Abstract
Background
Young women with breast cancer (BC) have an increased risk of contralateral breast cancer (CBC) compared with older women. This may contribute to the rising rates of bilateral mastectomy (BM), but it is unclear if BM leads to improved outcomes.
Methods
A prospectively maintained database was reviewed. Patient and tumor characteristics, survival, and rate of CBC were compared in women age ≤40 years treated for unilateral Stage 1–3 BC from January 2000 through December 2013.
Results
Patients ranged in age from 20 to 40 (mean 36) years. Of the 446 women, 188 had breast conservation surgery (BCS), 78 had unilateral mastectomy (UM), and 183 had BM. UM, BCS, and BM groups did not differ in mean age, tumor type, hormone receptor status, or Her2 status. Patients in the BCS and BM group had smaller, fewer node-positive (p = 0.02) and lower grade tumors (p < 0.01) compared with the UM group. With a median follow-up of 79 months, Disease-free survival was similar for patients treated with BM, BCS (p = 0.22), or UM (p = 0.75). OS was significantly worse in the patients treated with UM (0.02) but was not different between the BCS and BM groups. CBC incidence was 2% (5/263) in patients who underwent BCS or UM, and 0.4% (1/244) in patients without a germline genetic mutation.
Conclusions
BCS and UM resulted in similar disease-free survival (DFS) as BM in patients age 40 years and younger with BC. BCS and BM had similar OS, whereas UM patients had worse OS. Invasive CBC incidence was less than 0.5% at 10 years in patients without identified germline genetic mutations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Breast cancer is the leading cause of cancer-related death in women aged 20–40 years.1–3 Previous studies indicate that women younger than 40 have tumors with more aggressive biology and a worse prognosis, including a higher rate of locoregional recurrence following breast conserving therapy than patients older than age 50 years.4,5 In breast cancer survivors, the most frequent second primary cancer is a breast cancer in the contralateral breast.6 A review of the Surveillance, Epidemiology and End Results Program (SEER) database in 2010 found that women younger than age 50 years with stage 1–2, estrogen-receptor (ER)-negative tumors have a higher rate of contralateral breast cancer (CBC) than their older peers.5 Younger women also are more likely to have to have BRCA or other mutations, which put them at increased risk of CBC.7 Given this information, it is not surprising that bilateral mastectomy (BM) rates have risen from 3% in 1998 to 33% in 2011 in Californian women younger than age 40 years.8
Large, population-based studies have failed to demonstrate consistently a survival benefit to BM, but the number of young women included in these studies was low and variable.9–11 The rates of local recurrence and CBC have declined dramatically with improvements in adjuvant therapy for all women with breast cancer.7,12 Current recommendations, even in young women, are that BM should be considered only for women at high risk for a second primary breast cancer.13 Surgeons should continue to recommend breast conservation therapy in women younger than 40 years who are not at genetically increased risk of contralateral breast cancers.14 However, in a recent evaluation of the National Cancer Data Base (NCDB), women aged 45 years or younger have decreasing lumpectomy rates, and BM increased from 9.3 to 26.4% in this group between 2003 and 2010.15 The purpose of this study was to determine whether a contemporary cohort of women under age 40 years diagnosed with unilateral operable breast cancer undergoing BM had lower rates of CBC, improved disease-free (DFS), or overall survival (OS) compared with those undergoing unilateral mastectomy (UM) or breast conservation surgery (BCS).
Methods
A prospectively maintained database at a single academic institution was reviewed with approval from the institutional review board. Women age 40 years and younger treated for unilateral Stage 1–3 breast cancer from January 2000 through December 2013 were identified. Patient demographics, tumor characteristics, surgical treatment, and adjuvant therapy, including radiation, endocrine therapy and chemotherapy, CBC, distant recurrence, and survival data were collected. Patient and tumor characteristics were compared among patients who underwent BCS, UM, and BM. Survival, distant recurrence, and rate of CBC were compared among the three groups.
Statistical analysis was performed using SAS technology. Chi Square and Wilcoxon rank-order tests were used to compare categorical variables. Univariable analysis was performed using the Kruskal–Wallis test. A multivariable survival analysis was performed using a stepwise selection method including the following variables: surgery at primary site, hormone receptor status, chemotherapy, hormonal therapy, radiation, grade, histology, age, tumor size, and lymph node status. Kaplan–Meier method was used to estimate time to event distribution. Kaplan–Meier curves were created and analyzed via log-rank.
