Abstract
Background
Recent attention has focused on the ability to rescue patients from postoperative complications and prevent short-term mortality. However, it is unknown whether patients rescued from complications after complex cancer resections have long-term survival outcomes similar to those of patients without complications.
Methods
From 2005 to 2009 Surveillance, Epidemiology, and End Results (SEER)-Medicare data, the study identified elderly patients who underwent resection for cancers of the esophagus, lung, or pancreas. The association of risk-adjusted long-term survival with serious complications, minor complications, and no complications was analyzed.
Results
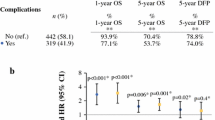
The study included 905 patients with esophageal cancer, 12,395 patients with lung cancer, and 1966 patients with pancreatic cancer. The serious complication rates were respectively 17.4, 9.5 and 11.8 %. The patients with serious complications had lower 5-year survival rates than those with no complications even if they were rescued and survived 30 days (20 vs 43 % for esophagus, 29 vs 54 % for lung, and 10 vs 21 % for pancreas cancer). Even after patients who died within 180 days after surgery were excluded from the analysis, a decrement in risk-adjusted long-term survival was observed among the patients with serious complications after all three procedures. The association between complications and long-term survival was not explained by differences in receipt of adjuvant chemotherapy
Conclusion
Patients who undergo complex cancer resection and experience serious complications have diminished long-term survival, even if they are “rescued” from their complications. This finding persists even when deaths within 6 months after surgery are excluded from the analysis. Metrics of surgical success should consider terms beyond 30 and even 90 days as well as the long-term consequences of surgical complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Variation in 30-day mortality after complex surgical procedures is attributable in part to differences in the abilities of hospitals to manage complications effectively and prevent postoperative death. In fact, high- and low-mortality hospitals have similar complication rates but differ chiefly in their ability to “rescue” patients after complications occur.1,2 For patients undergoing cancer resection, however, 30-day mortality metrics provide an incomplete assessment of the impact that postoperative complications have on longer-term survival. For example, delayed mortality in the 30- to 90-day window or even beyond may still be attributable to complications. Alternately, patients may survive their complications but remain so debilitated that they cannot complete adjuvant therapy, potentially compromising their long-term survival.3 Finally, postoperative complications may have immunomodulatory effects that influence tumor recurrence and disease-free survival.4,5
Previous studies have documented decreased long-term survival for patients with postoperative complications after resection of biliary,6 colorectal7–9 esophageal,10 gastric,11,12 hepatocellular,13 lung,14,15 and pancreatic cancers.16 However, most of these studies excluded only patients who died within 30 days after surgery and therefore may have underestimated the true short-term mortality attributable to complications. Studies that excluded deaths within 90 days found conflicting results.6,7,10,17,18 Furthermore, although postoperative complications are associated with decreased receipt of adjuvant chemotherapy,3,16 the association of chemotherapy use with long-term survival has been inconsistently examined in prior studies and remains unclear. Finally, most of these prior studies used institutional databases, raising concerns about selection bias and generalizability of the results.
We aimed to analyze population-based registry data on patients undergoing three different complex cancer resections, namely, esophagectomy, pulmonary lobectomy, and pancreatectomy. Using these robust, nationally representative data, we sought to quantify the impact of postoperative complications on long-term survival, assess the influence of surgical mortality beyond 30 days, and explore the role of adjuvant chemotherapy as a mediator of this relationship.
Methods
Data Source and Study Cohort
The primary data source was Surveillance, Epidemiology, and End Results (SEER) cancer registry data linked with national Medicare claims.19 We identified patients 65 years of age and older with a diagnosis of esophageal cancer, non-small cell lung cancer, or pancreatic cancer (excluding neuroendocrine tumors) between 2005 and 2009 who underwent a surgical resection with curative intent.
Only the first cancer-directed surgical procedure after diagnosis was considered. We included only patients with continuous, complete (parts A & B), fee-for-service Medicare enrollment at least 6 months before surgery and at least 12 months after surgery. Patients with metastatic disease or unknown extent of disease were excluded from the study. Patients with a preoperative hospital stay longer than 2 days were excluded, as also were patients with missing stage data.
