Abstract
Background
This study evaluated the use of axillary surgery (AS), including sentinel lymph node biopsy (SLNB), for patients with ductal carcinoma in situ (DCIS) and the factors associated with its use. To determine whether utilization of SLNB is appropriate, predictors of SLNB performance were compared with factors predictive of tumor upstaging.
Methods
The National Cancer Data Base was utilized to identify patients with American Joint Committee on Cancer (AJCC) clinical stage 0 breast cancer treated from 2004 to 2013. DCIS with microinvasion was excluded. Chi square tests and logistic regression were used to examine patient, tumor, and facility features associated with SLNB and tumor upstaging.
Results
Of the 218,945 total patients, 155,093 (70.8 %) underwent lumpectomy, and 63,852 (29.2 %) underwent mastectomy. SLNB was performed for 19.0 % of lumpectomy patients and 63.5 % of mastectomy patients. Multivariate analysis for 2012–2013 demonstrated that estrogen receptor (ER)-negative and grade 3 tumors were more likely to be treated with SLNB in both groups. Tumor size was significant only for the lumpectomy patients who underwent one operation. Further, 22.8 % of lumpectomy patients and 18.7 % of mastectomy patients who underwent AS were upstaged compared with 1.8 % of lumpectomy and 3.6 % of mastectomy patients who did not undergo AS. Tumor upstaging was predicted by ER-negative status (odds ratio [OR] 2.99; 95 % confidence interval [CI] 2.76–3.24) but not by higher grade or larger tumor size.
Conclusions
Use of SLNB for DCIS is high with mastectomy, and nearly one fifth of the lumpectomy patients underwent SLNB. However, the performance of AS was strongly associated with the likelihood of upstaging in both groups, suggesting that surgical judgment plays an important role in this decision.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In 2005, clinical practice guidelines recommended against the routine use of sentinel lymph node biopsy (SLNB) for patients with ductal carcinoma in situ (DCIS) on core biopsy undergoing breast-conserving surgery (BCS).1 At that time, exceptions for consideration of SLNB included large DCIS (>5 cm), suspected or proven microinvasion, and performance of mastectomy. Currently, National Comprehensive Cancer Network (NCCN) and American Society of Clinical Oncology (ASCO) guidelines state that SLNB for DCIS should be performed for a mass lesion at physical examination or imaging highly suggestive of invasive cancer, when the area of DCIS is larger than 5 cm, for patients undergoing mastectomy, and when surgical excision is in an anatomic location that would preclude future SLNB.2,3
The primary reason to perform SLNB at the time of BCS for patients with DCIS is to avoid a second operation if invasive cancer is found on final pathology. DCIS diagnosed on needle biopsy may be upstaged to invasive cancer due to the inherent sampling limitations of biopsy technique, and occurs in up to 26 % of patients.4 Moreover, the reported incidence of SLNB positivity among patients with DCIS ranges from 2 to 14 %, likely because these studies include patients upstaged to invasive cancer at final pathology.5–11 Factors predictive of upstaging include palpability, a mammographic mass, larger size, multicentric disease, suspicion of microinvasion, high nuclear grade, necrosis, and use of smaller-gauge biopsy needles.4,10,12,13
Reported rates for performance of SLNB for DCIS range from 21 to 97 %, but these rates are reported primarily from single-institution studies examining predictors of SLNB positivity, which select for tumors with high-risk characteristics.6,14–16 In 2010, the rate was 17.8 % for lumpectomy patients and 67.1 % for mastectomy patients in the Surveillance, Epidemiology, and End Results (SEER) database, although this was based on the number of lymph nodes examined rather than the specific type of axillary surgery.17
In 2012, the National Cancer Data Base (NCDB) began collecting information on whether SLNB or axillary lymph node dissection (ALND) was performed in addition to the number of nodes removed. We utilized this variable to examine trends in the use of axillary surgery (AS) for DCIS and to identify factors associated with SLNB performance for lumpectomy and mastectomy patients. We also sought to examine whether the performance of SLNB differed between patients whose breast tumor was upstaged from DCIS to invasive disease after excision and those who did not have tumor upstaging. The findings from this study help to determine whether SLNB is overutilized for DCIS and whether factors outside the current NCCN and ASCO guidelines are associated with SLNB use.
Methods
We conducted a retrospective cohort study of patients with a diagnosis of DCIS using the participant user file of the NCDB, a joint collaboration of the American Cancer Society and the American College of Surgeon’s Commission on Cancer. In this study, no patient, provider, or hospital identifiers were examined, and institutional review board approval was deemed not necessary.
Patient Cohort
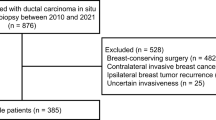
The NCDB was queried from 2004 to 2013 to identify female breast cancer patients 18 years of age or older with DCIS. Only patients who were clinical American Joint Committee on Cancer (AJCC) stage 0 (T classification blank, 0, X, or IS) and with a known number of regional lymph nodes examined were included in the study. Patients with microinvasion were coded as AJCC cT1. No code for “suspicious for microinvasion” is available in the NCDB, and these patients were therefore included as cTis. Patients with a prior cancer diagnosis and those who were diagnosed and treated at different institutions were excluded.
Surgical treatment included lumpectomy or mastectomy as identified by procedure code.18 Axillary surgery was defined as the surgical removal of any axillary regional lymph nodes. Prior to 2012, only the number of regional lymph nodes examined was included in the NCDB. In 2012, the NCDB began collecting data for the scope of regional lymph node surgery variable, which specifically codes for SLNB, ALND, and other regional lymph node removal.19 Upstaging was defined as final pathologic T stage greater than pT0 or pTis.
Clinical Variables
Patient characteristics included age (<50, 50–70, >70 years), race (Caucasian, African American, Hispanic, Asian Pacific Islander, other), socioeconomic status (SES) (high, middle, or low based on median household income and education level in the patient’s zip code area), insurance status (not insured, private insurance/managed care, Medicaid, Medicare, other government program, and unknown), and comorbidities (based on the Deyo Charlson comorbidity index). Facility characteristics included facility type (community cancer program, comprehensive community cancer program, academic/research program, and other) and facility location, categorized according to U.S. census regions.20 Facility volume was based on the National Accreditation Program for Breast Centers (NAPBC) analytic case load and categorized as low (0–100 cases/year), mid (101–250 cases/year), and high (>250 cases/year).21 Tumor characteristics included AJCC clinical and pathologic stage (0–IV), tumor size (≤1, 1.1–4, >4 cm, unknown), estrogen receptor (ER) status (positive, negative, unknown), and grade (1–2, 3, unknown).
Statistical Analysis
Patient, facility, and tumor characteristics were compared between treatment groups using descriptive statistics and Chi square tests. Surgical trends over time were assessed based on the use of AS. When the scope of regional lymph node surgery variable was available (2012–2013), factors associated with SLNB use and tumor upstaging were evaluated using univariate and multivariate logistic regression models. Statistical analysis was conducted using SPSS statistical software (SPSS for Windows, version 22; SPSS, Chicago, IL, USA). All tests were two-sided, and a p value of 0.05 or lower was considered statistically significant.
Results
Patient, Facility, and Tumor Characteristics
Of the 218,945 patients with AJCC clinical stage TisN0 breast cancer treated from 2004 to 2013, 155,093 (70.8 %) underwent lumpectomy and 63,852 (29.2 %) underwent mastectomy (Table 1). Axillary surgery was performed for 22.6 % of lumpectomy patients and 82.5 % of mastectomy patients. The mean and median numbers of nodes removed were respectively 2.7 and 2.0 for lumpectomy patients, and 3.7 and 2.0 for mastectomy patients.
Trends in Axillary Surgery for Lumpectomy and Mastectomy Patients, 2004–2013
The use of AS between 2004 and 2013 was assessed using the number of lymph nodes examined (Fig. 1). The AS rates for unilateral and bilateral mastectomy patients were nearly identical and combined into the “mastectomy” group. In 2013, AS rates increased to 87.4 % for mastectomy patients and 23.8 % for lumpectomy patients.
SLNB and ALND for Patients with DCIS, 2012–2013
Using the scope of regional lymph node surgery variable from 2012 to 2013, SLNB was performed for 19.0 % of lumpectomy patients and 63.5 % of mastectomy patients, whereas SLNB followed by ALND was performed for 2.5 and 13.3 % of lumpectomy and mastectomy patients, respectively (Fig. 2). The vast majority of those who underwent ALND after SLNB had ALND performed at the time of SLNB (96.5 % of lumpectomy patients and 94.4 % of mastectomy patients). Axillary lymph node dissection alone was performed at the time of initial surgery for 2.9 % of lumpectomy patients and 11.0 % of mastectomy patients.
Predictors of SLNB for Lumpectomy and Mastectomy Patients, 2012–2013
Predictors of SLNB performance for patients with a diagnosis of DCIS in 2012–2013 were examined (Table 2). The major notable differences between lumpectomy and mastectomy patients were insurance status and facility factors. More regional variation for SLNB was found among lumpectomy patients than among mastectomy patients. Patients cared for at academic/research institutions were less likely to undergo SLNB with lumpectomy and more likely to undergo SLNB with mastectomy. Patients in both groups with grade 3 tumors and ER-negative tumors were more likely to undergo SLNB. Larger tumor size was not predictive of SLNB use for lumpectomy patients.
Next, we selected patients who underwent only one operative procedure to exclude those who may have returned to the operating room for SLNB after invasive disease was found at the first excision. Multivariate analysis demonstrated that tumor sizes of 1.1–4.0 cm (odds ratio [OR], 1.21; 95 % confidence interval [CI] 1.14–1.30) and tumors larger than 4 cm (OR, 1.39; 95 % CI 1.16–1.66) were predictive of SLNB for lumpectomy patients treated with only one operative procedure. We examined the subset of lumpectomy patients with higher risk features (size > 5 cm or high-grade or ER-negative tumor) to determine whether their rate of SLNB differed from that of the larger cohort. The SLNB rate for patients with ER-negative tumors (28.9 %), tumors larger than 5 cm (25.0 %), or grade 3 tumors (24.4 %) (exclusive of the other high-risk features) was greater than that for the overall population (19.0 %).
Tumor Upstage Rates for DCIS Patients Undergoing SLNB or No Axillary Surgery, 2012–2013
For the patients who underwent AS in 2012–2013, the final pathologic T stage was upstaged from Tis or T0 for 22.8 % of lumpectomy patients and 18.7 % of mastectomy patients (Fig. 2). Among those who did not undergo AS, 1.8 % of lumpectomy patients and 3.6 % of mastectomy patients were upstaged. Following AS, 4.4 % of patients were upstaged to T1mi, 7.1 % were T1a, and 8.7 % had a final stage of T1b or greater. After SLNB not followed by ALND, 2.0 % of lumpectomy patients and 3.4 % of mastectomy patients had tumor-positive axillary lymph nodes, of which 21.7 % were micrometastases and 59.1 % were isolated tumor cells (ITCs).
For the patients who underwent SLNB followed by ALND, the final pathologic T stage was upstaged for 27.8 % of lumpectomy patients and 26.7 % of mastectomy patients. Tumor-positive axillary lymph nodes were found in 5.1 % of lumpectomy patients and 13.2 % of mastectomy patients, of which 41.4 % had one positive node and 17.3 % had two positive nodes. When patients treated with more than one operative procedure were excluded, the rates of upstaging remained similar for lumpectomy and mastectomy: respectively 18.9 and 17.6 % after SLNB alone, 23.6 and 26.6 % for SLNB followed by ALND; and 2.0 and 5.0 % for patients who did not undergo AS.
Predictors of T Stage Upstaging for Patients with DCIS, 2012–2013
To determine whether predictors for performance of SLNB were the same as those for tumor upstaging, we examined factors associated with upstaging for patients undergoing lumpectomy and mastectomy in 2012–2013 (Table 3). Patients treated at academic/research institutions were more likely to be upstaged, although the differences were small. The only tumor factor predictive of upstaging was ER status, with ER-negative tumors three times more likely to be upstaged than ER-positive tumors (OR, 2.99; 95 % CI 2.76–3.24). Tumor size and grade were not associated with tumor upstaging, and patients with grade 3 tumors actually were less likely to be upstaged. The analysis was repeated excluding patients who underwent more than one operative procedure, and also separately excluding size as a variable to avoid potential differences between clinical and pathologic T stage. ER-negative status remained the only tumor factor predictive of tumor upstaging in all models.
Discussion
Using the largest national dataset of incident breast cancers, we found that 63.5 % of mastectomy patients and 19.0 % of lumpectomy patients with DCIS underwent SLNB in 2012–2013. These rates are nearly identical to those from a SEER analysis in 2010,17 although that study used the number of lymph nodes examined as a surrogate for SLNB instead of the scope of regional lymph node surgery variable, which reflects the intent of the axillary procedure. Use of SLNB with mastectomy is high in accordance with NCCN and ASCO guidelines, and has stabilized in recent years. Predictors of SLNB use for mastectomy patients included treatment at an academic/research program or high-volume center, although substantial differences by region reflect facility and geographic variability in adherence to the guidelines. Although most mastectomy patients undergo SLNB, approximately 11 % are still treated with upfront ALND despite a clinical diagnosis of DCIS. The reasons for this finding are unclear and may be linked to clinical suspicion of invasive disease, which the NCDB does not capture.
Nearly one fifth of lumpectomy patients undergo SLNB, which seems disproportionately high given the guidelines for SLNB with lumpectomy. However, tumor upstage rates were significantly higher in the group of lumpectomy patients undergoing AS (22.8 %) than in the group that had no nodes removed (1.8 %). This suggests that surgeons predict fairly well which patients will be upstaged and thus who will need an SLNB. However, predictors of SLNB performance and tumor upstaging in our study differed from each other and from those in prior studies.4,8,10,22–28 In our study, the only factor predictive of tumor upstaging was ER-negative status. Two previous studies found a correlation between ER-negative tumors and upstaging from DCIS to invasive cancer.29,30 High grade and ER negativity were predictive of SLNB with lumpectomy in our cohort. Additionally, 30 % of patients with ER-negative disease alone and 25 % of patients with grade 3 disease alone underwent SLNB. Conversely, grade 3 tumors were less likely to be upstaged. Tumor size was not predictive of upstaging or SLNB, possibly because the NCDB does not contain clinical tumor size, and a discrepancy may exist between size on imaging or exam and size of the final pathologic specimen. However, when we excluded patients who underwent more than one operative procedure, larger tumor size was predictive of SLNB. In addition, ALND independent of SLNB was performed for approximately 3 % of lumpectomy patients in our study, which seems high given their clinical stage of DCIS and suggests that other clinical factors such as findings on imaging or exam may have influenced a surgeon to perform ALND. Finally, we found substantial regional variation in practice, with some areas of the country demonstrating more than two times greater likelihood of SLNB performance with lumpectomy.
Our ability to demonstrate compliance with clinical guidelines for SLNB in DCIS patients is limited as the NCDB does not contain several factors in the NCCN and ASCO guidelines, namely, imaging findings, palpability, and tumor location. In 20 % of patients, DCIS presents as a palpable mass, and both palpability and mammographic mass have been associated with upstaging (rates of 54.1 and 35.6 %, respectively).4,31 Although we could not exclude patients who had DCIS with “suspicion for microinvasion,” those with microinvasion on initial diagnostic biopsy are coded as cT1mic in the NCDB and were not included in this study. As in many large retrospective database studies, we were not able to collect information prospectively on factors that may influence performance of SLNB or tumor upstaging. The NCDB lacks information on the size and type of biopsy needle used, the number of biopsy samples, and comedo-necrosis, additional features associated with upstaging of DCIS.12,32–35 However, comparing our findings with the criteria in the NCCN and ASCO guidelines, ER status and grade are notable features missing from current recommendations. In our study, ER negativity was associated with both tumor upstaging and SLNB, and perhaps should be considered in future guidelines as an additional indication for SLNB in the treatment of lumpectomy patients with DCIS.
In summary, we demonstrated that the use of SLNB is high with mastectomy, matching recommendations in clinical guidelines. The SLNB rates for lumpectomy patients appear to be high but correlate well with tumor upstaging, suggesting that its use is not inappropriate in this setting. Although ER status plays a large role in predicting SLNB use and in upstaging tumors, it is not included in current guidelines and deserves further study. The low rate of nodal positivity reinforces the need to avoid ALND for patients undergoing lumpectomy for DCIS. The variable use of SLNB for DCIS highlights an opportunity to study clinical outcomes that will further inform recommendations regarding the utility of SLNB and ALND for patients with DCIS.
References
Lyman GH, Giuliano AE, Somerfield MR, et al. American Society of Clinical Oncology clinical practice guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol. 2005;23:7703–20.
Lyman GH, Temin S, Edge SB, et al. Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2014;32:1365–83.
National Comprehensive Cancer Network (2016). National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology: Breast Cancer Version 1.2016. