Abstract
Introduction
Triple-negative breast cancer (TNBC) is more common among African American (AA) and western sub-Saharan African breast cancer (BC) patients compared with White/Caucasian Americans (WA) and Europeans. Little is known about TNBC in east Africa.
Methods
Invasive BC diagnosed 1998–2014 were evaluated: WA and AA patients from the Henry Ford Health System in Detroit, Michigan; Ghanaian/west Africans from the Komfo Anokye Teaching Hospital in Kumasi, Ghana; and Ethiopian/east Africans from the St. Paul’s Hospital Millennium Medical College in Addis Ababa, Ethiopia. Histopathology and immunohistochemistry for estrogen receptor (ER), progesterone receptor (PR), and HER2/neu expression was performed in Michigan on formalin-fixed, paraffin-embedded samples from all cases.
Results
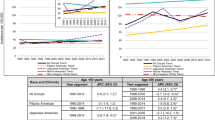
A total of 234 Ghanaian (mean age 49 years), 94 Ethiopian (mean age 43 years), 272 AA (mean age 60 years), and 321 WA (mean age 62 years; p = 0.001) patients were compared. ER-negative and TNBC were more common among Ghanaian and AA compared with WA and Ethiopian cases (frequency ER-negativity 71.1 and 37.1 % vs. 19.8 and 28.6 % respectively, p < 0.0001; frequency TNBC 53.2 and 29.8 % vs. 15.5 and 15.0 %, respectively, p < 0.0001). Among patients younger than 50 years, prevalence of TNBC remained highest among Ghanaians (50.8 %) and AA (34.3 %) compared with WA and Ethiopians (approximately 16 % in each; p = 0.0002).
Conclusions
This study confirms an association between TNBC and West African ancestry; TNBC frequency among AA patients is intermediate between WA and Ghanaian/West Africans consistent with genetic admixture following the west Africa-based trans-Atlantic slave trade. TNBC frequency was low among Ethiopians/East Africans; this may reflect less shared ancestry between AA and Ethiopians.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
African American (AA) women bear a disproportionately high share of the breast cancer mortality burden in the United States, and this outcome disparity has been increasing. Socioeconomic disadvantages that are more prevalent in the AA community, such as poverty rates and being underinsured, undeniably contribute to barriers in accessing the health care system and result in poorer cancer control overall.
However, there are features characterizing the epidemiology of breast cancer in AAs that cannot be easily ascribed to socioeconomic inequities. Until recently, population-based lifetime incidence rates of breast cancer have been lower for AA compared with White/Caucasian American (WA) women; the average age at breast cancer diagnosis is younger for AA patients; and AA women have higher rates of hormone receptor-negative and the biologically more-virulent triple-negative tumors. Last, population-based incidence rates of male breast cancer are higher in the AA community.
We sought to evaluate the question of whether African ancestry is associated with some heritable marker of risk for particular patterns of breast cancer pathogenesis by studying breast tumor phenotypes in four different population subsets: WAs; AAs; Ghanaians (representing west Africa); and Ethiopians (representing east Africa).
Methods
Ethics
This research effort represents clinicopathology studies that are components of an international breast cancer registry, approved by the Institutional Review Boards of the University of Michigan; the Henry Ford Health System; and the human research ethics approval and/or institutional departmental approval equivalents for the Komfo Anoyke Teaching Hospital in Kumasi Ghana (Committee on Human Research Publication and Ethics, Kwame Nkrumah University of Science and Technology) and the St. Paul’s Hospital Millennium Medical College in Addis Ababa, Ethiopia. Samples and results were de-identified/anonymized prior to analyses.