Outcomes and Risk Adjustment
Complications were identified from claims using an algorithm that includes cardiac, pulmonary, thromboembolic, and infectious complications.20–22 Relevant codes were derived from Medicare claims data and validated by multidisciplinary physician review of patient charts as part of the Complications Screening Program.20,21 “Serious complications” were defined as those associated with a hospital length of stay greater than the 75th percentile for that procedure.23 Survival after surgery was determined primarily using Medicare data, with SEER data used if Medicare data were incomplete.
The covariates used for risk adjustment were patient sex, age, American Joint Committee on Cancer (AJCC) disease stage, and comorbidity score. Comorbidity burden was quantified using the Charlson Comorbidity Index.24,25 Other demographic and clinicopathologic variables were ascertained from SEER.
To account for differences in resection procedures for similar malignancies (e.g., pancreaticoduodenectomy vs distal pancreatectomy), we also adjusted for the primary procedure code. For esophageal cancer, a sensitivity analysis included adjustment for histologic subtype (adenocarcinoma vs squamous cell cancer), but this did not affect our primary conclusions.
Statistical Analysis
Survival analyses were performed with Cox proportional hazards models using robust standard errors to account for clustering by hospital. Statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC, USA). The study protocol was deemed exempt from review by the University of Michigan Institutional Review Board. All analyses complied with the SEER-Medicare Data Use Agreement.
Results
The analysis included 905 patients with esophageal cancer, 12,395 patients with lung cancer, and 1966 patients with pancreatic cancer (Table 1). The incidence of serious complications ranged from 9.5 % for lung cancer resection to 17.4 % for esophageal cancer resections. Mortality rates at 30 days ranged from 3.3 % for lung cancer resections to 6.2 % for esophageal cancer resections, indicating that the majority of patients experiencing postoperative complications were rescued from early mortality. However, subsequent mortality at 90 and 180 days was significant, with the 180-day mortality rate rising to approximately three times the 30-day mortality rate across all procedures.
Initial survival analyses focused only on patients who survived at least 30 days after surgery, such that patients with complications who were not rescued would be excluded. Occurrence of complications was associated with poorer long-term survival across all disease stages and sites, even after patients who died within 30 days were excluded (Fig. 1). For example, among patients with stage 1 lung cancer, 5-year survival decreased from 62 % (median, 79 months) for those without a complication to 33 % (median, 33 months) for those rescued from a serious complication. Among patients with stage 1 pancreatic cancer, 5-year survival decreased from 45 % (median, 54 months) for those without a complication to 17 % (median, 15 months) for those rescued from a serious complication.
Multivariable analyses then were performed to adjust for other known determinants of survival, such as disease stage and comorbidity (Table 2). Again, patients who died within 30 days were excluded. The risk-adjusted survival of patients with minor complications did not differ appreciably from the survival of those without complications, although a statistically significant difference was observed for lung cancer. However, patients with serious complications had significantly worse risk-adjusted long-term survival across all three procedures, with hazard ratios ranging from 1.57 for pancreatic cancer to 2.55 for esophageal cancer.
Because mortality attributable to postoperative complications can occur beyond 30 days, additional analyses focused only on those patients who survived at least 90 and 180 days (Table 3). Although some of the effect of complications on mortality was attenuated with longer intervals after surgery, a persistent and significant effect of complications on long-term survival remained. Even when only the patients who survived 180 days after surgery were considered, those with serious complications had significantly worse risk-adjusted long-term survival across all three procedures, with hazard ratios ranging from 1.31 for pancreatic cancer to 1.63 for esophageal cancer.
There were differences in receipt of chemotherapy based on occurrence of complications (Table 4). For example, among patients with stage 2 pancreatic cancer, adjuvant chemotherapy was administered to 64 % of those without complications but only 33 % of those with serious complications (p < 0.001). Among patients with stage 2 lung cancer, adjuvant chemotherapy was given to 53 % of those without complications but only 19 % of those with serious complications (p < 0.001). However, when receipt of chemotherapy was added to the multivariable survival models, its effect was not significant in any analysis, and the hazard ratio estimates for the effects of complications remained virtually unchanged.
Discussion
In this population-based study of long-term survival after three different complex cancer resections, patients with serious postoperative complications experienced significantly inferior long-term survival compared with patients who had no complications. These results were remarkably consistent across all three procedures, with an increased risk for death after 30 days of 50–150 %. Although patients with serious complications had lower rates of receiving adjuvant chemotherapy, chemotherapy use alone did not explain the differences in long-term survival.
