Abstract
Background
The extent of tumor resection (EOTR) calculated by enhanced T1 changes in glioblastomas has been previously reported to predict survival. However, fluid-attenuated inversion recovery (FLAIR) volume may better represent tumor burden. In this study, we report the first assessment of the dynamics of FLAIR volume changes over time as a predictive variable for post-resection overall survival (OS).
Methods
Contemporary data from 103 consecutive patients with complete imaging and clinical data who underwent resection of newly diagnosed glioblastoma followed by the Stupp protocol between 2010 and 2013 were analyzed. Clinical, radiographic, and outcome parameters were retrieved for each patient, including magnetic resonance imaging (MRI)-based volumetric tumor analysis before, immediately after, and 3 months post-surgery.
Results
OS rate was 17.6 months. A significant incremental OS advantage was noted, with as little as 85 % T1-weighted gadolinium-enhanced (T1Gd)-EOTR measured on contrast-enhanced MRI. Pre- and immediate postoperative FLAIR-based EOTR was not predictive of OS; however, abnormal FLAIR volume measured 3 months post-surgery correlated significantly with outcome when FLAIR residual tumor volume (RTV) was <19.3 cm3 and <46 % of baseline volume (p < 0.0001 for both). Age and isocitrate dehydrogenase (IDH)-1 mutation were predictive of OS (p < 0.0001, Cox proportional hazards).
Conclusions
OS correlated with the immediate postoperative T1Gd-EOTR measured by enhanced T1 MRI, but not by FLAIR volume. Diminished abnormal FLAIR volume at 3 months post-surgery was associated with OS benefit when FLAIR-RTV was <19.3 cm3 or <46 % of baseline. These threshold values provide a new radiological variable that can be used for prediction of OS in patients with glioblastoma immediately after completion of standard chemoradiation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Glioblastomas are the most common primary malignant brain tumors1 and are widely infiltrative, making the extensive resection of these tumors a challenging goal.2 Controversy exists with regard to the extent of tumor resection (EOTR) that should be performed to impact survival;3–5 the EOTR of glioblastomas is mostly defined by calculating the enhanced tumor volume on T1-weighted magnetic resonance imaging (MRI) studies.1,6–10 Previous studies have suggested that resection of more than 78 % of the contrast-enhanced tumor volume is associated with improved survival;1,10 however, the enhanced tumor volume may underestimate the full extent of tumor burden since tumor infiltration into normal brain is known to exist in non-enhanced areas, which are characteristically hyperintense on T2-weighted and fluid-attenuated inversion recovery (FLAIR) sequences.5,9
The aim of this study was to assess the correlation between overall survival (OS) and post-surgical FLAIR residual tumor volume (FLAIR-RTV) and FLAIR-EOTR immediately after surgery and again at 3 months after patients completed a standard Stupp protocol consisting of chemotherapy and radiation therapy.
Methods
This study was approved by the Institutional Review Board (IRB) committee of the Tel Aviv Medical Center (IRB approval number TLV065013), and was based on prospectively collected data of consecutive patients with newly diagnosed glioblastoma undergoing surgical resection at the Tel Aviv Medical Center. From 2010 to 2013, a total of 369 adult patients (age >18 years) with newly diagnosed glioblastoma underwent surgical resection. Patients who had not completed the Stupp protocol or did not have all of the required imaging information were excluded from the study. Also excluded from the analysis were patients who only underwent tumor biopsy, those with infratentorial tumor, and patients with multifocal disease. Overall, 103 patients fulfilled the inclusion criteria and comprised the study group.
Clinical Characteristics
Clinical records of the study patients were retrospectively reviewed. Data of interest included demographics, comorbidities, presenting symptoms, hospital course, and postoperative neurological function. Pathological diagnosis was determined by a neuropathologist and was based on the World Health Organization (WHO) criteria.11 The Karnofsky Performance Scale (KPS) was used to assess preoperative functional status.
