Abstract
Background
Young age at breast cancer diagnosis has been associated with increased risk of recurrence and mortality. We reevaluated this assumption in a large, modern cohort of women diagnosed with breast cancer at age ≤40 years.
Methods
We identified women with breast cancer at age ≤40 years at a single institution from 1996–2008. We assessed locoregional recurrence (LRR), distant recurrence, disease-free survival (DFS), and overall survival (OS), and correlated patient and tumor characteristics with outcomes.
Results
We identified 584 women aged ≤40 years with breast cancer. Median age was 37 years, and median follow-up was 124 months; 61.5 % were stages 0–I and 38.5 % were stages II–III. Overall, 57.4 % had lumpectomies and 42.5 % mastectomies. DFS was 93 % at 5 years and 84.5 % at 10 years. OS was 93 % at 5 years and 86.5 % at 10 years. On multivariate analysis, worse DFS was associated with positive nodes (p = 0.002); worse OS was associated with larger tumor size (p = 0.042). When stratified by lumpectomy versus mastectomy, there were no significant differences in survival or recurrence. For lumpectomy patients, DFS was 96 % at 5 years and 88 % at 10 years; OS was 96 % at 5 years and 89 % at 10 years. For mastectomy patients, DFS was 89.5 % at 5 years and 79 % at 10 years; OS was 90 % at 5 years and 83 % at 10 years. Lumpectomy LRR rates were 1 % at 5 years and 4 % at 10 years. Mastectomy LRR rates were 3.5 % at 5 years and 8.7 % at 10 years.
Conclusions
Outcomes for women with breast cancer at age ≤40 years have improved. Lumpectomy recurrence rates are low, suggesting that lumpectomy is oncologically safe for young breast cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In 2015, the American Cancer Society estimated 10,500 new diagnoses of invasive breast cancer and 1650 in situ cases for women ages ≤40 years.1 Despite increasing public awareness about breast cancer, advances in breast cancer screening, and increased availability of genetic testing, we previously reported that up to 71 % of breast cancers in young women were palpable at diagnosis with larger tumors and a higher rate of positive axillary nodes at presentation compared with older women.2
Young age at breast cancer diagnosis was previously found to be an independent risk factor for disease recurrence.3–5 Among 10,709 women in five NSABP trials, 12-year rates of ipsilateral breast tumor recurrences for women ages ≤49, 50–59, and ≥60 years were 9.6, 5.8, and 5.6 %, respectively.5 In patients of all ages, the risk of in-breast recurrence after breast-conserving therapy (BCT) with radiation is approximately 1 % per year, up to 20 years after initial treatment.6 Patients who develop locoregional recurrence (LRR), as in-breast, chest wall, or regional nodal recurrence, have an increased risk of metastatic disease and death from breast cancer.4,7
Historically, young age has been associated with poorer survival. In one study, 980 women diagnosed with early-stage breast cancer between 1981 and 1991 were divided into three groups (ages ≤35, 36–50, and >50 years), and younger women were found to have a worse overall survival (71 vs. 83 vs. 92 %, respectively).8 However, differences related to age may be narrowing as the management of breast cancer improves. Better preoperative imaging, margin assessment, endocrine therapy, systemic therapy, and standard use of radiation therapy with a tumor bed boost can reduce recurrence and improve survival.9–11 We sought to reevaluate outcomes in a large, modern cohort of women diagnosed with stages 0–III breast cancer by age 40 years. We assessed rates of recurrence and survival and examined patient factors, tumor characteristics, and treatment modalities potentially associated with outcomes in young breast cancer patients.
Materials and Methods
Following Institutional Review Board approval, retrospective review of medical records identified women aged ≤40 years at a single institution who were diagnosed with stages 0–III breast cancer in 1996–2008. Demographic data, family history, initial presentation, genetic testing, imaging studies, surgery type, tumor characteristics, and neoadjuvant/adjuvant therapy received were recorded. Standard BRCA1/2 sequencing was used for genetic testing for most patients; rearrangement testing was added in patients diagnosed after 2006. Only a small number of patients underwent multigene panel testing. However, if updated or additional testing was performed, these results were included. Site of first recurrence and the interval between recurrence and/or death or last follow-up were recorded. If the first recurrence was locoregional, the first site of distant recurrence was also recorded. Patients were censored at their last follow-up visit.