Previous studies have been inconsistent in considering the effects of late mortality after 30 days that still may be related to complications. Our results demonstrated persistent differences in survival not only when patients who avoided 30-day mortality from complications were considered, but also when those who survived at least 90 and even 180 days after surgery were considered. These findings strongly suggest an association between occurrence of serious complications and long-term survival that is not explained by surgical mortality in the 30-, 90-, or even 180-day window after surgery. Our results are consistent with those of two recent studies that demonstrated decreased long-term survival of 90-day survivors among patients with complications after esophageal and colorectal cancer resections.7,10 As in our study, differences in receipt of adjuvant therapy did not explain the decrement in survival.
Failure to rescue or mortality among patients with complications has been widely studied and used as a hospital quality measure.26,27 Because high- and low-mortality hospitals have similar complication rates, the validity of complication rates as a marker of hospital quality has been questioned.1 The association between occurrence of complications and long-term survival of patients undergoing surgery for cancer, however, suggests that complication rates might need to be reconsidered as one element in assessing the overall quality of cancer care. Clearly, low surgical mortality remains the cornerstone of quality in surgical oncology. However, among low-mortality hospitals, patients with low complication rates may achieve superior oncologic outcomes.
Several limitations to our study should be noted. First, we used administrative data rather than clinical registry data to detect complications. Although this approach sacrifices some clinical detail, our definition of serious complications (i.e., complications associated with a hospital length of stay greater than the 75th percentile) is likely to be both sensitive and specific for adverse postoperative events.23 We performed risk adjustment using available claims data, which are inherently limited for this purpose.19 In particular, residual confounding is of concern because patients more prone to complications also may be prone to poorer long-term survival. However, we believe that the magnitude and consistency of the phenomenon we observed across three different procedures are unlikely to be spurious results due to inadequate risk adjustment. Similarly, we were unable to ascertain cause of death. However, late deaths for these poor-prognosis cancers are likely to be cancer related.
The mechanism by which postoperative complications and long-term survival may be linked is unclear. As noted earlier, the association may simply be the result of residual confounding. However, the occurrence of certain postoperative complications, such as pancreatic fistula, should in theory be unrelated to other comorbidities that have an impact on survival. Additionally, some studies have found that infectious complications in particular may have a negative impact on survival,5,7,10,15,28 suggesting that immunomodulatory effects may result in early cancer recurrence29–32 Inability to receive chemotherapy also may theoretically mediate differences in survival, although this was not the case in our study.
Complications after complex cancer surgery will never be completely eliminated, although avoiding them remains a worthwhile goal. Surgical and medical oncologists should be aware, however, that patients who do experience complications may have consequences that extend well beyond the postoperative period. The concept of “rescue” as defined by avoidance of mortality is not precise enough to capture the full effect of postoperative complications on patient outcomes. Further work is needed to understand the mechanism of death in these patients and whether intensified surveillance may be of benefit. Policymakers and providers also should be aware of this phenomenon in evaluating the quality of cancer care.
References
Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009;361:1368–75.
Wong SL, Revels SL, Yin H, et al. Variation in hospital mortality rates with inpatient cancer surgery. Ann Surg. 2015;261:632–6.
Hendren S, Birkmeyer JD, Yin H, et al. Surgical complications are associated with omission of chemotherapy for stage III colorectal cancer. Dis Colon Rectum. 2010;53:1587–93.
Okamura A, Takeuchi H, Matsuda S, et al. Factors affecting cytokine change after esophagectomy for esophageal cancer. Ann Surg Oncol. 2015;22:3130–5.
Mokart D, Giaoui E, Barbier L, et al. Postoperative sepsis in cancer patients undergoing major elective digestive surgery is associated with increased long-term mortality. J Crit Care. 2016;31:48–53.
Spolverato G, Yakoob MY, Kim Y, et al. Impact of complications on long-term survival after resection of intrahepatic cholangiocarcinoma. Cancer. 2015;121:2730–9.
Artinyan A, Orcutt ST, Anaya DA, et al. Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer: a study of 12,075 patients. Ann Surg. 2015;261:497–505.
Cunsolo A, Bragaglia RB, Petrucci C, et al. Survival and complications after radical surgery for carcinoma of the rectum. J Surg Oncol. 1989;41:27–32.
Mirnezami A, Mirnezami R, Chandrakumaran K, et al. Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg. 2011;253:890–9.