Pathology and Immunohistochemistry
Histopathology to confirm the diagnosis of breast cancer and immunohistochemistry for molecular marker studies were performed on the specimens from AA and WA cases by the Department of Pathology at the Henry Ford Health System. Evaluation of the Ghanaian and Ethiopian tumor specimens were performed at the University of Michigan North Campus Research Complex. Nuclear expression of hormone receptor (ER and PR) proteins was detected with specific monoclonal antibodies using a labeled streptavidin–biotin immunoperoxidase method. The immunohistochemical assay was performed on deparaffinized, formalin-fixed tissue sections of the specimens. Monoclonal mouse antibodies to human ER (DAKO clone ID5) and to human PR (DAKO clone PgR636) were used with a DAKO automated immunostainer following the manufacturer’s protocol. Immunohistochemistry for HER2/neu staining was performed using the HerceptTest (DAKO, Glostrup, Denmark), an FDA-approved clinical test that qualitatively identifies by light microscopy p185 HER2 overexpression in breast cancer cells. Molecular marker staining was interpreted in compliance with ASCO/CAP guidelines and as per Fitzgibbons et al.1 – 3 Tumors were scored as ER/PR-negative if they had less than 1 % nuclear staining. Confirmed ER- and PR-positive tumors served as positive controls, and normal adjacent mammary gland ductules present in the sections of tumor served as internal positive controls for the hormone receptors. The expression of HER2 was scored based on recommendations from Fitzgibbons et al.1 Grading was based on the degree and intensity of membrane labeling of tumor cells, on a scale from 0–3+ , as follows: grade 0 (no observable labeling or faint, incomplete, or barely detectable membrane labeling in <10 % of tumor cells), 1+ (faint, incomplete, or barely detectable membrane labeling in >10 % of tumor cells), 2+ (incomplete and/or weak to moderate complete membrane staining in >10 % of tumor cells, or complete, intense membrane labeling in <10 % of tumor cells), or 3+ (intense, complete membrane labeling in >10 % of tumor cells). A specimen scored as 0 or 1+ was classified as HER2/neu negative, and specimens scored as 3+ were considered positive. Those specimens with a score of 2+ were considered equivocal, and follow-up fluorescent in situ hybridization (FISH) was used to assess amplification of the HER2/neu gene in these cases. Tumors that were negative for ER, PR and HER2/neu were classified as triple-negative breast cancer (TNBC).
Ascertainment of Cases
AA and WA: At Henry Ford Health System, women diagnosed with their first primary invasive breast cancer between January 1, 2001 and December 31, 2006 were identified from the Pathology Information System (Co-Path). The initial date of entry reflects the year that HFHS implemented an institutional wide policy mandating routine assessment of the HER2 biomarker for all cases of invasive breast cancer. The other eligibility criteria were: (1) the initial diagnosis of breast cancer at HFHS; (2) AJCC TNM stages I–IV; and (3) insurance through the HMO plan. The first two eligibility requirements were imposed to minimize variation in the standards of the pathologic diagnostic criteria. The last criterion was imposed to reduce the potential confounding effect of socioeconomic status, i.e., limited or no access to healthcare, on the pathologic prognostic indicators of breast cancer. Data on date of birth/age at diagnosis, and racial-ethnic identity were collected from electronic medical records.
Ghanaian: Samples were obtained through the archived resources of the Department of Pathology at the Komfo Anokye Teaching Hospital in Kumasi, Ghana. They reflected a convenience-based collection of invasive breast cancer specimens in women diagnosed 1998–2014. Patient age at diagnosis and gender was the only uniformly available clinical feature on these cases, as provided by the Department of Pathology records.
Ethiopian: Samples were obtained through the archived resources of the Department of Pathology at the St. Paul’s Hospital Millennium Medical College in Addis Ababa, Ethiopia. They reflected a convenience-based collection of invasive breast cancer specimens in women diagnosed 2001–2014. Patient age at diagnosis and gender was the only uniformly available clinical feature on these cases, as provided by the Department of Pathology records.
Statistical Analysis
Parametric and nonparametric statistical techniques, as appropriate, were performed to discern the distribution of clinicopathologic variables between African-Americans and white-Americans populations. We then dichotomized women into two age groups, <50 years versus ≥50 years, and conducted a sub-set analysis to discern the distribution of clinicopathologic variables between African-American and White-American women younger than age 50 years.
All statistical tests were two-sided, and p values of p ≤ 0.05 were considered statistically significant. Analyses were performed using SAS vs. 9.1 (SAS Institute, Cary, NC).
Results
Tables 1 and 2 demonstrate the clinicopathologic features for the 272 AA compared with 321 WA patients from the Henry Ford Health System, revealing statistically significant higher frequencies of high-grade, estrogen receptor-negative and TNBC among the AA cases; frequency of HER2/neu-overexpressing tumors was similar between these two groups. The AA patients had a numerically but statistically nonsignificant younger mean age at diagnosis compared with the WA patients (60 vs. 62; p = 0.09). The AA patients had a similar stage distribution compared with the WA patients overall and in the subset analysis of patients younger than age 50 years.
As shown in Table 3, both American population subsets had older mean ages at diagnosis compared with the 234 Ghanaian patients (mean age 49 years) and the 94 Ethiopian patients (mean age 43 years; p < 0.001). High-grade pathology was significantly more common among the tumors of the AA, Ghanaian, and Ethiopian patients compared with those of the WA patients (50.4, 53.8, and 53.6 % compared with 33.7 %, respectively; p < 0.001).
Figure 1a demonstrates results of the molecular marker and phenotype comparisons. Frequency of ER-negative and TNBC was highest in the Ghanaians (71.1 and 53.2 % respectively), lower in the WAs (19.8 and 15.5 %, respectively), and intermediate in the AAs (37.1 and 29.8 %, respectively). Frequency of TNBC in the Ethiopian cases was similar to the WA cases (15.0 and 15.5 %, respectively). Differences in the distribution of these phenotypes across all four population subsets were statistically significant (p < 0.0001 for ER; p < 0.0001 for TNBC). Frequency of HER2/neu-overexpressing tumors was low in the WA, AA, and Ghanaian cases (16.7, 18.7, and 19.6 %, respectively) but significantly higher in the Ethiopian cases (33.3 %; p = 0.0048).
Figure 1b presents subset analysis for the patients younger than age 50 years, revealing patterns similar to those seen for patients of all ages. Frequency of TNBC was highest in the Ghanaians (50.8 %), lowest in WA and Ethiopians (nearly 16 % in each), and intermediate in AA patients (34.3 %; p < 0.0001). Among patients younger than age 50 years, the frequency of HER2/neu-overexpressing cancers was similar for all four subsets.
Table 4 demonstrates phenotype distributions for the four different patient populations as couplet comparisons, revealing that the Ethiopians and WAs were the most similar across all four phenotypes (p = 0.06). Statistically significant differences were observed in comparisons of all other couplets, largely driven by the highest frequencies of TNBC in the Ghanaian patients and moderately high frequencies in the AAs.
Discussion
A meta-analysis from 10 years ago evaluated survival rates of more than 13,000 AA and 75,000 WA breast cancer patients and found that AA identity was associated with a statistically significant outcome disadvantage, even after adjusting for socioeconomic status (mortality hazard 1.28; 95 % confidence interval 1.18–1.38).4 The importance of tumor biology in the complex disparities picture was highlighted in the 2015 Annual Report to the Nation on the Status of Cancer, demonstrating that population-based incidence rates of TNBC are approximately twofold higher for AAs compared with all other population subsets, a pattern seen in all age categories.5 Population-based incidence rates of male breast cancer also are higher for AAs compared with WAs, and the California Cancer Registry found a threefold higher frequency of TNBC among AA compared with WA men with breast cancer.6
The American Cancer Society and the Surveillance Epidemiology and End Results (SEER) Program reported recently that breast cancer incidence rates have been increasing for AA women and now are equal to the incidence rates in WA women.7 Many of the advances made in systemic therapy for breast cancer have been in targeted therapies for endocrine-sensitive and HER2/neu-overexpressing tumors. Because the frequency of TNBC is higher in AA breast cancer patients, these treatment advances are less effective in this population subset. The disproportionate effectiveness of targeted therapies in AA breast cancer patients, coupled with the increasing incidence of breast cancer in AA has resulted a widening of the mortality disparity between AAs and WAs, which is now a 42 % difference.