We assessed LRR, distant recurrence (DR), disease-free survival (DFS), and overall survival (OS). LRR was defined as recurrent cancer in the ipsilateral breast, chest wall, or regional lymph nodes (ipsilateral axillary, internal mammary, infraclavicular, and/or supraclavicular) as defined by the American Joint Committee on Cancer (AJCC 7th Edition).12 Contralateral or histologically distinct breast cancers were considered new events and were not included in the recurrence analyses. Survival data were gathered using the consensus of the Tumor Registry, Massachusetts Death Certificate Data, and the Social Security Master Death Index to determine the date of death for each patient.
Univariate analyses were conducted using Pearson’s Chi squared test, and multivariate analyses were conducted using Cox’s proportional hazard regression modeling. Survival and recurrence data were analyzed using the Kaplan–Meier estimator method. The log-rank test was used for the comparison of survival/recurrence curves. A p value ≤0.05 was considered statistically significant. All analyses were done using Stata (StataCorp. 2011. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP.)
Results
We identified 628 women aged ≤40 years diagnosed with stages 0–III primary breast cancer from 1996–2008. Follow-up data were available for 584 patients (Table 1). Median follow-up was 124 months (range 5–236); median age was 37 years (range 21–40) with 33 % ≤35 and 9 % ≤30 years. The majority of patients were self-identified as white/Caucasian (84.2 %, n = 492), and the remainder as Hispanic/Latino (5.3 %, n = 31), Asian (5.3 %, n = 31), black/African-American (2.7 %, n = 16), or unknown (2.4 %, n = 14). Clinically, 20.6 % were stage 0, 40.9 % stage I, 33.4 % stage II, and 5.1 % stage III.
Overall, 57.4 % had lumpectomies, 42.5 % had mastectomies, and one patient had an axillary dissection without breast surgery for positive axillary nodes with an occult primary. Among lumpectomy patients, 96 % (320/335) received radiation, and 36 % of mastectomy patients (90/248) received postmastectomy radiation (PMRT). Among patients with invasive cancer, 79.8 % (372/466) received chemotherapy, the majority (75.5 %, n = 281) receiving AC (doxorubicin and cyclophosphamide) or AC-T (doxorubicin, cyclophosphamide, and paclitaxel). For the 91 patients with HER2 positive invasive cancer, trastuzumab was administered in 48.4 % (n = 44). Among those with ER+ invasive cancers, 87 % (288/331) received endocrine therapy, and 37.7 % (26/69) of those with ER+ DCIS received endocrine therapy.
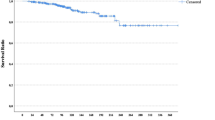
In follow-up of the entire cohort, there were 27 new breast primaries (4.6 %, histologically distinct and/or in the contralateral breast), 132 locoregional and/or distant recurrences, and 86 deaths from all causes. Overall, survival was quite high and LRR quite low compared with historical data. Kaplan–Meier estimates for LRR were 2 % at 5 years and 5.9 % at 10 years (Fig. 1a). DFS was 93 % at 5 years and 84.5 % at 10 years (data not shown). OS was 93 % at 5 years and 86.5 % at 10 years (Fig. 1c). For patients with stage 0 disease, OS was 100 % at 5 years and 96.7 % at 10 years. For patients with stage I disease, OS was 96.5 % at 5 years and 88.1 % at 10 years. For patients with stage II disease, OS was 88.3 % at 5 years and 82.5 % at 10 years. For patients with stage III disease, OS was 72.6 % at 5 years and 60.6 % at 10 years (Fig. 1d).
Among 446 women with invasive cancer, there were 122 locoregional and/or distant recurrences and 81 deaths from all causes at median follow-up of 124 months (range 5–235). Among 118 women with DCIS, there were 10 locoregional and/or distant recurrences and 5 deaths from all causes at median follow-up of 125 months (range 11–236). In the entire cohort, median time from diagnosis of breast cancer to any recurrence was 42 months (range 3–158). Median time to death following any recurrence was 65 months (range 5–201, n = 79).
Across the cohort of 584 patients, worse DFS and OS were associated with positive lymph nodes and larger tumor size. On univariate analysis, survival was not associated with ER/PR status, HER2 status, triple-negative disease, or the presence of a high-risk genetic mutation (Supplemental Table 1; Supplemental Fig. 1). For DFS, multivariate analysis, including age, invasive disease, tumor size, tumor grade 3, presence of lymphovascular invasion (LVI), positive lymph nodes, type of surgery, chemotherapy, and radiation, showed that only positive lymph nodes remained individually significant in predicting a worse DFS (by Cox regression, p = 0.002; Table 2). With respect to OS, multivariate analysis including the same variables showed that only tumor size remained individually significant in predicting a worse OS (by Cox regression, p = 0.042; Table 2).