Results
Patient Characteristics
A total of 446 women age 40 years and younger were treated for unilateral Stage 1–3 breast cancer. Mean patient age was 36 years (range 20–40). Mean follow-up was 88 months, with a median follow-up time of 79 months (range 5–194) for all patients. One hundred twenty-one patients (27%) had >10 year follow-up, 297 patients (67%) patients had >5 years follow-up. One hundred eighty-four women (41%) underwent BCS, 79 (18%) underwent UM, and 183 (41%) patients underwent BM. The number of patients undergoing BCS over time declined, whereas those electing BM has increased (Fig. 1). Overall, 60 (13%) women had identified deleterious genetic germline mutations. Of these, 52 patients had identified BRCA mutations. Two patients had mismatch repair mutations, and a single patient each had a CHEK2 mutation (OMIM 604373) and a BRIP1 mutation (OMIM 605882). Thirty-six of the 183 patients (22%) who underwent BM had BRCA or other identified deleterious mutations, whereas 19 of the 184 patients (7%) who underwent UM or BCS had identified mutations. Five patients without germline mutations (3%) who underwent BM had a history of Hodgkin’s lymphoma treated with mantle field radiation.
Tumor Characteristics
The majority of patients, 370 of 446 (83%), had infiltrating ductal carcinoma. Fourteen patients (3%) had tumors with lobular carcinoma, 21 patients had tumors with other histology (e.g., mucinous or metaplastic), and 41 tumors (9%) had mixed histology. Two-hundred fourteen patients (48%) had ER, PR-positive Her2-negative tumors and 17 patients had ER-positive, PR- and Her2-negative tumors (4%). Four patients (1%) had ER-negative, PR-positive Her2-negative tumors. Seventy-seven patients (17%) had ER-positive, Her2-positive tumors, and 27 patients (6%) patients had ER-negative, PR-negative Her2-positive tumors. One-hundred four patients (23%) had tumors that were triple-negative.
The UM group had more tumors that were >2 cm (49 of 79; 62%) compared with 58 of the 184 patients (32%) treated with BCS and 85 of the 183 patients (44%) treated with BM (p = 0.03). The patients who underwent BCS and BM also had fewer positive nodes (p = 0.02) and more low-grade tumors (p < 0.01) than the patients who underwent UM (Table 1). However, when patients treated with BM were compared to patients who underwent BCS there were no statistically significant differences between the number of lymph node positive patients, the size of tumors, or the hormone receptor status of the tumors.
Despite the evidence of more aggressive tumor biology in patients treated with unilateral mastectomy, more patients (143/184, 78%) treated with BM underwent chemotherapy compared with patients treated with BCS (119/183, 65%) or UM (51/79, 65%). This was most pronounced when lymph node-negative patients in the UM and BM groups were compared. Only 15 of 35 (43%) lymph node negative patients in the UM group had chemotherapy, whereas 79 of 112 (71%) lymph node-negative BM patients elected to undergo chemotherapy (p < 0.01). Seventy-three of the total 446 patients (16%) underwent neoadjuvant chemotherapy. Patients treated with bilateral mastectomy were more likely to have documented hormone therapy use; specifically, only 20 of 52 (38%) ER+ patients who underwent UM had documented hormonal therapy, whereas 82 of 122 (67%) ER+ patients who elected BM had documented hormonal therapy (p < 0.01).
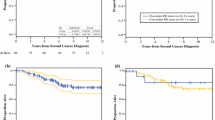
Disease-Free, Overall Survival, and CBC
Five- and 10-year DFS was not statistically significant among operative groups (Fig. 2). Kaplan–Meier estimated 5-year DFS was 87% for the patients treated with BCS (95% confidence interval (CI) 87–88%), 78% for the patients treated with UM (CI 74–82%), and 84% (CI 83–85%) for patients treated with BM (p = 0.42). The 5- and 10- year overall survival in the BCS group was 94% and 85% (CI 94–95% and 84–86%), UM group 79% and 77% (CI 74–81%, SE 0.27), and BM 90% and 83% (CI 89–91, SE 0.17) (p = 0.02). The UM group had worse overall survival compared with BCS and BM groups (Fig. 3). Ten of the 17 UM patients who died had ER-positive tumors (59%). Of the 10 ER+ UM patients who died, only 2 had documented hormone therapy use.
