Abstract
Background
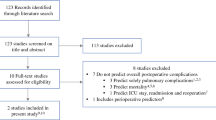
Few risk models have been provided to predict long-term prognosis after esophagectomy. This study investigated the reliability of a risk calculator as well as classification and regression trees analysis for predicting long-term prognosis after esophagectomy for esophageal cancer.
Methods
The study enrolled 438 patients who underwent esophagectomy at Keio University Hospital, Tokyo, Japan, between July 2000 and June 2016. Patients who underwent R0 or R1 resection or esophagectomy with combined resection of other organs were included. The authors investigated the usefulness of a risk model for 30-day mortality and operative mortality described in their previous report for predicting long-term prognosis after esophagectomy.
Results
The 438 patients (377 men and 61 women) in this study had a 5-year overall survival (OS) rate of 62.8% and a disease-free survival rate of 54.3%. The OS was higher for the patients with 30-day mortality risk model values lower than 0.675% than for those with values higher than 0.675% (p < 0.001). The cutoff values for prediction were shown to be significant risk factors in the multivariate analysis. The risk calculator was validated by comparing the cutoff values with Harrell’s C-index values of clinical stage. For overall risk, the C-index of operative mortality was 0.697, and the C-index of cStage was 0.671.
Conclusions
The risk calculator was useful for predicting recurrence and death after esophagectomy. Furthermore, because the C-index of the risk model for operative mortality was higher than for clinical tumor-node-metastasis stage, this risk-scoring system may be more useful clinically.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Despite recent development of surgical techniques and perioperative management for esophageal cancer, esophageal cancer continues to have a poor long-term outcome due to its high malignant potential.1 Some predictive factors of long-term prognosis after esophagectomy have been reported,2,3 and we have previously investigated the relationship between postoperative complications and long-term prognosis.4,5
In a previous study,5 we reported that postoperative pneumonia had a negative effect on overall survival (OS) after esophagectomy and suggested that the status of systemic inflammation, such as severe complications, would compromise cell-mediated immunity and induce micrometastasis.6 Furthermore, these complications often delay postoperative therapy. Thus, we suggested that patients who had higher risk factors for operative morbidity would have negative outcomes of recurrence or OS. We hypothesized that it would be possible to predict long-term prognosis by knowing risk factors for short-term outcomes after esophagectomy. We had previously performed risk stratification for esophagectomy using a risk calculator and had determined a risk-scoring system to predict 30-day and operative mortality.1 To enhance reliability, we hypothesized that our previous scoring system could be used to predict long-term outcomes if the backgrounds of the patients in the previous study were the same as those of patients in a new study.
In this study, we investigated the reliability of a risk calculator for predicting long-term recurrence and survival and determined cutoff values. To the best of our knowledge, this is the first report of relationships among calculator risk values and long-term prognosis in addition to risk cutoff values for recurrence and death.
Methods
Patients
This study enrolled 438 patients who had undergone esophagectomy with open thoracotomy or video-assisted thoracic surgery for thoracic esophageal cancer as the primary treatment at Keio University Hospital, Tokyo, Japan, between July 2000 and June 2016. Patients who underwent R0 or R1 resection or esophagectomy with combined resection of other organs were included.
Before treatment, the patients were examined by upper gastrointestinal endoscopy, thoracic and abdominal computed tomography, laboratory tests, and esophagography. The clinical stages of cancer were determined according to the Union Against Cancer, 7th edition.7 We excluded a patient who had cervical esophageal cancer and esophago-gastric junctional cancer.
We retrospectively evaluated the patients’ clinical information, pathologic findings, and prognosis obtained from hospital records. This study was conducted with the approval of the ethics committee of Keio University School of Medicine.
