Abstract
Background
Survival in peritoneal dissemination from appendiceal cancer after complete cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (CRS/HIPEC) varies within each histopathologic subtype. Analyzing patients with unique responses may uncover the mechanisms behind their extreme outcomes. We proposed a method to identify retrospectively and to characterize patients who responded exceptionally well or very poorly within each histopathologic subtype.
Methods
Retrospective review of patients with low-grade mucinous carcinoma peritonei (LGMCP), high-grade MCP (HGMCP), and HGMCP with signet ring cells (HGMCP-S) with complete CRS/HIPEC (CC-0/1) was performed. Patients were divided by recurrence status. Median follow-up was calculated for each. Exceptional responders (ExR) were defined as alive without recurrence after median follow-up of the nonrecurrent group. Poor responders (PoR) were defined as disease recurrence before median follow-up of the recurrent group. Perioperative characteristics were analyzed.
Results
LGMCP, HGMCP, and HGMCP-S had 48 (41%), 19 (23%), and 7 (14%) ExR and 11 (10%), 20 (24%), and 20 (39%) PoR, respectively. All ExR had lower median PCI (26 vs. 36 [p = 0.004]; 13 vs. 33.5 [p < 0.001]; 3 vs. 29.5 [p = 0.001]). Fewer LGMCP and HGMCP ExR had abnormal tumor markers (36% vs. 90% [p = 0.003]; 22% vs. 74% [p = 0.003]). More HGMCP and HGMCP-S ExR had CC-0 (vs. CC-1) cytoreductions (84% vs. 50%, p = 0.041; 100% vs. 40%, p = 0.008).
Conclusions
Stratifying patients by recurrence status and follow-up time successfully selects ExR and PoR within each histopathologic subtype. Perioperative characteristics of ExR versus PoR differ across histopathologic subtypes, except for disease burden. Genetic analysis may further elucidate differences and aid in the development of novel targeted therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Peritoneal dissemination (PD) from appendiceal cancer (AC) is a rare and advanced gastrointestinal neoplasm with unique clinical and biological behavior, distinct from colorectal cancer.1,2,3 Mucinous tumors of the appendix are morphologically and clinically diverse, ranging from low-grade mucinous carcinoma peritonei (LGMCP), high-grade mucinous carcinoma peritonei (HGMCP), and HGMCP with signet ring cells (HGMCP-S).4,5,6 Currently, cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (CRS/HIPEC) is the treatment of choice for PD from AC.7
Treatment response varies not only according to histopathologic subtype but also quality of cytoreduction.8,9 However, even when a complete cytoreduction is achieved, there are still patients within each histopathologic subtype who respond exceptionally well or very poorly after CRS/HIPEC.
Identifying patients with PD from AC who responded exceptionally well or very poorly after CRS/HIPEC is essential to understand patient outcomes, enhance patient selection, offer personalized treatment, and avoid unnecessary treatments. In this study, we suggest a method to retrospectively identify and describe the complete clinical profile of exceptional and poor responders within each histopathologic subtype after complete CRS/HIPEC.
Patient and Methods
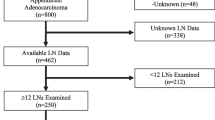
A retrospective review of a prospective institutional database with 673 CRS/HIPEC procedures from 1998 to 2017 was performed. A total of 368 patients had PD from AC with ECOG performance status between 0 and 2 and no evidence of extraperitoneal disease. Only data from the first CRS/HIPEC was analyzed.
Perioperative Management
Preoperatively, imaging (CT scan or MRI) and/or diagnostic laparoscopy were used to identify candidates for CRS/HIPEC. Preoperative CEA, CA-125, and CA 19-9 were elevated if > 5 ng/mL, 35 U/mL, and 37 U/mL, respectively.
Intraoperatively, peritoneal cancer index (PCI) was assessed with PCI ≥ 20 considered high disease burden.10 Resections were performed to reduce tumor to microscopic levels. Completeness of cytoreduction (CC) score was recorded (CC-0: no residual tumor, CC-1: tumor nodules < 2.5 mm, CC-2/3: tumor nodules ≥ 2.5 mm).10 HIPEC was performed using the closed technique with 40 mg of mitomycin-C at 41–42 °C for 90 min. After perfusion, gastrointestinal anastomoses were completed and chest tubes placed if indicated.