Univariable analysis identified patients treated with UM, nonductal histology, positive lymph node status, and high grade as factors significantly associated with worse DFS. DFS was not significantly associated with ER status, Her2 status, tumor size, receiving hormonal therapy, or age at diagnosis. On multivariable analysis following stepwise selection regional nodal positivity (hazard ratio [HR] 1.1 (SE 0.01) p < 0.01) and high grade (p = 0.05) were correlated with decreased DFS. When overall survival was evaluated by multivariable analysis, lymph node status was the only variable associated with decreased OS (HR 1.1, SE 0.02, p = 0.01). Tumor histologic subtype was not associated with worse overall survival. Surgical approach was not associated with DFS or OS on multivariable analysis.
Overall CBC incidence was only 2%. There were 5 CBC in the 263 patients treated with UM and BCS. Two of these patients developed subsequent ductal carcinoma in situ (DCIS), and three patients developed invasive breast cancer in the contralateral breast during the follow-up period. Two of the three patients with invasive CBC had identified genetic mutations (BRCA 1 and MUTYH). These two patients represent 11% of the 19 patients who had genetic mutations and underwent UM or BCS. Only 1 patient (0.4%) of the 244 patients without genetic mutations who underwent UM or BCS developed a contralateral invasive breast cancer with a median follow-up of 86 months.
Discussion
There is conflicting evidence about the contemporary surgical decision-making and outcomes of young women with breast cancer in a rapidly changing social, diagnostic, and treatment environment. An improved understanding of tumor biology, availability of targeted therapies, and changes in radiation delivery have likely impacted recurrence and survival rates in young women. This study indicates that in women age 40 years and younger with a mean follow-up of more than 6.5 years, BCS resulted in similar DFS and OS for patients as BM.
Women undergoing UM had significantly larger tumors, with more lymph node metastases than patients treated with BCS or BM. This may account for their worse overall survival seen in our study. These observations are similar to those identified in the recently published update of the Prospective Observational Study of Breast Cancer Treatment Outcomes for UK Women Aged 18–40 Years at Diagnosis (POSH). This study examined the outcomes of young women in the United Kingdom with breast cancer over time, stratified by stage and hormone receptor status.16 The majority of events experienced in young women were attributed to distant metastatic disease or death from breast cancer. They also found a higher event rate and lower distant disease-free interval in patients who underwent mastectomy. As in our cohort, mastectomy patients had larger, more frequently node-positive tumors. Patients with node-positive tumors were at highest risk for early local recurrence, distant metastasis, and decreased OS. In addition to suggesting that patients and surgeons are choosing UM in the young patients with more aggressive tumors or advanced disease, it corroborates our finding that mastectomy confers no survival advantage for young women compared with treatment with BCS. While patients who chose UM had more aggressive tumors, node-negative patients who underwent UM were less likely to undergo chemotherapy than those in the BM group. Additionally, patients with tumors that were ER-positive who elected UM were less likely to have documented hormone therapy. These treatment factors might contribute to the worse overall survival in the UM group.
Five- and 10-year DFS were not impacted by operative approach. When comparing patients treated with BM to patients treated with BCS, patients undergoing BM had similar tumor subtype, tumor size, and lymph node positivity. On multivariable analysis, decreased DFS was correlated with higher tumor grade and positive lymph nodes. This is in line with recent studies, including Plichta who compared outcomes in 584 women younger than age 40 years treated with lumpectomy and mastectomy and found no significant difference in DFS, OS, or local recurrence.17 Also, Aalders et al. from the Netherlands, points to tumor biology as a driver of disease-free survival, particularly in young women.18 This study’s results are similar to the results of a recent review of the SEER database, which demonstrated that 10-year survival is equivalent between patients treated with BCS and bilateral mastectomy.19 Contrary to early historical data, BM does not appear to result in a survival advantage, even for young women. As seen in older women, survival in young breast cancer patients is dictated by the tumor biology of their index tumor, influenced by adjuvant therapy, and not improved by contralateral surgery. In the modern era, the rate of contralateral breast cancer events in patients who have undergone unilateral surgery is low. Breast cancer survivors are more aggressively screened in contemporary practice, which may contribute to improved survival in the advent of a second breast cancer. Additionally, many patients with ER-positive disease take Tamoxifen, which also lowers the risk of CBC.
