Meier survival curves according to LCR or CAR status are summarized in Fig. 4. Patients with low LCR (≤ 12,980) had significantly worse OS (Fig. 4a; P < 0.0001) and DFS (Fig. 4b; P = 0.0011) than patients with high LCR (> 12,980). Patients with high CAR (> 0.02558) had significantly worse OS (Fig. 4c; P < 0.0001) and DFS (Fig. 4d; P = 0.0045) than patients with low CAR (≤ 0.02558). The univariate and multivariate analyses for the clinicopathological factors, including LCR and survival, are summarized in Table 4. Age, male sex, pathology (poorly differentiated or mucinous adenocarcinoma), pT4, lymph node metastasis, lymphovascular invasion, and low LCR (≤ 12,980) were associated with OS on univariate analysis. Age, male sex, pathology (poorly differentiated or mucinous adenocarcinoma), pT4, lymph node metastasis, lymphovascular invasion, no adjuvant chemotherapy, and low LCR (HR, 1.77; 95% CI, 1.23–2.60; P = 0.002) were independent predictors of worse OS on multivariate analysis. On univariate analysis, worse DFS was associated with male sex, pathology (poorly differentiated or mucinous adenocarcinoma), pT4, lymph node metastasis, lymphovascular invasion, number of lymph nodes retrieved < 12, and low LCR. On multivariate analysis, male sex, pT4, lymph node metastasis, no adjuvant chemotherapy, and low LCR (HR, 1.29; 95% CI, 1.00–1.66; P = 0.048) were independent predictors of worse DFS. High CAR (> 0.02558) was also an independent predictor of worse OS on multivariate analysis (HR, 1.80; 95% CI, 1.24–2.68; P = 0.002), but CAR was only marginally associated with worse DFS (HR, 1.28; 95% CI, 0.99–1.66; P = 0.0576) (data not shown).
Discussion
We compared the prognostic value of 16 systemic inflammatory biomarkers, including six existing inflammatory biomarkers, in 1303 patients with stage II or III colon cancer. Although we showed that nine inflammatory biomarkers were predictive for OS, only five were predictive for both OS and DFS. LCR had the highest accuracy to predict OS and was the only biomarker that was an independent predictor of both OS and DFS. To the best of the authors’ knowledge, this is the largest study to comprehensively compare the prognostic value of various inflammatory biomarkers, including previously published and new inflammatory biomarkers.
Systemic inflammation plays a crucial role in promoting cancer progression.17 Proinflammatory cytokines, such as tumor necrosis factor (TNF)-α and interleukin (IL)-1, IL-6, and IL-8, are upregulated as part of the inflammatory response. These cytokines activate intracellular pathways, such as those mediated by nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), and modulate cellular proliferation and angiogenesis.5 IL-6 induces synthesis of acute-phase proteins, including CRP, and decreases albumin production in the liver.20 Platelet counts may be elevated in response to proinflammatory cytokines, and they are also considered to regulate tumor angiogenesis by releasing vascular endothelial growth factor.21 Proinflammatory cytokines also mediate recruitment of circulating myeloid cells to the tumor, and CD8+ T-cells are decreased due to direct or indirect immunosuppression by intratumor myeloid cells.22 Thus, systemic inflammation is typically characterized by an increase in circulating neutrophils and monocytes and a decrease in circulating lymphocytes.23
Many previous studies have shown that systemic inflammatory biomarkers are independent prognostic factors in colorectal cancer. However, some studies focused solely on patients with stage IV cancer,15,24,25,26,27 while others included patients with stage I or stage IV cancer.6,11,13,28,29,30,31 There are few studies focusing on serum inflammatory biomarkers in patients with stage II/III colon cancer. We included only patients with stage II or III colon cancer, because accurate prediction of prognosis in this cohort might help to guide the decision regarding whether to use adjuvant chemotherapy and determine whether strict follow-up is necessary. Furthermore, the treatment strategy for stage IV colon cancer is more complicated than that for stage II/III colon cancer, and the incidence of recurrence is much higher, indicating the need to consider stage IV colon cancer patients separately. In this study, we showed that NLR, LMR, and PNI were predictive for OS but not DFS. Our results are different from those in the previous study by Li et al., which identified NLR and LMR as independent predictors of DFS in 5336 stage I–III colorectal cancer patients.28 This difference could be due to our exclusion of patients with stage I cancer, or a much higher 5-year DFS in the present study (79.3% vs 56.0%). Tokunaga et al. reported that PNI was an independent predictor of both OS and relapse-free survival in 468 stage I–III patients, but those authors did not analyze adjuvant chemotherapy as a covariate in the multivariate analysis.31
Our study shows that five inflammatory biomarkers, including CAR and LCR, were predictive for both OS and DFS. It is worth noting that CRP was part of all five of these biomarkers. Our results suggest that CRP is a key predictive factor for OS and DFS among patients with stage II/III colon cancer, and that, among patients with stage II/III colon cancer, inflammatory biomarkers incorporating CRP (CRP × neutrophil, CRP × monocyte, or CRP × platelet) might be more useful predictors than the well-studied, existing biomarkers, such as NLR, LMR, PLR, and PNI. Our study also shows that, among the 16 systemic inflammatory biomarkers, LCR had the highest AUC value for predicting OS, and only LCR was an independent predictor for both OS and DFS. LCR is a relatively new inflammatory biomarker reported by Okugawa et al.18 In that study, the authors compared nine inflammatory biomarkers in a discovery cohort of 373 patients with stage I–IV colorectal cancer, and showed that LCR was the most useful predictor of OS and DFS.18 Although their cut-off value of LCR (6000) was different from the one used in the present study (12,980)—potentially explained by differences in patient inclusion criteria (stage I and IV colorectal cancer and rectal cancer)—our data also suggest that LCR is the most sensitive inflammatory biomarker in a cohort of stage II/III colon cancer.