Postoperatively, patients were transferred to the ICU for 24 h and then to the inpatient oncology unit when clinically stable. Specific details on the management of these patients were published previously by our group.11 Surveillance included physical exam, imaging, and tumor markers every 6 months for 5 years and yearly thereafter until year 10. After 10 years, annual physical exams were performed. Recurrence was considered if there was evidence on imaging, rising/abnormal tumor markers, and/or clinical presentation (e.g., bowel obstruction).
Exceptional and Poor Responder Selection
Patients with complete cytoreduction (CC-0/1) were categorized by histopathologic subtype according to the Peritoneal Surface Oncology Group International expert panel consensus.6 Only patients with mucinous adenocarcinoma, including LGMCP, HGMCP, and HGMCP-S, were considered.
In order to find outlier patients, each histopathologic subtype was further divided by recurrence status (recurrence vs. nonrecurrence). Median follow-up for recurrent and nonrecurrent groups was calculated separately for each subtype. Follow-up time was calculated from the date of CRS/HIPEC to the last contact date or date of death. Exceptional responders (ExR) never had recurrence and had a follow-up time greater than the median follow-up of the nonrecurrent group. Poor responders (PoR) recurred before the median follow-up of the recurrent group (Fig. 1).
For each histopathologic subtype, two scatter plots (nonrecurrent and recurrent groups) of the surgery date versus follow-up time, because CRS/HIPEC were constructed to visualize ExR and PoR. Each point represents one patient and their current status.
Statistical Analysis
Perioperative variables were compared between ExR and PoR within each histopathologic subtype.12 Complications were graded according to Clavien-Dindo.13 Only patients proven to be an exceptional or poor responder were analyzed. Patients who recently underwent CRS/HIPEC or who recurred after a very long time were excluded (intermediate responders [InR]).
Chi square test or Fisher’s exact test assessed differences between categorical variables. Independent sample Student’s t test and Mann–Whitney U test compared continuous variables for normal and nonnormal data, respectively. Overall survival (OS) and progression-free survival (PFS) were calculated using the Kaplan–Meier method for ExR, PoR, and InR for each histopathology. OS was the time of CRS/HIPEC to the date of death from any cause. PFS was the time of CRS/HIPEC to disease recurrence or death from disease, whichever occurred first. All analyses were conducted with STATA version 12.0 and statistically significant if p ≤ 0.05.
Results
Of 368 patients with PD from AC, 250 had mucinous adenocarcinoma (116 LGMCP, 83 HGMCP, and 51 HGMCP-S) with median follow-up of 54 months (range 0–238). Recurrence was diagnosed in 19%, 46%, and 71% LGMCP, HGMCP, and HGMCP-S, respectively.
ExR and PoR Group Selection
For LGMCP, 94 (81%) patients did not recur with a median follow-up of 49 months. Of these 94 patients, 48 had follow-up > 49 months, comprising the ExR group. Recurrence occurred in 22 (19%) patients with a median follow-up of 59 months. Of these 22 patients, 11 recurred before 59 months, comprising the PoR group (Fig. 2).
Scatterplot of exceptional and poor responders by histopathologic subtype. Y-axis displays the follow-up in months. AWD alive with disease, DOC dead of other cause, DOD dead of disease, ExR exceptional responders, HGMCP high-grade mucinous carcinoma peritonei, HGMCP-S high-grade mucinous carcinoma peritonei with signet ring cells, LGMCP low-grade mucinous carcinoma peritonei, LTFU lost to follow-up, Med FU median follow-up, NED no evidence of disease, PoR poor responders
For HGMCP, 45 (54%) patients did not recur with a median follow-up of 60 months. Of these 45 patients, 20 had follow-up > 60 months, comprising the ExR group. Recurrence occurred in 38 (46%) patients with a median follow-up of 40 months. Of these 38 patients, 20 recurred before 40 months, comprising the PoR group (Fig. 2).
