Abstract
Objective
To compare long-term survival outcomes and patterns of recurrence of laparoscopic radical hysterectomy (LRH) and open radical hysterectomy (ORH) in early-stage cervical adenocarcinoma.
Methods
The medical records of 293 patients with stage IA2-IIA cervical adenocarcinomas who underwent radical hysterectomy were retrospectively reviewed.
Results
In total, 186 patients underwent LRH and 107 underwent ORH. There was no difference between the two surgery groups in clinicopathologic characteristics. There were no differences in disease-free survival (DFS) and overall survival (OS) between the LRH and ORH groups (88.7 vs. 84.1 %, P = 0.725; and 93.0 vs. 86.9 %, P = 0.735) for univariate analysis and multivariate analysis after adjusting for other significant prognostic factors. There was no difference in the patterns of recurrence between the two surgery groups (P = 0.220). The median time interval between surgery and the first recurrence were 25 months (range, 3–100 months) for LRH group and 14 months (range, 3–128 months) for ORH group (P = 0.230). The LRH group showed significantly fewer postoperative complications (P < 0.001), less estimated blood loss (P < 0.001), faster bowel movement recovery (P < 0.001), shorter postoperative hospital stay (P < 0.001), and a lower rate of wound dehiscence, ileus, lymphedema, infected lymphocele, and pelvic abscess (P = 0.004, 0.011, 0.017, and 0.040, respectively).
Conclusions
LRH has comparable survival outcomes with ORH and did not affect the pattern of recurrence in early-stage adenocarcinoma of the uterine cervix. The surgical outcomes were more favorable than ORH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cervical cancer is the third most common cancer and the fourth most common cause of cancer death in women worldwide.1 It also is the fifth and eighth most common cancer and cause of cancer death in Korean women.2,3 After squamous cell carcinoma, which comprises 75 % of all cases of cervical cancer, adenocarcinoma is, at 15 %, the second most common histologic type.4 Recently, the incidence of adenocarcinoma has increased, especially in young women between 20 and 40 years of age, whereas the incidence of squamous cell carcinoma has decreased.5–7 Recent studies show an 18.5–27 % incidence of adenocarcinoma, whereas older studies showed an incidence of 5 %.8–10 The incidence of the squamous cell carcinoma has decreased recently because of the adoption of nationwide screening programs for cervical cancer using Papanicolaou smear and human papillomavirus (HPV) tests and the use of the HPV vaccine.11–13
There is no difference in the treatment between cervical squamous cell carcinoma and adenocarcinoma in most treatment guidelines. However, although many previous studies dealing with cervical cancer included adenocarcinoma cases, patients with adenocarcinoma constituted only a small portion of their study population and the generalization of the results is thus not reasonable. In addition, recent studies suggested that adenocarcinoma is associated with higher rate of ovarian metastasis and positive peritoneal cytology and higher tendency of peritoneal carcinomatosis and hematogenous metastasis than squamous cell carcinoma.11,14–16 Therefore, unique investigation of its clinicopathologic characteristics and their application to the therapeutic strategy is needed.
Because most adenocarcinomas of the uterine cervix are diagnosed in younger women at an early stage, radical hysterectomy is the mainstay of treatment.17,18 Laparoscopic radical hysterectomy (LRH) has better surgical outcomes, including a smaller skin incision, less blood loss, less postoperative pain, shorter postoperative hospital stay, faster recovery, and fewer postoperative complications with similar intraoperative complications and survival outcomes compared with open radical hysterectomy (ORH) in early cervical cancer.19–21 However, no studies focused on the role of LRH in early cervical adenocarcinoma, although many previous studies included a fraction of patients with early cervical adenocarcinoma in their series. The purpose of this study was to compare the long-term survival outcomes and patterns of recurrence of LRH and ORH in early-stage adenocarcinoma of the uterine cervix.
