Abstract
Objective
The aim of this study was to analyze clinical and laboratory variables associated with complications after gastrectomy for gastric cancer to predict candidates for successful early discharge.
Methods
Consecutive patients undergoing gastrectomy at Seoul National University Hospital from January through December 2013 were identified from a prospective complications database. Clinicopathologic and postoperative laboratory parameters were analyzed to determine variables associated with complications. An additional validation study was performed from March through May 2014.
Results
Overall, complications occurred in 180/855 patients (21.1 %). Age >68 years (odds ratio [OR] 1.64), use of an open approach (OR 1.9), and use of combined resection (OR 1.67) were significant independent risk factors for complications (p < 0.05). The postoperative day (POD) 5 to preoperative white blood cell count (WBC) ratio (risk ratio [RR] 2.01), C-reactive protein (CRP) level on POD 5 (RR 1.1), and maximum body temperature on POD 4 (RR 2.36) independently predicted complications in a multivariate analysis (p < 0.05). After establishing an early discharge profile (EDP) based on these six variables, 152/855 patients (17.8 %) were predicted to have an uncomplicated course. Of these, 8/152 (5.3 %) experienced complications. In a validation study of 217 patients, 43/217 (19.8 %) were candidates for early discharge on POD 5, and 3 (7.0 %) had a false-positive EDP.
Conclusions
Patients younger than 68 years of age who underwent laparoscopic gastrectomy without combined resection might be candidates for early discharge on POD 5 if the POD 5 to preoperative WBC ratio is ≤1.2, POD 5 CRP level is ≤5.38 g/mL, and POD 4 body temperature is ≤37.4 °C.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Post-gastrectomy complications in patients with gastric cancer can be associated with increased morbidity, often resulting in long hospital stays, disturbances of oral nutrition, increased socioeconomic costs, and even poor long-term oncologic outcomes.1 , 2 Despite significant efforts to control complications, the rate of morbidity following gastrectomy is reported to be 10–28 %. 3 – 7
To date, many clinical studies related to the risk of complications after gastrectomy have focused on the detection of risk factors. Age, extent of gastrectomy, combined resection, comorbidities, the surgeon’s experience, and extent of lymphadenectomy have been reported as predictive factors.4 , 7 – 9 In terms of laboratory parameters, white blood cell count (WBC) and C-reactive protein (CRP) level are widely used markers for predicting infectious complications in various surgical fields.10 – 13 Although many studies have examined risk factors for complications, few reports have specifically focused on the factors predicting an uncomplicated hospital stay.
With increasing medical costs, safely reducing the length of a patient’s hospital stay has become a major focus for optimizing the utilization of healthcare resources.14 Determining which factors influence the length of hospital stay might provide information on how to reduce costs and improve treatment delivery.15 Enhanced recovery pathways have standardized perioperative care, facilitated ‘fast-track’ recovery, and been proven to reduce length of hospital stay after gastrectomy.16 , 17 For successful fast-track recovery, identifying patients with complications is indispensable before discharge. Thus, in this study, we investigated clinical and laboratory data for patients following gastrectomy to identify those patients who might be candidates for successful, uncomplicated early discharge.
Patients and Methods
Patients
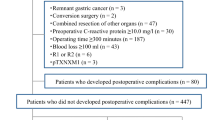
We retrospectively collected data from 855 patients who underwent gastric cancer surgery at Seoul National University Hospital between January and December 2013 who satisfied our inclusion criteria of having a primary gastric cancer diagnosis and who underwent gastrectomy. Patients who underwent preoperative chemotherapy and/or had other primary malignancies, recurrent cancer, or remnant gastric cancers were excluded.
Data on patient demographics, operative procedures, pathological results based on the American Joint Committee on Cancer (AJCC) TNM 7th edition,18 hospital course, laboratory results, and postoperative complications were reviewed. Data on complications were collected prospectively. The hospital course was monitored daily by the attending surgeon. In addition, based on a consensus of faculty at a weekly conference, the type and classification of each complication was defined using the Clavien–Dindo classification.19 Complications that occurred within 30 days postoperatively were considered relevant to the operation and were collected for this study. The data included that of patients who were discharged and then revisited the emergency room or outpatient clinic because of complications. Data for complications resulting in readmission and/or occurring outside of the hospital course were also collected; complications were defined based on our previous report on complications following gastrectomy.4 Comorbidity data were collected and scored according to the Charlson Comorbidity Index.20
The independent risk factors for overall postoperative complications were used to determine constituent units of an early discharge profile (EDP). Patients who satisfied the criteria of the EDP were defined as positive for EDP; however, patients who did satisfy all of the criteria were considered negative for EDP. A false-positive EDP was defined as a patient who was predicted to have an uncomplicated course but who experienced any postoperative complication.