For HGMCP-S, 15 (29%) patients did not recur with a median follow-up of 26 months. Of these 15 patients, 7 had follow-up > 26 months, comprising the ExR group. Recurrence occurred in 36 (71%) patients with a median follow-up of 26 months. Of these 36 patients, 20 recurred before 26 months, comprising the PoR group (Fig. 2).
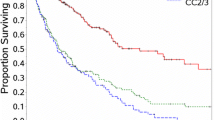
Survival Curves of the Groups Selected
Survival curves compared ExR, PoR, and InR in each histopathology. Comparing the overall population survival curve to that of each subtype shows how patient outcomes are greatly impacted by histopathology. However, within each subtype we aimed to select the outlier patients whose outcomes differ from the average. Survival curves with ExR and PoR show the extreme outcomes of these groups. Moreover, the similarity of the InR (neither ExR nor PoR) curve to the subtype cohort confirms that we successfully selected these outlier patients (Fig. 3).
Survival curves demonstrating the extreme outcomes of exceptional and poor responders by histopathologic subtype. ExR exceptional responders, HGMCP high-grade mucinous carcinoma peritonei, HGMCP-S high-grade mucinous carcinoma peritonei with signet ring cells, InR intermediate responders, LGMCP low-grade mucinous carcinoma peritonei, PoR poor responders
LGMCP: ExR and PoR
In LGMCP, ExR had a median CEA of 2 ng/mL (vs. 41 ng/mL in PoR, p = 0.001) and median CA-125 of 19 U/mL (vs. 84 U/mL in PoR, p = 0.005). Elevated CEA occurred in 26% ExR (vs. 70% PoR, p = 0.022) and elevated CA-125 occurred in 19% ExR (vs. 80% PoR, p = 0.001). Only 36% ExR (vs. 90% PoR) had any TM elevated (p = 0.003). Median PCI for ExR was 26 and 36 for PoR (p = 0.004). Median length of surgery and hospital stay for ExR was 8.6 h (vs. 12 h in PoR, p = 0.021) and 9 days (vs. 14 days in PoR, p = 0.023), respectively (Table 1). Overall, preoperative TM, disease burden, length of surgery, and length of stay were significantly different between ExR and PoR in LGMCP.
HGMCP: ExR and PoR
In HGMCP, mean age at surgery of ExR was 49 ± 10 years (vs. 56 ± 9 years for PoR; p = 0.029). ExR had lower TM levels compared to PoR (CA-125: 12 U/mL vs. 19 U/mL, p = 0.031; CA 19-9: 8 U/mL vs. 27 U/mL, p = 0.007, respectively). ExR were less likely to have elevated TM (CEA: 17% vs. 53%, p = 0.038; CA-125: 6% vs. 37%, p = 0.044; CA 19-9: 0% vs. 42%, p = 0.005). Elevated TM occurred in 22% of ExR (vs. 74% of PoR; p = 0.003; Table 1).
ExR had median PCI of 13 (vs. 34 in PoR, p < 0.001), 32% PCI ≥ 20 (vs. 80% PoR, p = 0.004), and median length of surgery of 8 h (vs. 11.6 h in PoR, p < 0.001) and median length of stay of 9 days (vs. 12 days in PoR, p = 0.014). CC-0 (vs. CC-1) cytoreductions occurred in 84% ExR (vs. 50% PoR, p = 0.041). Positive LN occurred in 16% of ExR (vs. 60% PoR, p = 0.008; Table 1). Overall, age at surgery, preoperative TM, disease burden, degree of complete cytoreduction, LN status, length of surgery, and length of stay were significantly different between ExR and PoR in HGMCP.
HGMCP-S: ExR and PoR
In HGMCP-S, median PCI was 3 for ExR and 30 for PoR (p = 0.001). No ExR versus 80% of PoR had PCI ≥ 20 (p < 0.001). ExR had median length of surgery of 6.4 h (vs. 11 h in PoR, p < 0.001) and median hospital stay of 7 days (vs. 10 days in PoR, p = 0.003). All ExR had CC-0 versus only 40% of PoR (p = 0.008; Table 1). Overall, disease burden, degree of complete cytoreduction (CC-0 vs. CC-1), length of surgery, and length of stay were significantly different between ExR and PoR in HGMCP-S.