The contralateral breast cancer rate (including both DCIS and invasive cancer) was only 2% in patients who underwent UM or BCS in this cohort. Only three patients developed a contralateral invasive breast cancer in follow-up, and of these, two patients had an identified deleterious germline genetic mutation. The risk of contralateral invasive breast cancer in patients without identified mutations who underwent unilateral surgery was <0.5% with a median follow-up of 79 months. This is consistent with other contemporary studies, which indicate that CBC is a rare event in the modern era.6,7,13 An evaluation of the SEER database from 1975 to 2006 by Nichols et al. suggests that the risk to all breast cancer survivors of CBC has fallen over time.12 The incidence of contralateral cancer in all patients after 1985 was 0.26% per year. In the youngest women evaluated in their cohort (age <30), the incidence was estimated at 0.8 per year, which decreased to 0.25% per year by age 40 years. They also noted that the rate of CBC has decreased beyond the year 2000, particularly in patients with ER positive tumors during the first 5 years following diagnosis, likely due to improvements in systemic therapy. Few studies incorporate genetic mutation status in their overall analysis of CBC incidence in young women. Our patient sample suggests that if genetic mutations carriers were excluded, contemporary contralateral breast cancer rates might be even lower in these large database reviews. This study does have limitations. It is a retrospective review of a single institution database. Additionally, a median follow-up of 79 months is short compared with the life span of women younger than age 40 years. In the review of the SEER database mentioned earlier, more than 70% of CBC cases occurred before 10 years following diagnosis.12 While longer follow-up and further studies are necessary to confirm the results of this cohort, these results are reassuring that in the modern treatment landscape, contralateral breast cancers are infrequent.
While treatment of breast cancer has improved in this patient population, paradoxically, the rates of contralateral prophylactic mastectomy have increased dramatically. In this study, close to 60% of women aged 40 years and younger underwent BM, and this number appears to be increasing over time. This is consistent with trends in California and nationally in this age group.8,20 While this study did not capture details about the surgical decision-making process, previous studies have identified anxiety and fear of recurrence as factors more frequently associated with patients who elect to undergo BM.20 While young women’s fear of contralateral cancer may be a significant factor in their surgical decision-making, women in this cohort were at more risk of disease recurrence than at risk of a CBC. Providers should discuss the low rate of CBC in young women without genetic mutations in the modern era to help decrease their anxiety and fear. For the majority of young women, BM is not likely to improve overall survival or decrease their risk of a CBC. Providers should emphasize the importance of adjuvant therapy in appropriate patients. Tumor biology and lymph node positivity play an important role in risk of recurrence, whereas operative approach does not significantly impact disease-free survival or overall survival.
Conclusions
With a median follow-up of 79 months, BCS resulted in similar disease-free survival and overall survival as bilateral mastectomy. Invasive contralateral breast cancers were rare (1%) in all women, regardless of operative approach. Despite the rising rates of bilateral mastectomy, the procedure does not enhance survival or diminish disease-free survival in young women with breast cancer.
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30.
de Deus Moura R, Carvalho FM, Bacchi CE. Breast cancer in very young women: clinicopathological study of 149 patients ≤25 years old. Breast. 2015;24(4):461–67.
Azim HA, Jr., Michiels S, Bedard PL, et al. Elucidating prognosis and biology of breast cancer arising in young women using gene expression profiling. Clin Cancer Res. 2012;18(5):1341–51.
Anders CK, Hsu DS, Broadwater G, et al. Young age at diagnosis correlates with worse prognosis and defines a subset of breast cancers with shared patterns of gene expression. J Clin Oncol. 2008;26(20):3324–30.