Surgical Procedures
At our hospital, transthoracic subtotal esophagectomy and resection of regional two- or three-field lymph nodes were performed.8 Thoracic procedures were performed through a right thoracic incision or by video-assisted thoracic surgery (VATS) with the patient in the left decubitus position in the years 2000–2008 or in a hybrid position combining the left decubitus position and the prone position since 2009.5,9
We routinely dissected mediastinal lymph nodes with bilateral recurrent nerve lymph nodes and abdominal lymph nodes, including pericardial lymph nodes and lymph nodes along the lesser curvature and left gastric artery.5,8 Since 2009, we also have resected the thoracic duct to achieve further radical lymph node dissection.8 We mainly used the stomach as an anastomotic organ with a cervical esophagus and performed reconstruction through the posterior mediastinal route.8,9,10 We used the terminal ileum and right colon as an anastomotic organ and followed an antesternal, retrosternal, or intrathoracic reconstructed route when gastric tubes could not be used because of synchronous double cancer of the stomach or a history of gastrectomy.8
Morbidity and Mortality
We used the Clavien–Dindo classification for complications and identified complication cases as those having a Clavien–Dindo classification greater than grade 2.11 The definition of grade 2 is the requirement of pharmacologic treatment without drugs other than those allowed for grade 1 complications. The definition of grade 3 is the requirement of surgical, endoscopic, or radiologic intervention. The definition of grade 4 is the presence of life-threatening complications requiring intensive care unit management. Grade 5 is defined as the death of a patient.
We also divided complications into two groups. The patients in group 1 had medical complications that were unrelated to the surgical procedure directly but were systemic responses against surgery such as pneumonia, arrhythmia, sepsis, or enteritis, and the patients in group 2 had surgical complications related to the surgical procedure such as anastomotic leakage, surgical-site infections (SSIs), recurrent laryngeal nerve palsy, abdominal hemorrhage, chylothorax, and necrosis of the gastric tube. Residual tumors were classified as R0 (no residual tumor), R1 (microscopic), and R2 (macroscopic residual tumor).
We investigated the physical status and laboratory test results every 3 months. We also examined upper gastrointestinal endoscopy and thoracic abdominal computed tomography (CT) scans every 6 or 12 months for at least 5 years after esophagectomy. The disease-free survival (DFS) and OS also were calculated from the date of surgery. Moreover, we examined 30-day mortality and operative mortality that occurred during hospitalization within 90 days or after discharge within 30 days after surgery.
Risk Calculator for Esophagectomy
We previously reported risk scoring systems for mortality risk models after esophagectomy using a nationwide database that applied the following logistic regression equation1:
where β i is the coefficient of the variable X i in the logistic regression equation. In this calculation, X i is 1 if a categorical factor is present and 0 if it is absent. For age category, X i is 1 for age 59 years or younger, 2 for age 60–64 years, 3 for age 65–69 years, 4 for age 70–74 years, and 5 for age 75 or older.1 We retrospectively evaluated the patient’s preoperative characteristics for calculation of the risk for 30-day mortality and operative mortality (Table S1).1
Statistical Analysis
Statistical analyses were performed by using Stata/SE 12.1 for Mac (StataCorp, College Station, TX, USA). Categorical variables were analyzed by using the Chi square test for univariate analysis, and continuous variables were analyzed by using the Mann–Whitney U test. A p value lower than 0.05 was considered to indicate statistical significance.
We investigated associations between the risk calculator’s values and prognosis using the Kaplan–Meier method and log-rank tests. Moreover, variables with p values lower than 0.05 in the univariate analysis were subsequently entered into a Cox regression model for multivariate analysis.
Classification and regression trees (CART) analysis are machine-learning methods for constructing a prediction model and simulating the clinical decisions process. It uses a generalization of the binomial variance called the Gini index and has some advantages. It can be fast in making predictions and can show cutoff values easily recognized visually.12,13,14 We used CART analysis to determine the best cutoff values of the risk model for 30-day mortality and operative mortality. These cutoff values were used to predict prognosis by applying the statistical software R, version 3.1.2 (R Foundation Statistical Computing, Vienna, Austria). The R packages “ctree” and “party” were used.12 To validate model performance, the C-index, a measure of model discrimination and area under the receiver operating characteristics (ROC) curve, was evaluated.