Discussion
Identifying patients with peritoneal dissemination (PD) from appendiceal cancer (AC) who will benefit from CRS/HIPEC or require additional treatments is essential in the management of this stage IV disease. Outcomes after CRS/HIPEC vary according to histopathologic subtype and quality of cytoreduction; however, within each histopathologic subtype, even when complete cytoreduction is achieved, there are still patients who respond exceptionally well or very poorly after this treatment. Stratifying patients by recurrence status and follow-up time allowed us retrospectively to select exceptional and poor responders treated with complete CRS/HIPEC within each subtype and compare their perioperative characteristics to better understand their clinical outcomes and obtain potential candidates for further molecular analysis.
The scatterplot patterns show the dramatic effect of histopathologic subtype on patient outcomes (Fig. 2). Moving from LGMCP to HGMCP to HGMCP-S, in the nonrecurrent groups the frequency of patients alive without disease (blue dots) decreases, whereas in the recurrent group the frequency of those dead of disease (red dots) increases. In high-grade malignancies, there are fewer ExR and PoR represent the majority.
Factors related to response vary across histopathologic subtype with the exception of PCI, length of surgery, and length of stay. Median PCI was higher in PoR versus ExR regardless of histopathologic subtype. The relevance of disease burden on outcomes has been reported by many authors.8,14,15,16,17 Our selection method also confirmed this. Additionally, the consistently significant differences observed in length of surgery and length of hospital stay could be explained by the difference in PCI, because greater disease burden requires more extensive surgery.18
It is worth noting that high disease burden (PCI ≥ 20) was significant in HGMCP and HGMCP-S but not in LGMCP. Seventy-three percent of LGMCP ExR had PCI ≥ 20 compared with 91% LGMCP PoR (p = 0.426). Therefore, PCI ≥ 20 in LGMCP may not be the right value to determine “high disease burden,” related to poor response, or an important selection criteria when a complete cytoreduction is feasible. However, PCI still contributes to LGMCP outcomes, because the median PCI was significantly different between ExR and PoR (26 vs. 36, p = 0.004).
Elevated tumor markers (TM) in ExR and PoR were significant in LGMCP and HGMCP. LGMCP PoR had higher CEA and CA-125 levels, whereas HGMCP PoR had higher CEA, CA-125, and CA 19-9 levels. No significant difference in TM levels between ExR and PoR in HGMCP-S was found, although the small number of ExR limits this finding. Another trend was the difference in median TM levels between ExR and PoR across histopathologies. As tumor grade increases (LGMCP to HGMCP to HGMCP-S), the difference between ExR and PoR median CEA and CA-125 decreased (CEA: 49.8 to 3.7 to 0.7 ng/mL; CA-125: 64.7 to 6.7 to 2 U/mL, respectively) and median CA 19-9 increased (0.4 to 19 to 15.6 U/mL, respectively). Thus, it is likely that the conflicting reported significance of TM on patient outcomes may be related to histopathologic subtype.19,20,21 TM should be analyzed in the context of histology.
Most consider CC-0 and CC-1 cytoreductions to be “complete” and associated with the best outcomes.16,22,23,24 In our study, this seems to be the case for low-grade tumors only. In HGMCP and HGMCP-S, more ExR had CC-0 cytoreductions than PoR, emphasizing the necessity of an aggressive surgery with no residual disease for high-grade tumors. A CC-0 cytoreduction is imperative to give patients the best chance at being an ExR in high-grade tumors with or without signet ring cells.