Against this background landscape of worsening breast cancer survival disparities related to racial-ethnic identity, our study evaluated the association between African ancestry and TNBC by studying four different patient populations: AAs; WAs; Ghanaians (representing west Africa) and Ethiopians (representing east Africa). The two populations of African patients were significantly younger than the American patients, but this pattern is likely heavily influenced by the shorter overall life expectancy of individuals born in low- and middle-income countries. We also found highest frequencies of ER-negative and TNBC in AA and west African/Ghanaian breast cancer patients. WAs and Ethiopians had similarly low frequencies for these phenotypes. Interestingly, frequency of HER2/neu-overexpressing tumors was elevated among Ethiopian breast cancer patients compared to the three other population subsets. These patterns persisted in subset analyses looking at patients younger than age 50 years.
Our study suggests that breast cancer patterns of AAs are similar to those of west Africans but differ from those of east Africans. Patterns of the Africa diaspora and forced population migration through the slave trade from several centuries ago may explain these observations.8 – 10 The colonial-era trans-Atlantic slave trade, which was largely controlled by the Europeans, resulted in west Africans (including the ancestors of present-day Ghanaians) being brought to the Americas. In contrast, the slave trade from east Africa brought many ancestors of contemporary Ethiopians to the mid-East and Asia. AAs therefore are likely to have more shared ancestry with west Africans/Ghanaians compared with Ethiopians.
Confirming that our study cases are broadly representative of national and international populations was challenging because of the paucity of published data on breast cancer phenotypes in Africa. Table 5 summarizes comparisons of our study AA and WA cases with population-based data from the SEER Program, demonstrating that patterns of disease in the HFHS cases were indeed comparable to national statistics.7 The study Ghanaian cases were generally comparable to other reports of breast cancer in Ghana with regard to the young median age at diagnosis and the high frequency of ER-negative as well as TNBC.11 , 12 A noteworthy exception was the study by Adjei et al., comparing a relatively small number of Ghanaian breast tumors (n = 51) to the tumors of Norway, with all immunohistochemistry performed at the Norwegian collaborating cancer facility.13 This study found a TNBC frequency of only 22 % among the Ghanaian cases; however of note, this study also reported a notably low frequency of TNBC in the comparison Norwegian population, at only 7 %. The frequency of TNBC among Ghanaian cases therefore was threefold higher than the comparison Norwegian cases, a statistically significant difference (p = 0.018). Very little data are available on molecular marker expression of breast cancers in Ethiopia, but work conducted by a German group has reported similarly low prevalence of ER-negative breast cancer in Ethiopian cases from Addis Ababa University (34.7 %) compared with our St. Paul’s Millennium Hospital study (28.6 %).14
Interestingly, SEER-based data evaluating breast cancers among women in the United States diagnosed 1996–2008 with diverse African ancestral backgrounds confirms differences in frequency of ER-negative breast cancer related to heritage.15 East African-born patients (186 patients, predominantly from Ethiopia or Eritrea) had ER-negative tumors in 22 % of cases compared with 33 % ER-negative tumors among 143 west African-born patients (mostly from Nigeria). Frequency of ER-negative tumors among WAs (18 %) was similarly low as that observed among east African-born patients. In contrast, U.S.-born AAs had higher prevalence of ER-negative tumors (31.2 %).
Clearly, more research is warranted in the study of breast cancer related to African ancestry. Our study suggests that west African ancestry is associated with inherited susceptibility for TNBC. Future work should strive to document population-based data on breast cancer incidence and mortality in different areas of Africa. This research and its relevance to breast cancer disparities in the United States can be refined by utilizing germline genotyping studies and Ancestry Informative Markers to quantify extent of east African versus west African ancestry in AA breast cancer patients.16 Furthermore, gene expression studies of tumors in breast cancer patients with African ancestry are needed so that we can define the extent to which TNBC subtypes are similar or different across diverse populations.17
This type of research holds great promise with regard to the critically important and relevant goals of understanding disparities in breast cancer burden related to racial-ethnic identity domestically, investing in the oncology care systems of low/middle-income countries, and identifying additional markers of hereditary susceptibility for TNBC.
References
Fitzgibbons PL et al. Template for reporting results of biomarker testing of specimens from patients with carcinoma of the breast. Arch Pathol Lab Med. 2014;138(5):595–601.
Hammond ME, et al. American society of clinical oncology/college of American pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract. 2010;6(4):195–7.
Wolff AC, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31(31):3997–4013.
Newman LA, et al. Meta-analysis of survival in African American and white American patients with breast cancer: ethnicity compared with socioeconomic status. J Clin Oncol. 2006;24(9):1342–9.
Kohler BA, et al. Annual report to the nation on the status of cancer, 1975–2011, featuring incidence of breast cancer subtypes by race/ethnicity, poverty, and state. J Natl Cancer Inst. 2015;107(6):djv048.
Chavez-Macgregor M, et al. Male breast cancer according to tumor subtype and race: a population-based study. Cancer. 2013;119(9):1611–7.
DeSantis CE, et al. Breast cancer statistics, 2015: convergence of incidence rates between black and white women. CA Cancer J Clin. 2016;66(1):31–42.
Campbell MC, et al. The peopling of the African continent and the diaspora into the new world. Curr Opin Genet Dev. 2014;29:120–32.
Salas A, et al. Charting the ancestry of African Americans. Am J Hum Genet. 2005;77(4):676–80.
Bryc K, et al. Genome-wide patterns of population structure and admixture in West Africans and African Americans. Proc Natl Acad Sci USA. 2010;107(2):786–91.
Ohene-Yeboah M, Adjei E. Breast cancer in Kumasi, Ghana. Ghana Med J. 2012;46(1):8–13.
Der EM, et al. Triple-negative breast cancer in Ghanaian women: the Korle Bu teaching hospital experience. Breast J. 2015;21(6):627–33.
Adjei EK, et al. Hormone receptors and Her2 expression in breast cancer in sub-Saharan Africa. A comparative study of biopsies from Ghana and Norway. Breast J. 2014;20(3):308–11.
Kantelhardt EJ, et al. The prevalence of estrogen receptor-negative breast cancer in Ethiopia. BMC Cancer. 2014;14:895.
Jemal A, Fedewa SA. Is the prevalence of ER-negative breast cancer in the US higher among Africa-born than US-born black women? Breast Cancer Res Treat. 2012;135(3):867–73.
Palmer JR, et al. Genetic susceptibility loci for subtypes of breast cancer in an African American population. Cancer Epidemiol Biomarkers Prev. 2013;22(1):127–34.
Lehmann BD, et al. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest. 2011;121(7):2750–67.
Acknowledgment
This work was supported by research funds contributed by the following agencies/organizations: Henry Ford Health System International Center for the Study of Breast Cancer Subtypes, Susan G. Komen for the Cure, Think Pink Rocks, QVC Fashion Footwear New York City, Susan and Richard Bayer Breast Cancer Research Fund, University of Michigan Comprehensive Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Additional information
Drs. Lisa A. Newman and Azadeh Stark have contributed equally as senior authors for this project.
Rights and permissions
About this article
Cite this article
Jiagge, E., Jibril, A.S., Chitale, D. et al. Comparative Analysis of Breast Cancer Phenotypes in African American, White American, and West Versus East African patients: Correlation Between African Ancestry and Triple-Negative Breast Cancer. Ann Surg Oncol 23, 3843–3849 (2016). https://doi.org/10.1245/s10434-016-5420-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5420-z