Results
Background Characteristics
The study investigated 377 men and 61 women (Table 1). The mean risk values were 1.22 ± 4.25% for 30-day mortality and 3.03 ± 4.37% for operative mortality (Table 1). Postoperatively, 270 patients (61.6%) had complications greater than Clavien–Dindo grade 2, 157 patients (35.8%) had medical complications, 183 patients (41.8%) had surgical complications, and 168 patients (38.4%) had no complications.
Validation of the Risk Model for Mortality
One patient (0.23%) died within 30 days, and four patients (0.91%) died during their hospital stay. The cause of 30-day mortality was acute respiratory distress syndrome (ARDS) within 7 days after esophagectomy. The operative mortality cases comprised one patient with lung metastasis, one patient with multiple brain metastasis, and other patients with ARDS. Although the mean risk model values for 30-day mortality did not differ significantly between the patients who did and those who did not die within 30 days (1.01% vs 1.22 ± 4.25%; p = 0.370), the mean risk model value for operative mortality among the patients who died during the operation was significantly higher than among the patients who did not die during the operation (9.37 ± 8.34% vs 2.97 ± 4.29%; p = 0.017).
OS and DFS
For all the patients, the 5-year OS rate was 62.8% and the DFS rate was 54.3%. We also investigated OS after dividing the patients into two groups by the cutoff values calculated by CART. Compared with the group of patients who had risk model 30-day mortality values higher than 0.675%, the group of patients with values of 0.675% or lower had a longer OS (p < 0.001). The risk model of operative mortality showed an OS rate significantly lower for the group of patients who had risk model for operative mortality values higher than 4.931% than for the group with values 4.931% or lower (p < 0.001) (Fig. 1a). For predicting DFS rates, the cutoff values determined by using CART were 0.594% for the risk model for 30-day mortality and 2.467% for the risk model for operative mortality (p < 0.001 for both) (Fig. 1b). In the multivariate analysis using Cox regression that included these factors, only the factors of clinical stages 3 and 4 and the risk model for mortality value were identified as predictors of death (risk model for 30-day mortality value > 0.675%; p < 0.001; hazard ratio [HR] 2.46; 95% confidence interval [CI] 1.75–3.46; and risk model for operative mortality > 4.931%; p < 0.001; HR 4.23; 95% CI 2.94–6.08) (Table 2A).
Clinical stages 3 and 4 and the risk model for mortality value also were identified as predictors of recurrence. (Table 2B). Moreover, the OS was significantly higher in the group with the high risk model for mortality values for all pathologic stages except for the group with risk model for 30-day mortality values of 0.675% or lower with a diagnosis of pathologic stage 4 disease. In contrast to the patients who underwent no neoadjuvant or neoadjuvant chemotherapy, the risk model values for the patients who underwent neoadjuvant chemoradiotherapy did not differ significantly except for the DFS of the patients with the risk model for operative mortality cutoff values higher than 2.467%.
Validation of Risk Model Performance for OS and DFS
To evaluate model performance, we validated the reliability of the risk calculator by comparing the risk model values with the Harrell’s C-index values of the clinical stage that was a significant risk factor for death and recurrence. For overall risk, the C-index of the risk model for operative mortality was the highest (C-index, 0.697), whereas the C-indexes were 0.662 for 30-day mortality and 0.671 for cStage. For the risk of recurrence, the C-indexes were 0.625 for 30-day mortality, 0.667 for operative mortality, and 0.684 for cStage.
Discussion
This study demonstrated the associations among our risk calculator values and the OS and DFS rates of patients who had undergone esophagectomy for esophageal cancer. We used CART analysis to determine the cutoff values for predicting OS and DFS. Furthermore, the C-index of the risk model for operative mortality was higher than for clinical TNM stage, suggesting that this risk scoring system would be more useful clinically.