Volumetric Analysis
The pre- and postoperative MRIs were obtained and reviewed for each patient. The preoperative tumor volume was measured using T1-weighted gadolinium-enhanced (T1Gd) and FLAIR-MRI (1.5–3 mm axial cuts) studies obtained up to 1 week prior to surgery. Using Brainlab software (BrainLAB, Heimstetten, Germany), the area of contrast enhancement and FLAIR abnormality were calculated for each axial section, and the tumor volume was quantified, in a semi-automated manner, based on the sum of axial areas. The FLAIR and T1Gd-RTVs were calculated in the same manner by evaluating the MRI obtained within the first 48 h following surgery, and 3 months after surgery and the completion of chemoradiation. The T1Gd-RTV and FLAIR-RTV calculations were based on T1Gd and FLAIR abnormalities on the MRI. The volume of blood products rather than residual tumor was confirmed by comparing T1-weighted gadolinium-enhanced and non-enhanced MRIs. The EOTR was calculated using the following formula: (preoperative − postoperative tumor volume)/preoperative tumor volume × 100. Volumetric measurements on the MRI were made by two clinicians unaware of patient outcome, and the area and volumes were computed using Brainlab software. The intraobserver consensus (ICC) of two independent observers was 0.914 (95 % CI 0.872–0.942; p = 0.001). Perioperative mortality was recorded within 30 days after surgery, while postoperative neurological outcome was assessed within 7 days from surgery. OS was calculated from time of surgery to the time of death, and all patients were treated according to the Stupp protocol within 6 weeks from surgery. Patients typically underwent follow-up MRI at 1–3-month intervals and/or if there were new or progressive neurological symptoms.
Statistical Analysis
Descriptive statistics were given as median, mean, and standard deviation (SD) for continuous variables, and as frequency distribution for categorical variables. The Chi square test or Fisher’s exact test was used to examine group differences in categorical variables, while the two-sample t test or Mann–Whitney test was used to compare the groups for continuous variables. A mixed model, repeated measures analysis of variance was performed for repeated measurements, and a multiple logistic regression model was applied to determine which parameters were independently associated with outcome. The model building methods used consisted of forced entry, forward selection, and backward elimination. A multivariate Cox regression analysis was performed to identify predictors independently associated with OS. OS as a function of time after surgery was expressed as Kaplan–Meier plots, and log-rank analysis was used to compare Kaplan–Meier plots. All statistical analyses were performed using SPSS 17.0 for windows (SPSS Inc., Chicago, IL, USA). A p value <0.05 were considered statistically significant.
Results
The clinical characteristics of the 103 patients included in this study are summarized in Table 1. The mean age of patients at diagnosis was 59.6 ± 12.5 years, and there was slight male predominance (n = 66, 64 %). The median KPS prior to surgery was 90, and 82.5 % of patients had a KPS >70. No patient was lost to follow-up. More patients presented with a motor deficit (n = 36, 36 %), followed by a language deficit (n = 33, 32 %) and a cognitive decline (n = 32, 31.1 %). Only 28 (27.2 %) patients suffered from headache. The most common tumor location was the temporal lobe (40 patients, 38.8 %), followed by the frontal lobe (39 patients, 37.9 %), parietal lobe (21 patients, 20.4 %), and occipital lobe (3 patients, 2.9 %). The mean preoperative contrast-enhanced tumor volume (T1Gd) and FLAIR abnormality were 35.3 ± 24.6 cm3 (range 0.3–115.9) and 100.7 ± 55.1 cm3 (range 3.7–222.5), respectively. Forty-five (43.6 %) patients harbored tumors in the right hemisphere, 55 (53.4 %) patients harbored tumors in the left hemisphere, and 3 patients (3 %) had bilateral tumor involvement. All patients underwent image-guided, 5-aminolevulinic acid (5-ALA)-directed microsurgical resection, followed by chemotherapy and radiation therapy (i.e. the Stupp protocol). Thirty-seven (35.9 %) patients underwent awake craniotomy for intraoperative monitoring of language and high cognitive functions. The mean postoperative T1Gd and FLAIR-RTVs, as measured by contrast-enhanced tumor volume and FLAIR, were 4.2 ± 7.4 cm3 (range 0–50.9) and 51.9 ± 35.2 cm3 (range 0.8–182.2), respectively, while the mean postoperative T1Gd and FLAIR-EOTRs, as measured by contrast-enhanced tumor volume and FLAIR, were 89.3 % (range 100–2.1 %) and 48.5 % (range 97.7 %, a twofold increase in volume of FLAIR abnormality), respectively. At 3 months post-resection, the T1Gd tumor volume was 15.3 ± 24 cm3, and 43.5 % of the baseline volume and 3.6-fold of the immediate postoperative volume. For the FLAIR-based calculation, the FLAIR volume at 3 months post-resection was 41.2 ± 50.6 cm3, representing 40.9 % of baseline FLAIR volume and 79.4 % of immediate postoperative FLAIR volume.