Lymph node status was significant in HGMCP, further validating our selection method. HGMCP PoR were more likely to have positive lymph nodes than HGMCP ExR (60% vs. 15%, p = 0.003). Although lymph node status was not significant for HGMCP-S ExR versus PoR (43% vs. 80%, p = 0.145), it may be due to the few number of ExR in this very aggressive subtype. The negative impact of positive lymph nodes on outcomes has been described in multiple studies and our selection method for ExR and PoR confirmed this in high-grade tumors.8,24,25,26,27
This method identified ExR and PoR after complete CRS/HIPEC within each histopathologic subtype. The clinical profile of LGMCP ExR was no TM elevated, normal CEA and CA-125, and PCI around 26. HGMCP ExR had no TM elevated, normal CEA, CA-125, and CA 19-9, low disease burden with PCI around 13, CC-0, and negative LN. In HGMCP-S, those with very low disease burden with PCI around 3 and CC-0 responded exceptionally well. These results are concordant with previous reported predictor factors in PD from AC and highlight the relevance of molecular characteristics in ExR and PoR. It is known that appendiceal cancers have molecular profiles distinct from colorectal cancer and between histopathologic subtypes.3 GNAS and TP53 mutations have been identified as prognostic biomarkers related to low- and high-grade tumors, respectively, whereas wild-type KRAS has been associated with better survival in patients treated with irinotecan.28,29 Therefore, molecular profiling of ExR and PoR may further elucidate clinical differences and aid in the development of novel targeted therapies.
Successfully defining ExR and PoR allows researchers to explore new ways to understand clinical outcomes and further investigate the molecular aspects of this rare disease. Currently, there is much interest in investigating these outstanding responders to glean insight into how to improve the average response. In 2014, the National Cancer Institute started the Exceptional Responders Initiative (ERI) to understand the molecular foundations for exceptional chemotherapy response. ERI defined exceptional responders as those who had a unique response to treatments not effective for most and plan to test their tissue for certain molecular features that could predict therapy response.30 Likewise, the Network of Enigmatic Exceptional Responders based at Harvard Medical School is a similar project that strives to identify genetic, health, and environmental factors that might explain the events that lead to exceptional outcomes in exceedingly rare patients.31 Correlating molecular features to clinical outcomes is invaluable in understanding and unlocking the best way to treat a disease.
In appendiceal neoplasms, Ang et al. performed genomic profiling in 703 cases, but only 76 cases were able to be correlated with clinical data.28 Borazanci et al. also profiled 588 specimens with primary AC; however, no clinical data were available for this large cohort.32 Both studies have yielded a lot of variable information that will take time to filter. However, the NCI investigators believe that exome-sequencing and deep targeted sequencing from only 100 outlier cases will yield promising discoveries. By utilizing this method to define ExR and PoR, researchers increase the chances of finding clinically meaningful results in a smaller population, which is essential in a rare cancer where not much clinical data and patients exist and can help to narrow the abundance of genomic data. We have successfully identified “outlier” patients with a rare disease from a cohort treated by the same surgical team with 19 years of clinical follow-up and matched tumor samples. This new approach allowed us to identify and characterize a specific population that not only have a particular clinical profile but may also harbor relevant genetic alterations that could explain their particular outcomes and should be explored.
We acknowledge some limitations in this study, including its retrospective design, data collected from a single institution, and the small sample size. Once we divided the large group of patients by histopathologic subtype and only selected the exceptional and poor responders, excluding patients with recent CRS/HIPEC or who recurred after a long time, we ended up with small number of patients, especially in HGMCP-S. This makes it difficult to detect small differences between groups or draw any generalizations about independence of the significant variables found within each histopathologic subtype. Finally, this is a new approach to define “outlier” patients that has not been described; however, it is grounded in clinical decision (those with the longest disease-free survival vs. quick recurrence) with findings that correlate with previously described predictive and prognostic factors.8,22,33,34,35
Conclusions
Stratifying patients by recurrence status and follow-up time is one method to identify patients retrospectively who respond exceptionally well or very poorly to treatment. This method yielded a select group in which genetic alterations should be explored to further elucidate the observed clinical outcomes and aid in the development of novel targeted therapies. Perioperative characteristics related to exceptional and poor outcomes in peritoneal dissemination from appendiceal cancer after CRS/HIPEC vary across histopathologic subtypes with the exception of disease burden, which impacts all subtypes. Genetic alteration studies in this cohort will follow.
References
Chua TC, Pelz JO, Kerscher A, Morris DL, Esquivel J. Critical analysis of 33 patients with peritoneal carcinomatosis secondary to colorectal and appendiceal signet ring cell carcinoma. Ann Surg Oncol. 2009;16(10):2765–70.