There are several limitations to this study. First, it was a retrospective, single-institutional study. So, it may have been subject to selection bias. However, few of our records were missing biomarker data, which might be a strength of this study. Second, we did not investigate the association of systemic inflammatory biomarkers with pathological findings, such as tumor infiltrating neutrophils, lymphocytes, monocytes, etc. Third, we did not validate the prediction model using external data, and we therefore need to check our prediction model against external data in the future. Finally, we have no data pertaining to perineural invasion32 or budding.33 These factors are reported to be associated with worse prognosis in colorectal cancer, and their inclusion as a factor might improve the baseline prediction model.
In conclusion, the results of the present study show that, among the 16 systemic inflammatory biomarkers, LCR could be used to predict OS and DFS in patients with stage II and III colon cancer.
References
Edwards BK, Noone AM, Mariotto AB, et al. Annual Report to the Nation on the status of cancer, 1975-2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2014;120:1290–1314.
Benson AB, 3rd, Venook AP, Cederquist L, et al. Colon cancer, version 1.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2017;15:370–398.
Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010;6:149–163.
Shibutani M, Maeda K, Nagahara H, et al. The prognostic significance of a postoperative systemic inflammatory response in patients with colorectal cancer. World J Surg Oncol. 2015;13:194.
Pine JK, Morris E, Hutchins GG, et al. Systemic neutrophil-to-lymphocyte ratio in colorectal cancer: the relationship to patient survival, tumour biology and local lymphocytic response to tumour. Br J Cancer. 2015;113:204–211.
Chan JC, Chan DL, Diakos CI, et al. The lymphocyte-to-monocyte ratio is a superior predictor of overall survival in comparison to established biomarkers of resectable colorectal cancer. Ann Surg. 2017;265:539–546.
Zou ZY, Liu HL, Ning N, Li SY, Du XH, Li R. Clinical significance of pre-operative neutrophil lymphocyte ratio and platelet lymphocyte ratio as prognostic factors for patients with colorectal cancer. Oncol Lett. 2016;11:2241–2248.
Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Shibuya N, Kubota K. Clinical significance of the C-reactive protein to albumin ratio for survival after surgery for colorectal cancer. Ann Surg Oncol. 2016;23:900–907.
Guthrie GJ, Roxburgh CS, Farhan-Alanie OM, Horgan PG, McMillan DC. Comparison of the prognostic value of longitudinal measurements of systemic inflammation in patients undergoing curative resection of colorectal cancer. Br J Cancer. 2013;109:24–28.
McMillan DC. The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39:534–540.
Park JH, Watt DG, Roxburgh CS, Horgan PG, McMillan DC. Colorectal cancer, systemic inflammation, and outcome: staging the tumor and staging the host. Ann Surg. 2016;263:326–336.
Koike Y, Miki C, Okugawa Y, et al. Preoperative C-reactive protein as a prognostic and therapeutic marker for colorectal cancer. J Surg Oncol. 2008;98:540–544.
Suzuki Y, Okabayashi K, Hasegawa H, et al. Comparison of preoperative inflammation-based prognostic scores in patients with colorectal cancer. Ann Surg. 2018;267:527–531.
Park BK, Park JW, Han EC, et al. Systemic inflammatory markers as prognostic factors in stage IIA colorectal cancer. J Surg Oncol. 2016;114:216–221.
Gomez D, Morris-Stiff G, Wyatt J, Toogood GJ, Lodge JP, Prasad KR. Surgical technique and systemic inflammation influences long-term disease-free survival following hepatic resection for colorectal metastasis. J Surg Oncol. 2008;98:371–376.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging manual. 7th edn. New York: Springer; 2010.