In the current study, significantly lower DFS and OS were observed for the patients who had medical complications. These findings potentially could be explained by the effects of inflammatory mediators and growth factors. Our previous two studies showed that changes in cytokines, such as interleukin 6 (IL-6) or IL-8, caused by postoperative complications or surgical stress, adversely affected short- and long-term outcomes after esophagectomy.15,16
In other studies, perioperative immunosuppression increased the incidence of metastasis.17,18,19 Moreover, invasive status, such as postoperative complications, can highly regulate specific growth factors such as fibroblast growth factors, epidermal growth factors, platelet-derived growth factor, and vascular endothelial growth factors. Because these growth factors lead to acceleration of tumor growth, this stimulatory pathway has been targeted for curative therapies for cancer.20 Although medical complications strongly correlated with long-term outcomes for these reasons in our study, it was more important preoperatively to identify all factors used in our risk calculator for predicting OS and DFS with respect to clinical aspects because there may be other etiologies of cytokine changes (e.g., micro-aspirated pneumonia), not just surgical complications.
We previously concluded that a risk calculator, especially one using a risk model for operative mortality, was the most reliable predictor of survival because it reflects many causes for increased inflammatory mediators and growth factors.21 Moreover, this calculator also included some factors, such as smoking history, weight loss, low-grade nutrition, platelet count, and thrombocytosis, that findings have shown to be independent predictive factors for long-term survival after esophagectomy,22,23,24 which improved the reliability of our calculator.
To date, only a few studies have investigated risk scoring systems for esophageal cancer. Reeh et al.25 reported that a preoperative esophageal risk score based on cardiovascular, pulmonary and hepato–renal organ systems was found to be an independent predictor of not only short-term outcomes but also of tumor recurrence. This scoring system is a useful predictor because of its simplicity. However, the calculator did not consider the factor of neoadjuvant therapy, as noted in the report.
Currently, neoadjuvant therapy for esophageal cancer is essential treatment. Therefore, patients who have undergone neoadjuvant therapy must be considered, as in our study, for predicting prognosis in esophageal cancer.
In addition, besides our risk calculator, there are no other biomarker or risk scoring systems for predicting recurrence that have shown reliability indicators as good as those in our risk model (HR 2.39; 95% CI 1.70–3.35 in the risk model for operative mortality). Furthermore, our risk model appears to be a better predictor than even clinical stage. The C-index of the risk model for operative mortality was 0.697, which was the highest C-index of any other risk factors. This finding suggests that both the reliability of the risk calculator for long-term outcome and preoperative factors contribute to prediction of prognosis of cancer.
This study had limitations. First, it was a retrospective single-center study limited to a Japanese population and thus may have been subject to selection bias. Second, the results of surgical treatment also can be affected by hospital volume and training status, especially for high-risk operations such as esophagectomy.26 Our results need to be validated in a multicenter prospective study in the future.
References
Takeuchi H, Miyata H, Gotoh M, et al. A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg. 2014;260:259–66.
Kidane B, Sulman J, Xu W, et al. Baseline measure of health-related quality of life (functional assessment of cancer therapy-esophagus) is associated with overall survival in patients with esophageal cancer. J Thorac Cardiovasc Surg. 2016;151:1571–80.
Hamai Y, Hihara J, Emi M, et al. Ability of fluorine-18 fluorodeoxyglucose positron emission tomography to predict outcomes of neoadjuvant chemoradiotherapy followed by surgical treatment for esophageal squamous cell carcinoma. Ann Thorac Surg. 2016;102:1132–39.
Takeuchi H, Saikawa Y, Oyama T, et al. Factors influencing the long-term survival in patients with esophageal cancer who underwent esophagectomy after chemoradiotherapy. World J Surg. 2010;34:277–84.
Booka E, Takeuchi H, Nishi T, et al. The impact of postoperative complications on survivals after esophagectomy for esophageal cancer. Med Baltim. 2015;94:e1369.