By 3 months, all patients were off steroids or were remaining on a minimal dose of dexamethasone 2 mg. Following surgery, nine (8.7 %) patients experienced postoperative complications, including three (2.9 %) patients who had postoperative dysphasia, three (2.9 %) patients who had a new motor deficit, one (0.97 %) patient who had new hemianopsia, and one (0.97 %) patient who developed postoperative hydrocephalus and eventually underwent ventriculoperitoneal shunt placement. In addition, one (0.97 %) patient had wound dehiscence. The median OS for the entire cohort was 17.6 months (range 0.7–55 months).
Clinical Parameters Associated with Overall Survival (OS)
Using the univariate Cox proportional hazards model analysis, the following parameters were found to be significantly associated with survival: age (p = 0.04), KPS (p = 0.006), isocitrate dehydrogenase (IDH)-1 mutation (p = 0.04), bilateral tumor infiltration (p = 0.004), postoperative complications (p = 0.004), T1Gd-RTV (p < 0.0001), postoperative T1Gd-EOTR as measured by contrast-enhancement (p < 0.0001), 3-month postoperative FLAIR volume (p < 0.0001), 3-month postoperative percentage of baseline FLAIR volume (p < 0.0001), and 3-month postoperative T1Gd-RTV (p < 0.0001). A multivariate Cox proportional hazards analysis revealed that age (hazard ratio [HR] 1.04, 95 % confidence interval [CI] 1.014–1.067; p = 0.003), IDH1 mutation (HR 0.07, 95 % CI 0.009–0.55; p = 0.01), T1Gd-RTV (HR 1.04, 95 % CI 1.015–1.058; p = 0.001), T1Gd-EOTR (HR 0.2, 95 % CI 0.86–0.51; p = 0.001), and 3-month postoperative percentage of baseline FLAIR volume (HR 1.017, 95 % CI 1.01–1.024; p = 0.001) were all predictors of OS.
Association Between T1-Weighted Gadolinium-Enhanced Extent of Tumor Resection (T1Gd-EOTR) and OS
The impact of different T1Gd-EOTR cut-off points on OS according to contrast-enhancement was assessed using Kaplan–Meier survival curves. A significant survival advantage was observed with a T1Gd-EOTR of ≥85 % of the enhanced volume (p < 0.0001). The median OS increased with higher T1Gd-EOTRs, while a T1Gd-EOTR < 85 % was associated with a median OS of 8.5 months. Resection of 85–95 % led to a 19.4-month median OS. A T1Gd-EOTR of 95–99 % was associated with a 26.7-month median OS, and a T1Gd-EOTR of 100 % was associated with a 27.5-month median OS (see Table 4; Fig. 3 in the Online Appendix).
Association Between T1Gd-Residual Tumor Volume (RTV) and OS
In the univariate analysis, the T1Gd-RTV strongly correlated with OS immediately following and 3 months after surgery (p < 0.0001). After controlling for factors previously shown to be associated with OS, the multivariate analysis revealed that the T1Gd-RTV remained significantly associated with immediate postoperative OS only (p < 0.0001). The T1Gd-RTV was incrementally evaluated in order to determine the threshold T1Gd-RTV associated with prolonged OS. The maximum T1Gd-RTV that was still associated with improved OS according to the multivariate analysis was 1 cm3 (p = 0.009). The median OS for patients without an T1Gd-RTV or with an T1Gd-RTV of <1 cm3 was 27.5 and 27.4 months, respectively, compared with 16.1 months for patients with an T1Gd-RTV of 1–3 cm3 (p = 0.009), 11.1 months for patients with an T1Gd-RTV of 3–5 cm3 (p < 0.0001), 10.1 months for patients with an T1Gd-RTV of 5–10 cm3 (p = 0.003), and 6.1 months for patients with an T1Gd-RTV of 10–60 cm3 (see Table 5; Fig. 4 in the Online Appendix).
Association between Fluid-Attenuated Inversion Recovery (FLAIR) RTV, EOTR and OS
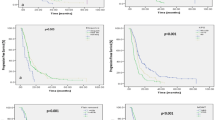
Preoperative and immediate postoperative FLAIR-based EOTR did not correlate with OS; however, the FLAIR volume and percentage of baseline FLAIR volume 3 months after surgery correlated significantly with OS when the FLAIR volume was <19.3 cm3 and the percentage of baseline FLAIR volume was <46 % of baseline (p < 0.0001 for both) (Tables 2, 3, respectively). Patients with a FLAIR volume >19.3 cm3 at 3 months survived 13.4 months compared with 26.7 months for patients with a FLAIR volume of ≤19.3 cm3 (p < 0.0001) (Fig. 1). Similarly, patients with a percentage of baseline FLAIR volume of <46 % had a median OS of 26.7 months, while patients with a percentage of baseline FLAIR volume >46 % had a significantly shorter survival (13.5 months; p < 0.0001) (Fig. 2).