Bedrosian I, Hu CY, Chang GJ. Population-based study of contralateral prophylactic mastectomy and survival outcomes of breast cancer patients. J Natl Cancer Inst. 2010;102(6):401–9.
Marcheselli R, Marcheselli L, Cortesi L, et al. Risk of second primary malignancy in breast cancer survivors: a nested population-based case-control study. J Breast Cancer. 2015;18(4):378–85.
van den Broek AJ, van ‘t Veer LJ, Hooning MJ, et al. Impact of age at primary breast cancer on contralateral breast cancer risk in BRCA1/2 mutation carriers. J Clin Oncol. 2016;34(5):409–18.
Kurian AW, Lichtensztajn DY, Keegan TH, Nelson DO, Clarke CA, Gomez SL. Use of and mortality after bilateral mastectomy compared with other surgical treatments for breast cancer in California, 1998-2011. JAMA. 2014;312(9):902–14.
Chung A, Huynh K, Lawrence C, Sim MS, Giuliano A. Comparison of patient characteristics and outcomes of contralateral prophylactic mastectomy and unilateral total mastectomy in breast cancer patients. Ann Surg Oncol. 2012;19(8):2600–06.
Yao K, Winchester DJ, Czechura T, Huo D. Contralateral prophylactic mastectomy and survival: report from the National Cancer Data Base, 1998-2002. Breast Cancer Res Treat. 2013;142(3):465–76.
Pesce C, Liederbach E, Wang C, Lapin B, Winchester DJ, Yao K. Contralateral prophylactic mastectomy provides no survival benefit in young women with estrogen receptor-negative breast cancer. Ann Surg Oncol. 2014;21(10):3231–39.
Nichols HB, Berrington de Gonzalez A, Lacey JV, Jr., Rosenberg PS, Anderson WF. Declining incidence of contralateral breast cancer in the United States from 1975 to 2006. J Clin Oncol. 2011;29(12):1564–69.
Pesce CE, Liederbach E, Czechura T, Winchester DJ, Yao K. Changing surgical trends in young patients with early stage breast cancer, 2003 to 2010: a report from the National Cancer Data Base. J Am Coll Surg. 2014;219(1):19–28.
Katipamula R, Degnim AC, Hoskin T, et al. Trends in mastectomy rates at the Mayo Clinic Rochester: effect of surgical year and preoperative magnetic resonance imaging. J Clin Oncol. 2009;27(25):4082–88.
Ye JC, Yan W, Christos PJ, Nori D, Ravi A. Equivalent survival with mastectomy or breast-conserving surgery plus radiation in young women aged <40 years with early-stage breast cancer: a national registry-based Stage-by-Stage Comparison. Clin Breast Cancer. 2015;15(5):390–97.
Maishman T, Cutress R, Hernandez A, Gerty S, Copson ER, Durcan L, Eccles DM. Local recurrence and breast oncological surgery in young women with breast cancer: the POSH observational cohort study. Ann Surg. 2016. doi:10.1097/SLA.0000000000001930.
Plichta JK, Rai U, Tang R, et al. Factors associated with recurrence rates and long-term survival in women diagnosed with breast cancer ages 40 and younger. Ann Surg Oncol. 2016;23(10):3212–20.
Aalders KC, Postma EL, Strobbe LJ et al. Contemporary locoregional recurrence rates in young patients with early-stage breast cancer. J Clin Oncol. 2016;34(18):2107–14.
van Laar C, van der Sangen MJ, Poortmans PM, et al. Local recurrence following breast-conserving treatment in women aged 40 years or younger: trends in risk and the impact on prognosis in a population-based cohort of 1143 patients. Eur J Cancer. 2013;49(15):3093–101.
Rosenberg SM, Sepucha K, Ruddy KJ, et al. Local therapy decision-making and contralateral prophylactic mastectomy in young women with early-stage breast cancer. Ann Surg Oncol. 2015;22(12):3809–15.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Donovan, C.A., Bao, J., Gangi, A. et al. Bilateral Mastectomy as Overtreatment for Breast Cancer in Women Age Forty Years and Younger with Unilateral Operable Invasive Breast Cancer. Ann Surg Oncol 24, 2168–2173 (2017). https://doi.org/10.1245/s10434-017-5856-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5856-9