Matsuda S, Takeuchi H, Kawakubo H, et al. Cumulative prognostic scores based on plasma fibrinogen and serum albumin levels in esophageal cancer patients treated with transthoracic esophagectomy: comparison with the Glasgow prognostic score. Ann Surg Oncol. 2015;22:302–10.
Sobin L, Gospodarowicz M WC, eds. TNM Classification of Malignant Tumours. 7th ed Wiley-Liss, New York, 2009.
Matsuda S, Takeuchi H, Kawakubo H, et al. Clinical outcome of transthoracic esophagectomy with thoracic duct resection: number of dissected lymph node and distribution of lymph node metastasis around the thoracic duct. Med Baltim. 2016;95:e3839.
Kaburagi T, Takeuchi H, Kawakubo H, et al. Clinical utility of a novel hybrid position combining the left lateral decubitus and prone positions during thoracoscopic esophagectomy. World J Surg. 2014;38:410–18.
Takesue T, Takeuchi H, Ogura M, et al. A prospective randomized trial of enteral nutrition after thoracoscopic esophagectomy for esophageal cancer. Ann Surg Oncol. 2015;22:802–09.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Breiman L, Friedman JH, Stone CJ, et al. Classification and regression trees. 1984;1:368.
Garzotto M, Beer TM, Hudson RG, et al. Improved detection of prostate cancer using classification and regression tree analysis. J Clin Oncol 2005;23:4322–29.
Loh W-Y. Classification and regression trees. Wiley Interdiscip. Rev. 2011;1:14–23.
Okamura A, Takeuchi H, Matsuda S, et al. Factors affecting cytokine change after esophagectomy for esophageal cancer. Ann Surg Oncol. 2015;22:3130–35.
Ogura M, Takeuchi H, Kawakubo H, et al. Clinical significance of CXCL-8/CXCR-2 network in esophageal squamous cell carcinoma. Surgery. 2013;154:512–20.
Shakhar G, Ben-Eliyahu S. Potential prophylactic measures against postoperative immunosuppression: could they reduce recurrence rates in oncological patients? Ann Surg Oncol. 2003;10:972–92.
Hogan BV, Peter MB, Shenoy HG, et al. Surgery-induced immunosuppression. Surgeon. 2011;9:38–43.
Goldfarb Y, Sorski L, Benish M, et al. Improving postoperative immune status and resistance to cancer metastasis. Ann Surg. 2011;253:798–810.
Abramovitch R, Marikovsky M, Meir G, et al. Stimulation of tumour growth by wound-derived growth factors. Br J Cancer. 1999;79:1392–98.
Ferri LE, Law S, Wong KH, et al. The influence of technical complications on postoperative outcome and survival after esophagectomy. Ann Surg Oncol. 2006;13:557–64.
Feng JF, Huang Y, Lu WS CQ. Preoperative platelet count in esophageal squamous cell carcinoma: is it a prognostic factor? Langenbecks Arch Surg. 2013;398:1115.
Shimada H, Oohira G, Okazumi S, et al. Thrombocytosis associated with poor prognosis in patients with esophageal carcinoma. J Am Coll Surg. 2004;198:737–41.
Tsuruo T, Fujita N. Platelet aggregation in the formation of tumor metastasis. Proc Japan Acad Ser B, Phys Biol Scienes. 2008;84:189–98.
Reeh M, Metze J, Uzunoglu FG, et al. The PER (Preoperative Esophagectomy Risk) Score: a simple risk score to predict short-term and long-term outcome in patients with surgically treated esophageal cancer. Medicine Baltimore. 2016;95:1–8.
Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:2128–37.
Acknowledgment
The authors thank Kumiko Motooka, who belongs to the staff at the Department of Surgery in Keio University School of Medicine, for her help in the preparation of this report.
Disclosure
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Takeuchi, M., Takeuchi, H., Kawakubo, H. et al. Perioperative Risk Calculator Predicts Long-Term Oncologic Outcome for Patients with Esophageal Carcinoma. Ann Surg Oncol 25, 837–843 (2018). https://doi.org/10.1245/s10434-017-6311-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-6311-7