Methods
The medical records of patients with International Federation of Obstetrics and Gynecology (FIGO) stage IA2-IIA cervical adenocarcinomas who underwent LRH or ORH at Asan Medical Center, Seoul, Korea, between 1997 and 2013 were retrospectively reviewed under the approval of the Institutional Review Board. Radical surgery was performed in all patients with FIGO stage IA2-IIA2 cervical cancer in our institution, unless the patient refused surgery and wanted radiation and/or chemotherapy or there were any uncontrolled, underlying medical problems. We excluded cases with incomplete or missing medical records or inadequate follow-up after surgery.
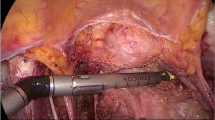
ORH was performed through a low midline incision with periumbilical extension according to the Piver-Rutledge type 3 hysterectomy procedure.22 Bilateral systematic pelvic lymph node dissection was performed in all patients. Enlarged or suspicious lymph nodes were sent for frozen diagnosis during surgery. If there was pelvic lymph node metastasis that was revealed using analysis of a frozen section during surgery, paraaortic lymph node dissection was performed to the inferior mesenteric artery level. If there was paraaortic lymph node metastasis below the inferior mesenteric artery, paraaortic lymph node dissection was extended up to the left renal vein level. LRH was performed using the four trocar system as previously described.23 Two 12-mm trocars were placed at the umbilicus and left lower quadrant and two 5-mm trocars were placed at the right lower quadrant and suprapubic area. Cohen cannula was used as a uterine manipulator. The extent of the surgery and the surgical technique for LRH was the same as for ORH except for a midline incision of the abdomen. Vaginal cuff was closed vaginally in LRH. Our treatment policy is to complete LRH or ORH even if parametrial invasion or lymph node metastasis is encountered during surgery. Ovaries were preserved in young women, and bilateral salpingo-oophorectomy was considered in perimenopausal or postmenopausal women or women with complex ovarian tumors.
Patients with intermediate-risk factors, such as bulky tumors, deep cervical stromal invasion, or lymphovascular invasion in accordance with Gynecologic Oncology Group 92 criteria, were recommended for adjuvant radiotherapy.24 Patients with high-risk factors (parametrial invasion, lymph node metastasis, or resection margin involvement) were recommended for adjuvant concurrent chemoradiation therapy (CCRT). After discussion with their physician, some patients received adjuvant chemotherapy.
Patients were divided into LRH and ORH groups, and long-term survival outcomes and the pattern of recurrence were compared and analyzed. Surgical outcomes also were compared between LRH and ORH. Adverse events occurring within 1 month after surgery were regarded as postoperative complications. We defined febrile morbidity as a body temperature of 38 °C or higher after the first day of surgery on more than two occasions separated by at least a 4-h interval without any specific cause. In general, we removed the Foley catheter from the patients at 7 days after surgery. Bladder dysfunction was defined as voiding difficulty requiring reinsertion of the Foley catheter or clean intermittent catheterization. A return of bowel sounds and flatus passage indicated that bowel movement had returned; meals could then be given to the patients. Patients were followed up after the completion of treatment every 3 months for the first 2 years, every 6 months during the next 3 years, and then yearly thereafter.
Statistical Analysis
The Student’s t test or Mann–Whitney U test was used to compare the mean values and χ 2 or Fisher exact tests were used to compare the frequency distributions of the two groups. The Kaplan–Meier method with log-rank test was used to calculate and compare disease-free survival (DFS) and overall survival (OS) outcomes between the two groups. The time from the date of surgery to the date of recurrence of tumor or censoring was defined as DFS, and the time from the date of surgery to the date of patient death, last follow-up, or censoring was defined as OS. Multivariate analysis was performed using the Cox proportional hazards model with variables showing statistical significance in univariate analysis. P values <0.05 in two-sided tests were considered statistically significant. SPSS software (version 21.0; IBM, Armonk, NY) was used to perform statistical analysis.
Results
In total, 293 eligible patients with adenocarcinoma of the uterine cervix of FIGO stage IA2-IIA underwent ORH or LRH and were followed up at Asan Medical Center during the study period; 186 and 107 patients underwent LRH and ORH, respectively. The clinicopathologic characteristics of the patients are listed in Table 1. There was no difference between the two groups in terms of age, body mass index, parity, history of medical disease, previous abdominal surgery, FIGO stage, histologic subtype, grade of tumor, size of tumor, depth of cervical stromal invasion, lymphovascular space invasion, parametrial invasion, and lymph node metastasis. The most common histologic subtype and FIGO stage was mucinous type and stage IB1.
After surgery, 18, 24, and 65 patients received adjuvant chemotherapy, RT, and CCRT, respectively. There was no difference in the type of adjuvant therapy between the two groups. In 18 patients who received adjuvant chemotherapy, the regimens were taxane/platinum in 13 patients and 5-fluorouracil/platinum in 5 patients. In 66 patients who received adjuvant CCRT, the chemotherapeutic regimen was cisplatin in 51 patients and taxane/platinum in 15 patients.
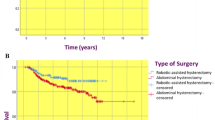
The overall median follow-up time was 58.8 (range, 4.2–189.4) months. The median follow-up times were 47.2 months and 70.6 months for the LRH and ORH groups, respectively (P < 0.001). There were 21 (11.3 %) and 17 (15.9 %) recurrences (P = 0.281) and 13 (7.0 %) and 14 (13.1 %) deaths (P = 0.095) in the LRH and ORH groups, respectively. The 5-year DFS was 89.2 and 86.9 % for the LRH and ORH groups, respectively (P = 0.848), and the 10-year DFS was 88.7 and 85.0 % for the LRH and ORH groups, respectively (P = 0.782; Fig. 1). The 5-year OS was 94.6 and 92.5 % for the LRH and ORH groups, respectively (P = 0.666), and the 10-year OS was 93.0 and 88.8 % for the LRH and ORH groups, respectively (P = 0.849; Fig. 1).
FIGO stage, tumor size, depth of stromal invasion, lymphovascular space invasion, parametrial invasion, lymph node metastasis, and requirement for adjuvant therapy were found to be the prognostic factors for DFS in univariate analysis. Lymph node metastasis was the only independent prognostic factor for DFS found by multivariate analysis (odds ratio [OR], 2.84; 95 % confidence interval [CI], 1.27–6.34; P = 0.011). There was no difference between the LRH and ORH groups in terms of the DFS (OR 1.27; 95 % CI 0.62–2.64; P = 0.514) after adjustment for the prognostic factors significantly associated with this outcome in univariate analysis (FIGO stage, tumor size, depth of stromal invasion, lymphovascular space invasion, parametrial invasion, lymph node metastasis, and requirement for adjuvant therapy; Table 2).
FIGO stage, tumor size, depth of stromal invasion, lymphovascular space invasion, parametrial invasion, lymph node metastasis, and requirement for adjuvant therapy were the indicated prognostic factors for OS by univariate analysis. Lymph node metastasis was the only independent prognostic factor for OS found in the multivariate analysis (OR 2.93; 95 % CI 1.07–8.00; P = 0.036). There was no difference in OS between the LRH and ORH groups (OR 1.43; 95 % CI 0.58–3.49; P = 0.438) after adjustment for the prognostic factors significantly associated with OS (FIGO stage, tumor size, depth of stromal invasion, lymphovascular space invasion, parametrial invasion, lymph node metastasis, and requirement for adjuvant therapy; Table 3).
Table 4 shows the anatomic location of recurrent disease at the time of the first recurrence after surgery. There was no difference in the patterns of recurrence between the two surgery groups (P = 0.220). The median time interval between surgery and the first recurrence were 25 months (range, 3–100 months) for LRH group and 14 months (range, 3–128 months) for ORH group (P = 0.230).
Surgical outcomes are presented in Supplementary Table 1. There were no differences between the two groups in terms of the operating time, preoperative and postoperative hemoglobin levels, changes in the perioperative hemoglobin level, transfusion rate and amount, and number of harvested lymph nodes. The LRH group showed significantly less estimated blood loss (433.1 vs. 627.0 mL, P < 0.001), faster return of bowel movement (2.0 vs. 2.8 days, P < 0.001), and shorter postoperative hospital stay (10.4 vs. 17.5 days, P < 0.001). Intraoperative and postoperative complications and postoperative bladder dysfunction are detailed in Supplementary Table 2. There were 5 (2.7 %) and 0 (0 %) intraoperative complications in the LRH and ORH groups, respectively (P = 0.162). There was one case (0.5 %) of conversion to laparotomy in the LRH group. However, the ORH group showed a significantly higher rate of postoperative complications than the LRH group (34.6 vs. 14.0 %, P < 0.001). The LRH group had a significantly lower rate of wound dehiscence (P = 0.004), ileus (P = 0.001), lymphedema (P = 0.017), infected lymphocele and pelvic abscesses (P = 0.04). There were 49 (26.3 %) and 28 (26.2 %) bladder dysfunctions in the LRH and ORH groups, respectively (P = 1.000).
Discussion
In our study, both LRH and ORH showed excellent long-term survival outcomes in patients with early-stage adenocarcinoma of the uterine cervix. The disease-free and overall survival outcomes were not different between LRH and ORH groups. The pattern of recurrence and the time interval to recurrence were not different between LRH and ORH groups. LRH is an oncologically safe surgical treatment that is comparable to ORH for early-stage adenocarcinoma of the uterine cervix.
Adenocarcinoma of the uterine cervix is a relatively rare type of cervical cancer that comprises approximately 15 % of overall cervical cancer cases and which has recently shown an increasing incidence among the 20–40-year-old age group.4,5,8–10 Most of these cases are diagnosed at an early stage, making them amenable to radical hysterectomy.5,9,25 Radical hysterectomy should be considered in these settings as the primary treatment modality. Although CCRT is a treatment modality that offers similar effects to radical hysterectomy, radical hysterectomy can provide better ovarian and sexual function preservation with fewer long-term complications and has been performed in approximately 80 % of patients.26–28 In addition, a previous study reported DFS and OS rates of 86 and 90 % for radical hysterectomy followed by adjuvant therapy for adenocarcinoma of the cervix with FIGO stage IA2-IIA, which seem to be acceptable and comparable to those of squamous cell carcinoma.29 In the past when the incidence of adenocarcinoma of uterine cervix was relatively low, it was regarded as the same disease entity with squamous cell carcinoma. However, recent advanced researches suggested that its characteristics is somewhat different from those of squamous cell carcinoma in epidemiology, prognostic factors, and patterns of dissemination and recurrence.30 Especially, adenocarcinoma is associated with higher rate of ovarian metastasis and positive peritoneal cytology and higher tendency of peritoneal carcinomatosis and hematogenous metastasis than squamous cell carcinoma.11,14,15 Therefore, the impact of laparoscopic surgery on the survival outcomes and pattern of recurrence should be separately evaluated in the adenocarcinoma alone. Our study is the first that evaluated the role of laparoscopic radical hysterectomy in the surgical management of early-stage adenocarcinoma of uterine cervix. LRH did not affect on the survival outcomes and patterns of recurrence in early-stage adenocarcinoma of the uterine cervix.
In our study, there were no differences between the two treatment groups in terms of operating time, number of harvested lymph nodes, recurrence, death, and survival outcomes. LRH showed significantly better outcomes in terms of estimated blood loss, bowel movement recovery, postoperative hospital stay, and postoperative complications. Additionally, regarding postoperative complications, LRH showed less wound dehiscence, ileus, lymphedema, and lymphocele and pelvic abscesses. An intervention review of the Cochrane collaboration that analyzed previous studies comparing LRH with ORH reported no significant difference in intra- and postoperative complications between the two groups.31 However, in our current analysis LRH was associated with less bleeding and a faster discharge from hospital. Previous studies have revealed that LRH is a viable treatment approach showing better surgical outcomes in cervical cancer patients in terms of less bleeding, earlier recovery of bowel movement, shorter hospital stay, and fewer perioperative complications.23,32 LRH also was reported previously to be a feasible and safe approach in various settings, such as in the obese and elderly and in patients with bulky tumors.32–34 However, there have been few such studies in cases of adenocarcinoma of the cervix, because these patients comprised only a small proportion of the subjects in previous studies of all types of cervical cancer and the results did not reflect the histologic characteristics of this subtype.
In our study, the median follow-up period in the LRH group was 47.2 months compared with 70.6 months in the ORH group. The long follow-up time is one of the strength of our study. The main limitation of our present study was its retrospective design. In addition, there might have been a selection bias in our series. Laparoscopic surgery was chosen after patient consultation and/or according to surgeon preference. However, there were no differences in the overall baseline clinicopathological characteristics between the two surgery groups analyzed.
In conclusion, LRH has comparable survival outcomes with ORH and did not affect the pattern of recurrence in early-stage adenocarcinoma of the uterine cervix. The surgical outcomes were more favorable than ORH.
References
Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Jung KW, Won YJ, Oh CM, et al. Prediction of cancer incidence and mortality in Korea, 2015. Cancer Res Treat. 2015;47:142–8.
Jung KW, Won YJ, Kong HJ, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015;47:127–41.
Kosary CL. FIGO stage, histology, histologic grade, age and race as prognostic factors in determining survival for cancers of the female gynecological system: an analysis of 1973-87 SEER cases of cancers of the endometrium, cervix, ovary, vulva, and vagina. Semin Surg Oncol. 1994;10:31–46.
Vinh-Hung V, Bourgain C, Vlastos G, et al. Prognostic value of histopathology and trends in cervical cancer: a SEER population study. BMC Cancer. 2007;7:164.
Attanoos R, Nahar K, Bigrigg A, et al. Primary adenocarcinoma of the cervix: a clinicopathologic study of prognostic variables in 55 cases. Int J Gynecol Cancer. 1995;5:179–86.
Quinn MA. Adenocarcinoma of the cervix: are there arguments for a different treatment policy? Curr Opin Obstet Gynecol. 1997;9:21–4.
Berek JS, Hacker NF, Fu YS, et al. Adenocarcinoma of the uterine cervix: histologic variables associated with lymph node metastasis and survival. Obstet Gynecol. 1985;65:46–52.
Hopkins MP, Morley GW. A comparison of adenocarcinoma and squamous cell carcinoma of the cervix. Obstet Gynecol. 1991;77:912–7.
Kjorstad KE. Adenocarcinoma of the uterine cervix. Gynecol Oncol. 1977;5:219–23.
Gien LT, Beauchemin MC, Thomas G. Adenocarcinoma: a unique cervical cancer. Gynecol Oncol. 2010;116:140–6.
Zheng T, Holford TR, Ma Z, et al. The continuing increase in adenocarcinoma of the uterine cervix: a birth cohort phenomenon. Int J Epidemiol. 1996;25:252–8.
Vizcaino AP, Moreno V, Bosch FX, et al. International trends in the incidence of cervical cancer: I. Adenocarcinoma and adenosquamous cell carcinomas. Int J Cancer. 1998;75:536–45.
Shimada M, Kigawa J, Nishimura R, et al. Ovarian metastasis in carcinoma of the uterine cervix. Gynecol Oncol. 2006;101:234–7.
Kuji S, Hirashima Y, Komeda S, et al. The relationship between positive peritoneal cytology and the prognosis of patients with FIGO stage I/II uterine cervical cancer. J Gynecol Oncol. 2014;25:90–6.
Fujiwara K, Monk B, Devouassoux-Shisheboran M. Adenocarcinoma of the uterine cervix: why is it different? Curr Oncol Rep. 2014;16:416.
Adegoke O, Kulasingam S, Virnig B. Cervical cancer trends in the United States: a 35-year population-based analysis. J Womens Health (Larchmt). 2012;21:1031–7.
Baalbergen A, Veenstra Y, Stalpers L. Primary surgery versus primary radiotherapy with or without chemotherapy for early adenocarcinoma of the uterine cervix. Cochrane Database Syst Rev. 2013:CD006248.
Pellegrino A, Vizza E, Fruscio R, et al. Total laparoscopic radical hysterectomy and pelvic lymphadenectomy in patients with Ib1 stage cervical cancer: analysis of surgical and oncological outcome. Eur J Surg Oncol. 2009;35:98–103.
Chen Y, Xu H, Li Y, et al. The outcome of laparoscopic radical hysterectomy and lymphadenectomy for cervical cancer: a prospective analysis of 295 patients. Ann Surg Oncol. 2008;15:2847–55.
Abu-Rustum NR, Gemignani ML, Moore K, et al. Total laparoscopic radical hysterectomy with pelvic lymphadenectomy using the argon-beam coagulator: pilot data and comparison to laparotomy. Gynecol Oncol. 2003;91:402–9.
Piver MS, Chung WS. Prognostic significance of cervical lesion size and pelvic node metastases in cervical carcinoma. Obstet Gynecol. 1975;46:507–10.
Nam JH, Park JY, Kim DY, et al. Laparoscopic versus open radical hysterectomy in early-stage cervical cancer: long-term survival outcomes in a matched cohort study. Ann Oncol. 2012;23:903–11.
Sedlis A, Bundy BN, Rotman MZ, et al. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: a gynecologic oncology group study. Gynecol Oncol. 1999;73:177–83.
Chargui R, Damak T, Khomsi F, et al. Prognostic factors and clinicopathologic characteristics of invasive adenocarcinoma of the uterine cervix. Am J Obstet Gynecol. 2006;194:43–8.
Landoni F, Maneo A, Colombo A, et al. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet. 1997;350:535–40.
Trimble EL, Harlan LC, Gius D, et al. Patterns of care for women with cervical cancer in the United States. Cancer. 2008;113:743–9.
Kato T, Watari H, Takeda M, et al. Multivariate prognostic analysis of adenocarcinoma of the uterine cervix treated with radical hysterectomy and systematic lymphadenectomy. J Gynecol Oncol. 2013;24:222–8.
Park JY, Kim DY, Kim JH, et al. Outcomes after radical hysterectomy in patients with early-stage adenocarcinoma of uterine cervix. Br J Cancer. 2010;102:1692–8.
Fujiwara H, Yokota H, Monk B, et al. Gynecologic Cancer InterGroup (GCIG) consensus review for cervical adenocarcinoma. Int J Gynecol Cancer. 2014;24:S96–101.
Kucukmetin A, Biliatis I, Naik R, et al. Laparoscopically assisted radical vaginal hysterectomy versus radical abdominal hysterectomy for the treatment of early cervical cancer. Cochrane Database Syst Rev. 2013;10:CD006651.
Park JY, Kim DY, Kim JH, et al. Laparoscopic versus open radical hysterectomy in patients with stage IB2 and IIA2 cervical cancer. J Surg Oncol. 2013;108:63–9.
Park JY, Kim DY, Kim JH, et al. Laparoscopic compared with open radical hysterectomy in obese women with early-stage cervical cancer. Obstet Gynecol. 2012;119:1201–9.
Park JY, Kim DY, Kim JH, et al. Laparoscopic versus open radical hysterectomy for elderly patients with early-stage cervical cancer. Am J Obstet Gynecol. 2012;207:195 e1–8.
Disclosure
The authors declare that there are no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Park, JY., Kim, D., Suh, DS. et al. The Role of Laparoscopic Radical Hysterectomy in Early-Stage Adenocarcinoma of the Uterine Cervix. Ann Surg Oncol 23 (Suppl 5), 825–833 (2016). https://doi.org/10.1245/s10434-016-5489-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5489-4