We next evaluated how breast-conserving therapy (BCT) versus mastectomy affected patient outcomes. In this retrospective series, selection of surgical procedures was based on tumor features and patient and physician preferences.
Table 3 summarizes patient and tumor characteristics stratified by surgical procedure (lumpectomy vs. mastectomy). Median follow-up was slightly longer for lumpectomy patients (means: 127 vs. 115 months, p = 0.007). There were no significant differences in age at diagnosis, presence of genetic mutations, histological tumor type, or nodal status between lumpectomy and mastectomy patients. As expected, women undergoing mastectomy were more likely to have a higher clinical T stage (p < 0.001). There were significant differences in the distribution of disease stages between those undergoing lumpectomy versus mastectomy (p = 0.001), with stage 0 and stage III tumors more common among mastectomy patients. Triple-negative status was similar between lumpectomy and mastectomy patients. The mastectomy cohort included more high T-stage patients, and as expected, neoadjuvant chemotherapy was more common (p = 0.038). After adjusting for T stage, the difference in receipt of neoadjuvant chemotherapy did not persist.
For patients undergoing BCT, DFS was 96 % at 5 years and 88 % at 10 years, and OS was 96 % at 5 years and 89 % at 10 years. For patients undergoing mastectomy, DFS was 89.5 % at 5 years and 79 % at 10 years, whereas OS was 90 % at 5 years and 83 % at 10 years. These differences are not surprising as the mastectomy group included more patients with higher T stage and disease stage (Table 3). However, there were no significant differences in survival or recurrence based on the initial surgical procedure (log-rank test, unadjusted, all p > 0.05; Fig. 2a, b).
Kaplan–Meier estimates for the entire cohort stratified by type of surgery (lumpectomy vs. mastectomy) of (a) locoregional recurrence (log-rank test, p = 0.614) and (b) overall survival (log-rank test, p = 0.096). Kaplan–Meier estimates of overall survival stratified by type of surgery for women with (c) Stages 0–I (Stage 0, log-rank test, p = 0.749; Stage I, log-rank test, p = 0.673), and (d) Stages II–III disease (Stage II, log-rank test, p = 0.156; Stage III, log-rank test, p = 0.281)
Risk of LRR was very low after lumpectomy among young women in our series. Rates of any LRR after lumpectomy were 1 % at 5 years and 4 % at 10 years. Rates of ipsilateral breast recurrence after lumpectomy were 0.6 % at 5 years and 2.8 % at 10 years, and rates of regional nodal recurrence after lumpectomy were 0.3 % at 5 years and 1.3 % at 10 years. For mastectomy patients, rates of any LRR were 3.5 % at 5 years and 8.7 % at 10 years. Rates of ipsilateral chest wall recurrence after mastectomy were 2.1 % at 5 years and 4.7 % at 10 years, and rates of regional nodal recurrence were 1.8 % at 5 years and 5.9 % at 10 years.
When stratified by clinical stage and surgical treatment (lumpectomy vs. mastectomy), there was no significant difference in OS for patients with stages 0 or I disease (Fig. 2c; stage 0, log-rank test, p = 0.749; stage I, log-rank test, p = 0.673). However, for those with stages II–III disease, mastectomy patients had a trend towards a worse OS (Fig. 2d, stage II, log-rank test, p = 0.156; stage III, log-rank test, p = 0.281). After adjusting for tumor size using clinical T stage, surgical procedure (lumpectomy vs. mastectomy for stages II–III) was not significantly associated with OS (by Cox regression, p = 0.160 for the surgical treatment, p = 0.005 for clinical T stage).
Discussion
Several large studies published before 2010 found young age at diagnosis to be an independent predictor of poor prognosis.13–16 Beadle et al. found OS to be 64.6 % at 10 years, whereas Coulombe et al. reported an OS of 78.1 % at 10 years.17,18 In our study, OS was 86.5 % at 10 years, suggesting that recent improvements in diagnosis and treatment have translated into improved outcomes for young women.
We found no significant difference in survival when comparing lumpectomy versus mastectomy among our patients. A recent meta-analysis evaluating BCT versus mastectomy in 22,598 women ages ≤40 years with early-stage breast cancer also found no significant difference in the risk of death related to the surgical procedure.19
In addition to improved OS, we report significantly lower LRR rates compared with older series. For example, Voogd et al. reported 10-year actuarial LRR rates for patients aged ≤35 years as 35 % after BCT.20 Beadle et al. reported a 10-year actuarial LRR rate of 15.8 % following BCT and 12.5 % following mastectomy in a cohort of 652 women aged ≤35 years.17 In comparison, our LRR was 4 % after BCT and 8.7 % after mastectomy at 10 years by Kaplan–Meier analysis. In a separate study of 1434 consecutive patients undergoing BCT at our institution, some of whom also were included in this study, the 5-year LRR rate following BCT in women aged 23–46 years was 5 %.21
We found that age (as a continuous variable in women aged ≤40 years) was not significantly associated with recurrence or survival. This may suggest that if a woman is diagnosed with breast cancer at age ≤40 years, her exact age may not contribute substantially to her prognosis.
Bharat et al. previously reported that younger women were 1.5 times more likely to die from breast cancer than older women.13 In contrast, outcomes in our cohort of young women with breast cancer were very similar to outcomes in the general breast cancer population. According to 2015 data from the American Cancer Society, survival among all women with invasive breast cancer is 89 % after 5 years and 83 % after 10 years.1 When women diagnosed with breast cancer between 2005 and 2011 were stratified by stage using SEER data, Howlander et al. reported 5-year relative survival rates of 99 % for those with localized disease and 85 % for regional disease, which is comparable to our findings in women aged ≤40 years.22 In the SEER data, 61 % had localized disease at diagnosis, whereas 32 % had regional disease, similar to the stage distribution among our young patients.1,22 These data suggest that young women’s breast cancers are now being detected at stages similar to older women’s cancers.
The reasons for the improved outcomes observed in our study are likely multifactorial. Patients in our series, particularly in later years, had the benefit of digital mammography as well as the increasing use of breast MRI in their preoperative workup (data not shown). Better preoperative imaging allows for improved surgical treatment planning and identification of patients not eligible for breast conservation. Better staging also allowed us to exclude patients with metastatic disease at diagnosis who may have been included in prior series of young breast cancer patients.
Improved lumpectomy margin assessment has been shown to improve outcomes.23 Standardization of specimen handling and orienting, use of shaved margins, and intraoperative specimen radiography have helped to improve lumpectomy margin assessment, reduce the need for reoperation, and potentially decrease the risk of local recurrence.24–26
Advancements in radiation therapy strategies likely contributed to favorable outcomes in our cohort. We routinely used a boost to the lumpectomy tumor bed, which has been shown to reduce LRR in young women.27 The use of PMRT in more than a third of our mastectomy patients potentially contributed to our low LRR rate after mastectomy and also may contribute to improved survival.28,29
The evolution of systemic therapy, in particular, routine use of endocrine therapy after the 1998 Early Breast Cancer Trialists meta-analysis, has undoubtedly improved outcomes in young breast cancer patients.30 In our cohort, more than 77 % of patients with ER-positive breast cancer received endocrine therapy, which improves control of both local and distant disease. Randomized trials have shown that addition of a taxane to anthracycline-based regimens provides improved DFS.31,32 Current NCCN guidelines recommend preferential use of regimens incorporating both anthracyclines and taxanes, and use of these agents was standard in our cohort.33
Despite the marked improvement in young women’s breast cancer outcomes reflected in our cohort, strategies for further improvement exist. Genetic testing of more young women with strong family histories would allow earlier identification of risk gene mutation carriers for high-risk screening and risk reducing surgery.33,34 Although NCCN guidelines outline eligibility for MRI screening of high-risk women, we previously reported underutilization of high-risk screening algorithms and genetic testing in young women.33,35 Finally, our results show that despite remarkable progress, young women still have ongoing risks of recurrence and mortality over time, confirming the need for continued improvement in systemic and other therapies.
In summary, outcomes for women diagnosed with breast cancer at age ≤40 years have improved over time, with stage distribution and survival now similar to that of older women. Rates of LRR following BCT are low, suggesting that BCT is an oncologically safe approach for young breast cancer patients. We believe that improvements in preoperative imaging and margin assessment, routine use of modern radiation and endocrine therapy, and advances in chemotherapy regimens have all contributed to improving the prognosis of young breast cancer patients. In the future, better identification and screening of high-risk patients may further improve outcomes.
References
American Cancer Society. Breast cancer facts & figures 2015–2016. Atlanta: American Cancer Society, Inc.; 2015.
Zabicki K, Colbert JA, Dominguez FJ, et al. Breast cancer diagnosis in women ≤40 versus 50 to 60 years: increasing size and stage disparity compared with older women over time. Ann Surg Oncol. 2006;13(8):1072–7.
de Bock GH, van der Hage JA, Putter H, Bonnema J, Bartelink H, van de Velde CJ. Isolated loco-regional recurrence of breast cancer is more common in young patients and following breast conserving therapy: long-term results of European organisation for research and treatment of cancer studies. Eur J Cancer. 2006;42(3):351–6.
Komoike Y, Akiyama F, Iino Y, et al. Ipsilateral breast tumor recurrence (IBTR) after breast-conserving treatment for early breast cancer: risk factors and impact on distant metastases. Cancer. 2006;106(1):35–41.
Anderson SJ, Wapnir I, Dignam JJ, et al. Prognosis after ipsilateral breast tumor recurrence and locoregional recurrences in patients treated by breast-conserving therapy in five national surgical adjuvant breast and bowel project protocols of node-negative breast cancer. J Clin Oncol. 2009;27(15):2466–73.
Kreike B, Hart AA, van de Velde T, et al. Continuing risk of ipsilateral breast relapse after breast-conserving therapy at long-term follow-up. Int J Radiat Oncol Biol Phys. 2008;71(4):1014–21.
Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;366(9503):2087–106.
Fowble BL, Schultz DJ, Overmoyer B, et al. The influence of young age on outcome in early stage breast cancer. Int J Radiat Oncol Biol Phys. 1994;30(1):23–33.
Kaplan HG, Malmgren JA, Atwood MK, Calip GS. Effect of treatment and mammography detection on breast cancer survival over time: 1990–2007. Cancer. 2015;121(15):2553–61.
Saadatmand S, Bretveld R, Siesling S, Tilanus-Linthorst MM. Influence of tumour stage at breast cancer detection on survival in modern times: population-based study in 173,797 patients. BMJ. 2015;351:h4901.
Berry DA, Cronin KA, Plevritis SK, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353(17):1784–92.
Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual. 7th ed. New York: Springer-Verlag; 2010.
Bharat A, Aft RL, Gao F, Margenthaler JA. Patient and tumor characteristics associated with increased mortality in young women (< or = 40 years) with breast cancer. J Surg Oncol. 2009;100(3):248–51.
Gnerlich JL, Deshpande AD, Jeffe DB, Sweet A, White N, Margenthaler JA. Elevated breast cancer mortality in women younger than age 40 years compared with older women is attributed to poorer survival in early-stage disease. J Am Coll Surg. 2009;208(3):341–7.
de la Rochefordiere A, Asselain B, Campana F, et al. Age as prognostic factor in premenopausal breast carcinoma. Lancet. 1993;341(8852):1039–43.
Love RR, Duc NB, Dinh NV, Quy TT, Xin Y, Havighurst TC. Young age as an adverse prognostic factor in premenopausal women with operable breast cancer. Clin Breast Cancer. 2002;2(4):294–8.
Beadle BM, Woodward WA, Tucker SL, et al. Ten-year recurrence rates in young women with breast cancer by locoregional treatment approach. Int J Radiat Oncol Biol Phys. 2009;73(3):734–44.
Coulombe G, Tyldesley S, Speers C, et al. Is mastectomy superior to breast-conserving treatment for young women? Int J Radiat Oncol Biol Phys. 2007;67(5):1282–90.
Vila J, Gandini S, Gentilini O. Overall survival according to type of surgery in young (≤40 years) early breast cancer patients: a systematic meta-analysis comparing breast-conserving surgery versus mastectomy. Breast. 2015;24(3):175–81.
Voogd AC, Nielsen M, Peterse JL, et al. Differences in risk factors for local and distant recurrence after breast-conserving therapy or mastectomy for stage I and II breast cancer: pooled results of two large european randomized trials. J Clin Oncol. 2001;19(6):1688–97.
Arvold ND, Taghian AG, Niemierko A, et al. Age, breast cancer subtype approximation, and local recurrence after breast-conserving therapy. J Clin Oncol. 2011;29(29):3885–91.
Howlader N, Noone A, Krapcho M, et al. SEER cancer statistics review. 1975–2012. http://seer.cancer.gov/csr/1975_2012.
Singletary SE. Surgical margins in patients with early-stage breast cancer treated with breast conservation therapy. Am J Surg. 2002;184(5):383–93.
Cabioglu N, Hunt KK, Sahin AA, et al. Role for intraoperative margin assessment in patients undergoing breast-conserving surgery. Ann Surg Oncol. 2007;14(4):1458–71.
Chagpar AB, Killelea BK, Tsangaris TN, et al. A randomized, controlled trial of cavity shave margins in breast cancer. N Engl J Med. 2015;373(6):503–10.
Singh M, Singh G, Hogan KT, Atkins KA, Schroen AT. The effect of intraoperative specimen inking on lumpectomy re-excision rates. World J Surg Oncol. 2010;8:4.
Bartelink H, Maingon P, Poortmans P, et al. Whole-breast irradiation with or without a boost for patients treated with breast-conserving surgery for early breast cancer: 20-year follow-up of a randomised phase 3 trial. Lancet Oncol. 2015;16(1):47–56.
Overgaard M, Hansen PS, Overgaard J, et al. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. danish breast cancer cooperative group 82b trial. N Engl J Med. 1997;337(14):949–55.
Ragaz J, Jackson SM, Le N, et al. Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. N Engl J Med. 1997;337(14):956–62.
Early Breast Cancer Trialists’ Collaborative Group. Tamoxifen for early breast cancer: an overview of the randomised trials. Lancet. 1998;351(9114):1451–67.
Mamounas EP, Bryant J, Lembersky B, et al. Paclitaxel after doxorubicin plus cyclophosphamide as adjuvant chemotherapy for node-positive breast cancer: results from NSABP B-28. J Clin Oncol. 2005;23(16):3686–96.
Bear HD, Anderson S, Smith RE, et al. Sequential preoperative or postoperative docetaxel added to preoperative doxorubicin plus cyclophosphamide for operable breast cancer: national surgical adjuvant breast and bowel project protocol B-27. J Clin Oncol. 2006;24(13):2019–27.
Gradishar WJ, Anderson BO, Balassanian R, et al. NCCN clinical practice guidelines in oncology: breast cancer. version 1. 2016.
Rosenberg SM, Ruddy KJ, Tamimi RM, et al. BRCA1 and BRCA2 mutation testing in young women with breast cancer. JAMA Oncol. 2016;2:730–36.
Samphao S, Wheeler AJ, Rafferty E, et al. Diagnosis of breast cancer in women age 40 and younger: delays in diagnosis result from underuse of genetic testing and breast imaging. Am J Surg. 2009;198(4):538–43.
Disclosure
The authors have no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10434_2016_5404_MOESM1_ESM.tif
Supplementary material 1 (TIFF 1549 kb) Kaplan-Meier estimates for the entire cohort stratified by (A) tumor grade (log rank test, p=0.039)
10434_2016_5404_MOESM2_ESM.tif
Supplementary material 2 (TIFF 1549 kb) Kaplan-Meier estimates for the entire cohort stratified by (B) lymphovascular invasion (log rank test, p<0.001)
10434_2016_5404_MOESM3_ESM.tif
Supplementary material 3 (TIFF 1549 kb) Kaplan-Meier estimates for the entire cohort stratified by (C) lymph node status (log rank test, p<0.001)
10434_2016_5404_MOESM4_ESM.tif
Supplementary material 4 (TIFF 1549 kb) Kaplan-Meier estimates for the entire cohort stratified by (D) triple negative receptor status (log rank test, p=0.968)
10434_2016_5404_MOESM5_ESM.docx
Supplementary material 5 (DOCX 13 kb) Univariate analyses (by Cox regression) of disease-free survival and overall survival. HR: hazard ratio, 95%CI: 95% confidence interval, LVI: lymphovascular invasion, ER: estrogen receptor, PR: progesterone receptor, HER2: human epidermal growth factor 2
Rights and permissions
About this article
Cite this article
Plichta, J.K., Rai, U., Tang, R. et al. Factors Associated with Recurrence Rates and Long-Term Survival in Women Diagnosed with Breast Cancer Ages 40 and Younger. Ann Surg Oncol 23, 3212–3220 (2016). https://doi.org/10.1245/s10434-016-5404-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5404-z