Overall survival by FLAIR volume 3 months postoperatively. The median overall survival for patients who had a residual FLAIR volume of <19.3 cm3 (blue line) was 26.6 months compared with 13.5 months (p < 0.0001) for patients with a residual FLAIR volume of >19.3 cm3 (green line). FLAIR fluid-attenuated inversion recovery
Overall survival by percentage of baseline FLAIR volume 3 months postoperatively. The median overall survival for patients who had a FLAIR abnormality of ≤46 % of baseline (blue line) was 19.4 months compared with 12.6 months when the residual tumor volume was >46 % (p < 0.0001) (green line). FLAIR fluid-attenuated inversion recovery
Association Between FLAIR, T1Gd-RTV and OS
The T1Gd-RTV measured immediately post-surgery and at 3 months post-surgery correlated significantly with the FLAIR volume at 3 months after surgery. The Pearson correlation showed a modest but significant correlation between T1Gd-RTV when measured immediately postoperatively and 3 months after surgery as measured by FLAIR volume (R = 0.326, p = 0.002). Using the Pearson correlation test, a stronger correlation was found between tumor volume measured by T1Gd and FLAIR 3 months after surgery (R = 0.855, p = 0.001). It emerged that 57.4 % of patients with <15 % residual tumor enhancement also had a <46 % FLAIR abnormality at 3 months after surgery compared with baseline values (Fisher’s exact test, p = 0.01).
Discussion
The current study was carried out on a contemporary homogenous group of 103 patients with newly diagnosed glioblastoma who underwent tumor resection followed by the Stupp protocol. The median OS for the entire cohort was 17.6 months, and the T1Gd-RTV, T1Gd-EOTR, and 3-month postoperative FLAIR and percentage of baseline FLAIR volumes were all predictors of OS. Among all prognostic factors known to be associated with OS in glioblastoma patients, EOTR is the only one that is modifiable.12,13 There is abundant class II and III evidence but not class I evidence, which precludes the validation of criteria for guiding glioblastoma EOTR.1,10,14–31 The contrast-enhanced region in a glioblastoma is used to delineate the tumor burden; however, due to the infiltrative nature of this lesion, the contrast-enhanced volume underestimates the true tumor extent. Thus, T2 and FLAIR sequences, and not solely the enhanced T1 sequence, are used for radiation planning.32 Importantly, the preoperative and immediate postoperative FLAIR abnormality is a mixture of tumor-associated edema and true tumor infiltration. Moreover, surgical manipulation may create immediate postoperative MRI areas of FLAIR abnormality that are indistinguishable from true tumor infiltration. Our results support this likelihood. Neither FLAIR abnormalities measured by preoperative MRIs nor those measured by immediate postoperative MRIs correlated with OS. However, after resolution of the postoperative changes when measured 3 months postoperatively, the volume of FLAIR abnormality appeared to better represent the true tumor extension. On the other hand, even at 3 months post-surgery, the volume of a FLAIR abnormality may be affected by treatment-related changes. This is especially relevant for larger tumors with larger areas of irradiation, which could theoretically lead to more FLAIR alterations after treatment. In opposition to our results, Grabowski et al.9 and, more recently, Li et al.33 reported that the FLAIR-RTV measured immediately postoperation was a significant predictor of OS. Grabowski et al.9 correctly noted that the preoperative mass effect on surrounding tissue, along with intraoperative manipulation of tissue within the surgical site, may create an abnormal, edema-related T2/FLAIR signal that can persist from days to weeks after surgery. In fact, an unknown portion of the measured abnormal T2/FLAIR-RTV may represent edema that will eventually resolve, and not tumor infiltration. Grabowski et al. describe this feature as a methodological shortcoming of their study. Nevertheless, the reason for the discrepancy in results is not clear. In the current study, we demonstrated for the first time that the FLAIR volume and the percentage of baseline FLAIR volumes when measured 3 months after surgery are predictive of OS. We also delineated the FLAIR volume thresholds at 3 months postoperatively that correlate with OS.