Additional internal validation for the application of this profile was performed from March to May 2014 using data from 217 patients based on the same inclusion and exclusion criteria used in this study.
Patients underwent subtotal (including distal, pylorus-preserving, or proximal) or total gastrectomy with regional lymphadenectomy as defined by the Japanese Gastric Cancer Association treatment guidelines.21 Briefly, laparoscopic gastrectomy with D1+ lymph node dissection was performed for patients preoperatively diagnosed with clinically early gastric cancer (EGC), while open gastrectomy with D2 lymphadenectomy was performed for patients with advanced gastric cancer (AGC). Patients enrolled in the KLASS-02 trial (NCT01456598), a prospective, multicenter, randomized controlled trial comparing laparoscopic and open distal gastrectomy with D2 lymphadenectomy for AGC, underwent laparoscopic distal gastrectomy, even if they were diagnosed with AGC preoperatively.22 According to the surgeon’s preference, either total or proximal gastrectomy was performed for EGC in the upper third of the stomach, and pylorus-preserving or distal gastrectomy was performed for EGC in the middle third of the stomach. All surgical procedures were performed by four experienced faculty surgeons.
Patients were managed perioperatively using the same standardized clinical pathway protocol.23 Prophylactic antibiotics were administered immediately before skin incision and continued until the first postoperative day (POD 1). Following surgery, sips of water were allowed for patients on POD 3, irrespective of whether flatus could be passed. Serum laboratory tests, including complete blood count, electrolytes, admission panel (i.e. calcium, phosphorus, glucose, blood urea nitrogen [BUN], uric acid, cholesterol, protein, albumin, total bilirubin, alkaline phosphatase, aspartate aminotransferase, alanine aminotransferase, and creatinine) and CRP level, were measured on PODs 2, 5, and 7. If water was ingested successfully, patients were allowed a semi-fluid diet on POD 4. In the absence of complications or complaints, patients were discharged on the seventh or eighth POD after removal of stitches.
Statistical Analysis
Categorical variables were presented as numbers and percentages, and postoperative complications were compared among groups using the Chi square test. Continuous variables were expressed as the means and standard deviations, and the means were compared using the Student’s t test. A univariate analysis was conducted to evaluate the independent association of each factor with the development of postoperative complications. Independent risk factors for postoperative complications were then adjusted in a multivariate logistic regression. During that analysis, variables found to be significant in the univariate analysis were entered into a multivariate analysis. In the multivariate analysis, adjusted odds ratios (ORs) [exponential β] were calculated with 95 % confidence intervals (CIs). Multicollinearity between independent variables (i.e. laboratory data) was assessed by variance inflation factors (VIF) [reference value of 5] before calculating the final output. We configured the EDP using independent risk factors for complications confirmed by multivariate analysis. A receiver operating characteristic (ROC) curve analysis was conducted to evaluate predictors of complications by age, CRP level, WBC count, and maximal body temperature on POD 4. Optimal cut-off values were determined by the maximum value of Youden’s index (sensitivity + specificity−1). All tests were two-sided and were performed at a significance level of 5 % using IBM® SPSS® Statistics version 20 software (IBM Corporation, Armonk, NY, USA). This study was approved by the Institutional Review Board of our institution (H-1305-043-488).
Results
Patient Characteristics
A total of 855 patients were included in the study, and their clinicopathological characteristics are shown in Table 1. Overall, 180 patients (21.1 %) developed complications, accounting for 245 clinical events; 71 patients (8.3 %) experienced severe complications (grade IIIa or higher). Detailed descriptions of local and systemic complications are presented in electronic supplementary Table S1 .
Clinical and Laboratory Outcomes Associated with Postoperative Complications
In the univariate analysis, higher complication rates were associated with older age, male sex, type of gastrectomy (e.g. total and proximal gastrectomy), the open surgical method, extent of lymphadenectomy (e.g. D2), combined resection, and higher maximal body temperature on POD 4 (POD 4 BTmax; all p < 0.05) [Table 2]. In the analysis of laboratory data, POD 2 WBC count, POD 2 CRP level, POD 2 albumin level, POD 5 WBC count, POD 5 CRP level, POD 5 BUN level, and POD 5 albumin level were significantly different between patients with and without complications (all p < 0.05) [Table 2]. In addition, the ratios of the WBC count (including the POD 2:preoperative, POD 5:preoperative, and POD 5:POD 2 ratios) and the POD 5:POD 2 CRP ratio were significantly different between patients with and without postoperative complications.
In the multivariate analysis, age >68 years (OR 1.64, 95 % CI 1.12–2.40), the open approach (OR 1.9, 95 % CI 1.29–2.8), and combined resection (OR 1.67, 95 % CI 1.06–2.62) were found to be significant independent predictors for overall complications (p < 0.05). The POD 5:preoperative WBC ratio (risk ratio [RR] 2.01, 95 % CI 1.18–3.43), POD 5 CRP level (RR 1.1, 95 % CI 1.05–1.15), and POD 4 BTmax (RR 2.396, 95 % CI 1.43–3.9) were found to be independent predictors in the multivariate analysis (all p < 0.05) [Table 3].
Establishment of an Early Discharge Profile
Using the results of the ROC curve analysis, the cut-off values for each significant continuous variable were (i) age 68.5 years; (ii) POD 5 CRP level 5.38 g/mL; (iii) POD 5:preoperative WBC ratio 1.2; and (iv) POD 4 BTmax 37.45 (Electronic Supplementary Fig. S1). With the addition of two categorical variables (laparoscopic approach and the absence of combined organ resection), a total of six values comprised the EDP (Electronic Supplementary Table S2).
Based on the EDP we developed, of the 855 total patients, the number of patients predicted to have an uncomplicated course was 152 (17.8 %). Among these 152 patients, 144 (94.7 %) did not experience any complication and 8 patients (8/152, 5.3 %) did. These 8 patients were considered to have a false-positive EDP (Table 4). In the internal validation study for the EDP, 43/217 patients (approximately one-fifth, 19.8 %) were predicted to have an uncomplicated recovery. Among these 43 patients who met the requirements for the EDP, 3 had a false-positive EDP (false-positive rate 7 %, 3/43) [Table 5].
Complications Associated with a False-Positive Early Discharge Profile
Among 152 patients predicted to have uncomplicated recoveries, 8 (5.3 %) developed a total of nine complications, including three grade I complications (two wound complications and one urinary complication), three grade II complications (one motility disorder, one aggravation of previous ulcerative colitis, and one pancreatic leakage), two grade IIIa complications (two anastomotic stenoses), and one grade IIIb complication (one adhesive ileus). For the patient with the grade IIIb complication, laparoscopy-assisted total gastrectomy with Roux-en-Y esophagojejunostomy was performed with adhesiolysis and duodenojejunostomy on POD 29 for adhesive ileus. Two patients with grade IIIa complications successfully recovered after balloon dilation for anastomotic stenosis. The remaining patients with false-positive EDP complications were managed with conservative treatment. Of the three patients with false-positive EDPs in the validation analysis, all three had grade IIIa complications (two with wound dehiscence and one anastomotic stenosis). All of these patients recovered after wound repair under local anesthesia and temporary stent insertion throughout the stenotic anastomosis.
Discussion
In the current study, we developed and internally validated an EDP for predicting which patients would experience uncomplicated recoveries after gastrectomy in order to identify candidates for early discharge. The EDP integrated four clinical variables (age, surgical approach, combined organ resection, and POD 4 BTmax) and two laboratory values (POD 5 CRP and POD 5:preoperative WBC ratio) associated with postoperative complications.
In our study, age >68 years, the open surgical method, and combined organ resection independently predicted the occurrence of complications. In addition to these factors, we discovered that POD 4 BTmax was significantly associated with complications. In terms of the relationship between laboratory values and complications, Dutta et al. showed that CRP values on PODs 3 and 4 were clinically useful for predicting surgical infectious complications after resection for esophagogastric cancer.11 A previous report from our institution determined that pre-albumin, a visceral protein that is sensitive to protein malnutrition, is a useful marker for predicting infectious complications after gastric surgery.24 In another study, we revealed a relationship between hemoglobin level and complications, suggesting that both anemia and transfusion are important factors in the development of complications.25 In the present study, we analyzed the influence of several laboratory values on the occurrence of post-gastrectomy complications. POD 2 WBC, POD 5 CRP level, and the POD 5:preoperative WBC ratio were significantly related to the development of complications. The concept of the WBC ratio as a laboratory value was introduced in this analysis in order to compensate for baseline differences among patients. In fact, two WBC values (POD 2 WBC and the POD 5:preoperative WBC ratio) were found to be significant predictors. However, POD 2 WBC count was excluded from our EDP because it had a lower relative risk than the POD 5:preoperative WBC ratio (1.06 vs. 2.01, respectively).
Overall, 78.9 % (675/855) of patients had an uncomplicated course, while only 17.8 % of patients were predicted to have an uncomplicated course, which might seem to indicate that the discriminatory power of the EDP is low. However, we created this EDP with a focus on the detection of candidates for safe early discharge on POD 5 without any complications. Based on this profile, approximately one-fifth of patients could be discharged earlier than they would be based on the routine clinical pathway’s discharge on POD 7 used in our institution.
Given the complications associated with patients with false-positive EDPs in this study, the developed EDP may not appropriately account for anastomotic stenoses, wound problems, or gastrointestinal motility disorders. Among a total of 12 patients with false-negative risk profiles, three-quarters (9/12) had complications that were classified as one of these types of complications. Among all occurring complications, the EDP was least able to predict anastomotic stenosis (3/19 [15.8 %] compared with wound problems, 3/19 [15.8 %], and gastrointestinal motility disorder, 2/30 [6.7 %]). Monitoring clinical signs and laboratory values is the cornerstone of routine postoperative care, whereas WBC count and CRP level are the most widely used markers of infectious complications, such as anastomotic leakage, fluid collection, and pneumonia. However, anastomotic stenosis, wound problems, and ileus are not accompanied by inflammatory processes in the initial stage.
Recently, the application of minimally invasive surgery has increased, and gastrectomy could be considered a field in which fast-track surgery could be adopted.16 , 17 To accomplish successful fast-track surgery, the selection of patients who will have an uncomplicated postoperative course is essential. In this study, we were able to predict patients who did not experience complications and who could have been successfully discharged early after gastrectomy using clinical data through POD 4 and laboratory values on POD 5. In other words, application of this profile for predicting uncomplicated patients could also be useful for expanding fast-track surgery in gastric cancer surgery. The profile proposed in this study might be a useful means of establishing a reasonable discharge recommendation.
This study had several limitations. First, we did not consider the timing of complication development; however, postoperative complications were detected before POD 5 in 103/855 patients (12.1 %). Our EDP did not consider the development of early complications. Second, the predictive value for early discharge (<20 %) appears low. Finally, in our gastric cancer cohorts, two-thirds of patients were diagnosed in the early stage, which is different from the profile described in Western studies.
Conclusions
We established and validated an EDP for predicting an uncomplicated hospital course after gastrectomy for gastric cancer. Patients younger than 68 years of age who underwent laparoscopic gastrectomy without combined resection might be candidates for early discharge at POD 5 if the POD 5:preoperative WBC ratio is ≤1.2, POD 5 CRP level is ≤5.38, and POD 4 BTmax is ≤37.4 °C.
References
Sierzega M, Kolodziejczyk P, Kulig J. Impact of anastomotic leakage on long‐term survival after total gastrectomy for carcinoma of the stomach. Br J Surg. 2010;97:1035-42.
Yoo HM, Lee HH, Shim JH, Jeon HM, Park CH, Song KY. Negative impact of leakage on survival of patients undergoing curative resection for advanced gastric cancer. J Surg Oncol. 2011;104:734-40.
Sasako M, Sano T, Yamamoto S, et al. D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med. 2008;359:453-62.
Lee KG, Lee HJ, Yang JY, et al. Risk factors associated with complication following gastrectomy for gastric cancer: retrospective analysis of prospectively collected data based on the Clavien–Dindo system. J Gastroint Surg. 2014;18:1269-77.
Kim HH, Hyung WJ, Cho GS, et al. Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report—a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg. 2010;251:417-20.
Degiuli M, Sasako M, Ponti A. Morbidity and mortality in the Italian gastric cancer study group randomized clinical trial of D1 versus D2 resection for gastric cancer. Br J Surg. 2010;97:643-9.
Park DJ, Lee HJ, Kim HH, Yang HK, Lee KW, Choe KJ. Predictors of operative morbidity and mortality in gastric cancer surgery. Br J Surg. 2005;92:1099-102.
Kim MC, Kim W, Kim HH, et al. Risk factors associated with complication following laparoscopy-assisted gastrectomy for gastric cancer: a large-scale Korean multicenter study. Ann Surg Oncol. 2008;15:2692-700.
Persiani R, Antonacci V, Biondi A, et al. Determinants of surgical morbidity in gastric cancer treatment. J Am Coll Surg. 2008;207:13-9.
Platt JJ, Ramanathan ML, Crosbie RA, et al. C-reactive protein as a predictor of postoperative infective complications after curative resection in patients with colorectal cancer. Ann Surg Oncol. 2012;19:4168-77.
Dutta S, Fullarton GM, Forshaw MJ, Horgan PG, McMillan DC. Persistent elevation of C-reactive protein following esophagogastric cancer resection as a predictor of postoperative surgical site infectious complications. World J Surg. 2011;35:1017-25.
Welsch T, Frommhold K, Hinz U, et al. Persisting elevation of C-reactive protein after pancreatic resections can indicate developing inflammatory complications. Surgery. 2008;143:20-8.
Garcia-Granero A, Frasson M, Flor-Lorente B, et al. Procalcitonin and C-reactive protein as early predictors of anastomotic leak in colorectal surgery: a prospective observational study. Dis Colon Rectum. 2013;56:475-83.
Kiran RP, Delaney CP, Senagore AJ, Steel M, Garafalo T, Fazio VW. Outcomes and prediction of hospital readmission after intestinal surgery. J Am Coll Surg. 2004;198:877-83.
Collins TC, Daley J, Henderson WH, Khuri SF. Risk factors for prolonged length of stay after major elective surgery. Ann Surg. 1999;230:251-9.
Kim JW, Kim WS, Cheong JH, Hyung WJ, Choi SH, Noh SH. Safety and efficacy of fast-track surgery in laparoscopic distal gastrectomy for gastric cancer: a randomized clinical trial. World J Surg. 2012;36:2879-87.
Yu Z, Zhuang CL, Ye XZ, Zhang CJ, Dong QT, Chen BC. Fast-track surgery in gastrectomy for gastric cancer: a systematic review and meta-analysis. Langenbecks Arch Surg. 2014;399:85-92.
Washington K. 7th edition of the AJCC cancer staging manual: stomach. Ann Surg Oncol. 2010;17:3077-9.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-13.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-83.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011;14:113-23.
Kim HI, Hur H, Kim YN, et al. Standardization of D2 lymphadenectomy and surgical quality control (KLASS-02-QC): a prospective, observational, multicenter study [NCT01283893]. BMC Cancer. 2014;14:209.
Jeong SH, Yoo MW, Yoon HM, et al. Is the critical pathway effective for the treatment of gastric cancer? J Kor Surg Soc. 2011;81:96-103.
Bae HJ, Lee HJ, Han DS, et al. Prealbumin levels as a useful marker for predicting infectious complications after gastric surgery. J Gastroint Surg. 2011;15:2136-44.
Jung DH, Lee HJ, Han DS, et al. Impact of perioperative hemoglobin levels on postoperative outcomes in gastric cancer surgery. Gastric Cancer. 2013;16:377-82.
Funding
This study was supported by a grant from the National R & D Program for Cancer Control, Ministry of Health & Welfare, Republic of Korea (1320270).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Ji-Ho Park, Young-Gil Son, Tae-Han Kim, Yeon-Ju Huh, Jun-Young Yang, Yong-Joon Suh, Yun-Suhk Suh, Seong-Ho Kong, Hyuk-Joon Lee, and Han-Kwang Yang declare no potential conflicts of interest.
Additional information
Ji-Ho Park and Young-Gil Son have contributed equally to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Park, JH., Son, YG., Kim, TH. et al. Identification of Candidates for Early Discharge After Gastrectomy. Ann Surg Oncol 24, 159–166 (2017). https://doi.org/10.1245/s10434-016-5447-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5447-1