Rossi S, Basso M, Strippoli A, et al. Are markers of systemic inflammation good prognostic indicators in colorectal cancer? Clin Colorectal Cancer. 2017;16:264–274.
Okugawa Y, Toiyama Y, Yamamoto A, et al. Lymphocyte-C-reactive protein ratio as promising new marker for predicting surgical and oncological outcomes in colorectal cancer. Ann Surg. (2019). https://doi.org/10.1097/sla.0000000000003239.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845.
Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Kubota K. Combination of platelet count and neutrophil to lymphocyte ratio is a useful predictor of postoperative survival in patients with colorectal cancer. Br J Cancer. 2013;109:401–407.
Zhu Y, Zhou S, Liu Y, Zhai L, Sun X. Prognostic value of systemic inflammatory markers in ovarian Cancer: a PRISMA-compliant meta-analysis and systematic review. BMC Cancer. 2018;18:443.
Shinko D, Diakos CI, Clarke SJ, Charles KA. Cancer-related systemic inflammation: the challenges and therapeutic opportunities for personalized medicine. Clin Pharmacol Ther. 2017;102:599–610.
Dupre A, Malik HZ. Inflammation and cancer: What a surgical oncologist should know. Eur J Sur Oncol. 2018;44:566–570.
Tang H, Li B, Zhang A, Lu W, Xiang C, Dong J. Prognostic significance of neutrophil-to-lymphocyte ratio in colorectal liver metastasis: a systematic review and meta-analysis. PLoS ONE. 2016;11:e0159447.
Wu Y, Li C, Zhao J, et al. Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios predict chemotherapy outcomes and prognosis in patients with colorectal cancer and synchronous liver metastasis. World J Surg Oncol. 2016;14:289.
Thomsen M, Kersten C, Sorbye H, et al. Interleukin-6 and C-reactive protein as prognostic biomarkers in metastatic colorectal cancer. Oncotarget. 2016;7:75013–75022.
Shibutani M, Maeda K, Nagahara H, et al. Prognostic significance of the lymphocyte-to-monocyte ratio in patients with metastatic colorectal cancer. World J Gastroenterol. 2015;21:9966–9973.
Li Y, Jia H, Yu W, et al. Nomograms for predicting prognostic value of inflammatory biomarkers in colorectal cancer patients after radical resection. Int J Cancer. 2016;139:220–231.
Choi WJ, Cleghorn MC, Jiang H, Jackson TD, Okrainec A, Quereshy FA. Preoperative neutrophil-to-lymphocyte ratio is a better prognostic serum biomarker than platelet-to-lymphocyte ratio in patients undergoing resection for nonmetastatic colorectal cancer. Ann Surg Oncol. 2015;22 Suppl 3:S603–S613.
Jiang H, Tang E, Xu D, et al. Development and validation of nomograms for predicting survival in patients with non-metastatic colorectal cancer. Oncotarget. 2017;8:29857–29864.
Tokunaga R, Sakamoto Y, Nakagawa S, et al. Comparison of systemic inflammatory and nutritional scores in colorectal cancer patients who underwent potentially curative resection. Int J Clin Oncol. 2017;22:740–748.
Knijn N, Mogk SC, Teerenstra S, Simmer F, Nagtegaal ID. Perineural invasion is a strong prognostic factor in colorectal cancer: a systematic review. Am J Surg Pathol. 2016;40:103–112.
Ueno H, Murphy J, Jass JR, Mochizuki H, Talbot IC. Tumour ‘budding’ as an index to estimate the potential of aggressiveness in rectal cancer. Histopathology. 2002;40:127–132.
Acknowledgment
This work was supported by a grant-in-aid of the Public Trust Fund for Clinical Cancer Research, and JSPS KAKENHI under Grant Nos. 18K08664 and 18K08635.
Author information
Authors and Affiliations
Contributions
SS and TA designed the study and wrote the manuscript. SS, TA, TT, TN, YF, and MU contributed to data collection. SS, TA, KO, and FO contributed to the analysis and interpretation of data. All authors contributed to analysis and interpretation of data. All authors critically reviewed the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflicts of interest for this article.
Approval of Research Protocol
This retrospective research protocol was approved by the Institutional Review Board of Cancer Institute Hospital (Reference No. 2016-1090), and it conforms to the provisions of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suzuki, S., Akiyoshi, T., Oba, K. et al. Comprehensive Comparative Analysis of Prognostic Value of Systemic Inflammatory Biomarkers for Patients with Stage II/III Colon Cancer. Ann Surg Oncol 27, 844–852 (2020). https://doi.org/10.1245/s10434-019-07904-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07904-9