Limitations
The limitations of any retrospective analysis also apply to our study, particularly with respect to the risk of selection bias; however, such risk of selection bias may be minimized by including only patients who were scheduled for an attempted gross total resection of their tumor. We used a quantitative semi-automated segmentation algorithm to measure a FLAIR abnormality without differentiation between tumor and edema or operative artifacts. Such differentiation is not feasible with current imaging technologies. The impact of the so-called ‘pseudo-progression’ on OS was not addressed in this work since it merits a separate study with longer imaging and clinical follow-up. In addition, our volumetric data were available before, immediate after, and 3 months postoperatively, but not later on. Finally, the conclusions presented in our study should be validated in a larger cohort of patients in order to assess the predictive value of FLAIR volume in patients with glioblastoma.
Conclusions
This is the first study to demonstrate the dynamics of FLAIR volume changes over time as a predictive variable for OS. Immediate postoperative EOTR measured by enhanced T1 MRI, but not by FLAIR volume, was found to significantly correlate with OS. An abnormal FLAIR volume at 3 months after surgery was associated with an OS. This finding provides a new radiological variable that can be used for prediction of OS in patients with glioblastoma.
References
Lacroix M, Abi-Said D, Fourney DR, et al. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg. 2001;95(2):190–98.
Barker FG 2nd, Prados MD, Chang SM, et al. Radiation response and survival time in patients with glioblastoma multiforme. J Neurosurg. 1996;84(3):442–8.
Dea N, Fournier-Gosselin MP, Mathieu D, Goffaux P, Fortin D. Does extent of resection impact survival in patients bearing glioblastoma? Can J Neurol Sci. 2012;39(5):632–7.
Kawano H, Hirano H, Yonezawa H, et al. Improvement in treatment results of glioblastoma over the last three decades and beneficial factors. Br J Neurosurg. 2015;29(2):206–12.
Marko NF, Weil RJ, Schroeder JL, Lang FF, Suki D, Sawaya RE. Extent of resection of glioblastoma revisited: personalized survival modeling facilitates more accurate survival prediction and supports a maximum-safe-resection approach to surgery. J Clin Oncol. 2014;32(8):774–82.
Chaichana KL, Cabrera-Aldana EE, Jusue-Torres I, et al. When gross total resection of a glioblastoma is possible, how much resection should be achieved? World Neurosurg. 2014;82(1–2):e257–65.
Smets T, Lawson TM, Grandin C, Jankovski A, Raftopoulos C. Immediate post-operative MRI suggestive of the site and timing of glioblastoma recurrence after gross total resection: a retrospective longitudinal preliminary study. Eur Radiol. 2013;23(6):1467–77.
Chaichana KL, Jusue-Torres I, Navarro-Ramirez R, et al. Establishing percent resection and residual volume thresholds affecting survival and recurrence for patients with newly diagnosed intracranial glioblastoma. Neuro Oncol. 2014;16(1):113–22.
Grabowski MM, Recinos PF, Nowacki AS, et al. Residual tumor volume versus extent of resection: predictors of survival after surgery for glioblastoma. J Neurosurg. 2014;121(5):1115–23.
Sanai N, Polley MY, McDermott MW, Parsa AT, Berger MS. An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg. 2011;115(1):3–8.
Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114(2):97–109.
Oppenlander ME, Wolf AB, Snyder LA, et al. An extent of resection threshold for recurrent glioblastoma and its risk for neurological morbidity. J Neurosurg. 2014;120(4):846–53.
Gonda DD, Warnke P, Sanai N, Taich Z, Kasper EM, Chen CC. The value of extended glioblastoma resection: insights from randomized controlled trials. Surg Neurol Int. 2013;4:110.
Curran WJ Jr, Scott CB, Horton J, et al. Does extent of surgery influence outcome for astrocytoma with atypical or anaplastic foci (AAF)? A report from three Radiation Therapy Oncology Group (RTOG) trials. J Neuro Oncol. 1992;12(3):219–27.
Dinapoli RP, Brown LD, Arusell RM, et al. Phase III comparative evaluation of PCNU and carmustine combined with radiation therapy for high-grade glioma. J Clin Oncol. 1993;11(7):1316–21.
Hollerhage HG, Zumkeller M, Becker M, Dietz H. Influence of type and extent of surgery on early results and survival time in glioblastoma multiforme. Acta Neurochir (Wien). 1991;113(1–2):31–7.
Huber A, Beran H, Becherer A, Prosenc N, Witzmann A. Supratentorial glioma: analysis of clinical and temporal parameters in 163 cases [in German]. Neurochirurgia (Stuttg). 1993;36(6):189–93.