Markar S, Gronnier C, Duhamel A, et al. The impact of severe anastomotic leak on long-term survival and cancer recurrence after surgical resection for esophageal malignancy. Ann Surg. 2015;262:972–80.
Li QG, Li P, Tang D, et al. Impact of postoperative complications on long-term survival after radical resection for gastric cancer. World J Gastroenterol. 2013;19:4060–5.
Mita K, Ito H, Hashimoto M, et al. Postoperative complications and survival after gastric cancer surgery in patients older than 80 years of age. J Gastrointest Surg. 2013;17:2067–73.
Zhou YM, Zhang XF, Li B, et al. Postoperative complications affect early recurrence of hepatocellular carcinoma after curative resection. BMC Cancer. 2015;15:689.
Kodama K, Higashiyama M, Yokouchi H, et al. Survival and postoperative complications after extended surgery for non-small cell lung cancer: a retrospective study. Jpn J Thorac Cardiovasc Surg. 1999;47:546–51.
Andalib A, Ramana-Kumar AV, Bartlett G, et al. Influence of postoperative infectious complications on long-term survival of lung cancer patients: a population-based cohort study. J Thorac Oncol. 2013;8:554–61.
Labori KJ, Katz MH, Tzeng CW, et al. Impact of early disease progression and surgical complications on adjuvant chemotherapy completion rates and survival in patients undergoing the surgery first approach for resectable pancreatic ductal adenocarcinoma: a population-based cohort study. Acta Oncol. 2015;1–13.
Aahlin EK, Trano G, Johns N, et al. Risk factors, complications, and survival after upper abdominal surgery: a prospective cohort study. BMC Surg. 2015;15:83.
Pugalenthi A, Protic M, Gonen M, et al. Postoperative complications and overall survival after pancreaticoduodenectomy for pancreatic ductal adenocarcinoma. J Surg Oncol. 2016;113:188–93.
Nathan H, Pawlik TM. Limitations of claims and registry data in surgical oncology research. Ann Surg Oncol. 2008;15:415–23.
Iezzoni LI, Daley J, Heeren T, et al. Identifying complications of care using administrative data. Med Care. 1994;32:700–15.
Weingart SN, Iezzoni LI, Davis RB, et al. Use of administrative data to find substandard care: validation of the complications screening program. Med Care. 2000;38:796–806.
Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Ann Surg. 2009;250:1029–34.
Osborne NH, Nicholas LH, Ryan AM, et al. Association of hospital participation in a quality reporting program with surgical outcomes and expenditures for Medicare beneficiaries. JAMA. 2015;313:496–504.
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–83.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9.
Silber JH, Williams SV, Krakauer H, et al. Hospital and patient characteristics associated with death after surgery: a study of adverse occurrence and failure to rescue. Med Care. 1992;30:615–29.
Silber JH, Romano PS, Rosen AK, et al. Failure-to-rescue: comparing definitions to measure quality of care. Med Care. 2007;45:918–25.
Tokunaga M, Tanizawa Y, Bando E, et al. Poor survival rate in patients with postoperative intraabdominal infectious complications following curative gastrectomy for gastric cancer. Ann Surg Oncol. 2013;20:1575–83.
Doan HQ, Bowen KA, Jackson LA, et al. Toll-like receptor 4 activation increases Akt phosphorylation in colon cancer cells. Anticancer Res. 2009;29:2473–8.
Goldfarb Y, Sorski L, Benish M, et al. Improving postoperative immune status and resistance to cancer metastasis: a combined perioperative approach of immunostimulation and prevention of excessive surgical stress responses. Ann Surg. 2011;253:798–810.
Hsu RY, Chan CH, Spicer JD, et al. LPS-induced TLR4 signaling in human colorectal cancer cells increases beta1 integrin-mediated cell adhesion and liver metastasis. Cancer Res. 2011;71:1989–98.
Pierce BL, Ballard-Barbash R, Bernstein L, et al. Elevated biomarkers of inflammation are associated with reduced survival among breast cancer patients. J Clin Oncol. 2009;27:3437–44.
Disclosure
Dr. Sandra L. Wong was supported by AHRQ1K08 HS20937-01 and American Cancer Society RSG-12-269-01-CPHPS.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nathan, H., Yin, H. & Wong, S.L. Postoperative Complications and Long-Term Survival After Complex Cancer Resection. Ann Surg Oncol 24, 638–644 (2017). https://doi.org/10.1245/s10434-016-5569-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5569-5