Sugarbaker PH, Jablonski KA. Prognostic features of 51 colorectal and 130 appendiceal cancer patients with peritoneal carcinomatosis treated by cytoreductive surgery and intraperitoneal chemotherapy. Ann Surg. 1995;221(2):124–32.
Alakus H, Babicky ML, Ghosh P, et al. Genome-wide mutational landscape of mucinous carcinomatosis peritonei of appendiceal origin. Genome Med. 2014;6(5):43.
Carr NJ, Bibeau F, Bradley RF, et al. The histopathological classification, diagnosis and differential diagnosis of mucinous appendiceal neoplasms, appendiceal adenocarcinomas and pseudomyxoma peritonei. Histopathology. 2017;71(6):847–58.
Misdraji J. Mucinous epithelial neoplasms of the appendix and pseudomyxoma peritonei. Mod Pathol. 2015;28(Suppl 1):S67–79.
Carr NJ, Cecil TD, Mohamed F, et al. A consensus for classification and pathologic reporting of pseudomyxoma peritonei and associated appendiceal neoplasia: the results of the Peritoneal Surface Oncology Group International (PSOGI) Modified Delphi Process. Am J Surg Pathol. 2016;40(1):14–26.
Sugarbaker PH. New standard of care for appendiceal epithelial neoplasms and pseudomyxoma peritonei syndrome? Lancet Oncol. 2006;7(1):69–76.
Jimenez W, Sardi A, Nieroda C, et al. Predictive and prognostic survival factors in peritoneal carcinomatosis from appendiceal cancer after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 2014;21(13):4218–25.
Reghunathan M, Kelly KJ, Valasek MA, Lowy AM, Baumgartner JM. Histologic predictors of recurrence in mucinous appendiceal tumors with peritoneal dissemination after HIPEC. Ann Surg Oncol. 2018;25(3):702–8.
Jacquet P, Sugarbaker PH. Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treat Res. 1996;82:359–74.
Shankar S, Ledakis P, El Halabi H, Gushchin V, Sardi A. Neoplasms of the appendix: current treatment guidelines. Hematol Oncol Clin N Am. 2012;26(6):1261–90.
Sugarbaker P. Technical handbook for the integration of cytoreductive surgery and perioperative intraperitoneal chemotherapy into the surgical management of gastrointestinal and gynecologic malignancy, 4th edn. Foundation for Applied Research in Gastrointestinal Oncology; 2005.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Aziz O, Jaradat I, Chakrabarty B, et al. Predicting survival after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for appendix adenocarcinoma. Dis Colon Rectum. 2018;61(7):795–802.
Sugarbaker PH. Epithelial appendiceal neoplasms. Cancer J. 2009;15(3):225–35.
Van Sweringen HL, Hanseman DJ, Ahmad SA, Edwards MJ, Sussman JJ. Predictors of survival in patients with high-grade peritoneal metastases undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Surgery. 2012;152(4):617–24 (discussion 624–5).
Esquivel J, Sugarbaker PH. Second-look surgery in patients with peritoneal dissemination from appendiceal malignancy: analysis of prognostic factors in 98 patients. Ann Surg. 2001;234(2):198–205.
Arjona-Sanchez A, Esquivel J, Glehen O, et al. A minimally invasive approach for peritonectomy procedures and hyperthermic intraperitoneal chemotherapy (HIPEC) in limited peritoneal carcinomatosis: the American Society of Peritoneal Surface Malignancies (ASPSM) multi-institution analysis. Surg Endosc. 2019;33(3):854–60.
Wagner PL, Austin F, Sathaiah M, et al. Significance of serum tumor marker levels in peritoneal carcinomatosis of appendiceal origin. Ann Surg Oncol. 2013;20(2):506–14.
van Ruth S, Hart AA, Bonfrer JM, Verwaal VJ, Zoetmulder FA Prognostic value of baseline and serial carcinoembryonic antigen and carbohydrate antigen measurements in patients with pseudomyxoma peritonei treated with cytoreduction and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 2002;9(10):961–67.
Taflampas P, Dayal S, Chandrakumaran K, Mohamed F, Cecil TD, Moran BJ. Pre-operative tumour marker status predicts recurrence and survival after complete cytoreduction and hyperthermic intraperitoneal chemotherapy for appendiceal Pseudomyxoma peritonei: analysis of 519 patients. Eur J Surg Oncol. 2014;40(5):515–20.
Chua TC, Moran BJ, Sugarbaker PH, et al. Early- and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Clin Oncol. 2012;30(20):2449–56.
Omohwo C, Nieroda CA, Studeman KD, et al. Complete cytoreduction offers longterm survival in patients with peritoneal carcinomatosis from appendiceal tumors of unfavorable histology. J Am Coll Surg. 2009;209(3):308–12.
Votanopoulos KI, Russell G, Randle RW, Shen P, Stewart JH, Levine EA. Peritoneal surface disease (PSD) from appendiceal cancer treated with cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC): overview of 481 cases. Ann Surg Oncol. 2015;22(4):1274–9.
Glehen O, Mohamed F, Sugarbaker PH. Incomplete cytoreduction in 174 patients with peritoneal carcinomatosis from appendiceal malignancy. Ann Surg. 2004;240(2):278–85.
Halabi HE, Gushchin V, Francis J, et al. Prognostic significance of lymph node metastases in patients with high-grade appendiceal cancer. Ann Surg Oncol. 2012;19(1):122–5.
Baumgartner JM, Tobin L, Heavey SF, Kelly KJ, Roeland EJ, Lowy AM. Predictors of progression in high-grade appendiceal or colorectal peritoneal carcinomatosis after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 2015;22(5):1716–21.
Ang CS-P, Shen JP, Hardy-Abeloos CJ, et al. Genomic landscape of appendiceal neoplasms. JCO Precis Oncol. 2018(2):1–18.
Hara K, Saito T, Hayashi T, et al. A mutation spectrum that includes GNAS, KRAS and TP53 may be shared by mucinous neoplasms of the appendix. Pathol Res Pract. 2015;211(9):657–64.
NCI. Molecular profiling in tissue samples from patients with cancer who are exceptional responders to treatment. 2014. https://ClinicalTrials.gov/show/NCT02243592. Accessed 25 Jan 2019.
The ASCO Post. Unraveling the Mystery of What Gives Exceptional Responders Their Superpower. http://www.ascopost.com/issues/august-25-2018/unraveling-the-mystery-of-what-gives-exceptional-responders-their-superpower/. Accessed 29 Jan 2019 (2018).
Borazanci E, Millis SZ, Kimbrough J, Doll N, Von Hoff D, Ramanathan RK. Potential actionable targets in appendiceal cancer detected by immunohistochemistry, fluorescent in situ hybridization, and mutational analysis. J Gastrointest Oncol. 2017;8(1):164–72.
Ihemelandu C, Sugarbaker PH. Clinicopathologic and prognostic features in patients with peritoneal metastasis from mucinous adenocarcinoma, adenocarcinoma with signet ring cells, and adenocarcinoid of the appendix treated with cytoreductive surgery and perioperative intraperitoneal chemotherapy. Ann Surg Oncol. 2016;23(5):1474–80.
Smeenk RM, Verwaal VJ, Antonini N, Zoetmulder FA. Survival analysis of pseudomyxoma peritonei patients treated by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg. 2007;245(1):104–9.
Baratti D, Kusamura S, Nonaka D, et al. Pseudomyxoma peritonei: clinical pathological and biological prognostic factors in patients treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC). Ann Surg Oncol. 2008;15(2):526–34.
Acknowledgment
The authors thank Roy Hatch for his help with the literature review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare that there is no conflict of interest regarding the publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Munoz-Zuluaga, C., King, M.C., Sardi, A. et al. Selection and Characteristics of Patients with Peritoneal Dissemination from Appendiceal Cancer with Exceptional/Poor Survival After CRS/HIPEC. Ann Surg Oncol 26, 2268–2275 (2019). https://doi.org/10.1245/s10434-019-07374-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07374-z