Jeremic B, Grujicic D, Antunovic V, Djuric L, Stojanovic M, Shibamoto Y. Influence of extent of surgery and tumor location on treatment outcome of patients with glioblastoma multiforme treated with combined modality approach. J Neuro Oncol. 1994;21(2):177–85.
Keles GE, Anderson B, Berger MS. The effect of extent of resection on time to tumor progression and survival in patients with glioblastoma multiforme of the cerebral hemisphere. Surg Neurol. 1999;52(4):371–79.
Keles GE, Chang EF, Lamborn KR, et al. Volumetric extent of resection and residual contrast enhancement on initial surgery as predictors of outcome in adult patients with hemispheric anaplastic astrocytoma. J Neurosurg. 2006;105(1):34–40.
Kowalczuk A, Macdonald RL, Amidei C, et al. Quantitative imaging study of extent of surgical resection and prognosis of malignant astrocytomas. Neurosurgery. 1997;41(5):1028–36.
Lamborn KR, Chang SM, Prados MD. Prognostic factors for survival of patients with glioblastoma: recursive partitioning analysis. Neuro Oncol. 2004;6(3):227–35.
Nitta T, Sato K. Prognostic implications of the extent of surgical resection in patients with intracranial malignant gliomas. Cancer. 1995;75(11):2727–31.
Nomiya T, Nemoto K, Kumabe T, Takai Y, Yamada S. Prognostic significance of surgery and radiation therapy in cases of anaplastic astrocytoma: retrospective analysis of 170 cases. J Neurosurg. 2007;106(4):575–81.
Pope WB, Sayre J, Perlina A, Villablanca JP, Mischel PS, Cloughesy TF. MR imaging correlates of survival in patients with high-grade gliomas. AJNR Am J Neuroradiol. 2005;26(10):2466–74.
Simpson JR, Horton J, Scott C, et al. Influence of location and extent of surgical resection on survival of patients with glioblastoma multiforme: results of three consecutive Radiation Therapy Oncology Group (RTOG) clinical trials. Int J Radiat Oncol Biol Phys. 1993;26(2):239–44.
Stark AM, Nabavi A, Mehdorn HM, Blomer U. Glioblastoma multiforme-report of 267 cases treated at a single institution. Surg Neurol. 2005;63(2):162–169.
Tortosa A, Vinolas N, Villa S, et al. Prognostic implication of clinical, radiologic, and pathologic features in patients with anaplastic gliomas. Cancer. 2003;97(4):1063–71.
Ushio Y, Kochi M, Hamada J, Kai Y, Nakamura H. Effect of surgical removal on survival and quality of life in patients with supratentorial glioblastoma. Neurol Med Chir (Tokyo). 2005;45(9):454–60.
Vecht CJ, Avezaat CJ, van Putten WL, Eijkenboom WM, Stefanko SZ. The influence of the extent of surgery on the neurological function and survival in malignant glioma. A retrospective analysis in 243 patients. J Neurol Neurosurg Psychiatry. 1990;53(6):466–71.
Warnke PC, Kreth FW, Scheremet R, Ostertag CB. Response to Drs. Simpson, et al.: Influence of location and extent of surgical resection on survival of patients with glioblastoma multiforme: results of three consecutive Radiation Therapy Oncology Group clinical trials. Int J Radiat Oncol Biol Phys. 1994;29(1):220.
Ali AN, Ogunleye T, Hardy CW, Shu HK, Curran WJ, Crocker IR. Improved hippocampal dose with reduced margin radiotherapy for glioblastoma multiforme. Radiat Oncol. 2014;9:20.
Li YM, Suki D, Hess K, Sawaya R. The influence of maximum safe resection of glioblastoma on survival in 1229 patients: can we do better than gross-total resection? J Neurosurg. 2016;124(4):977–88.
Acknowledgment
The authors would like to thank Esther Eshkol, MA, for editorial assistance.
Disclosures
Rachel Grossman, Nir Shimony, Dror Shir, Tal Gonen, Razi Sitt, Tali Jonas Kimchi, Carmit Ben Harosh, and Zvi Ram have no disclosures to declare.
Funding
No funding was used to assist in the preparation of this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Grossman, R., Shimony, N., Shir, D. et al. Dynamics of FLAIR Volume Changes in Glioblastoma and Prediction of Survival. Ann Surg Oncol 24, 794–800 (2017). https://doi.org/10.1245/s10434-016-5635-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5635-z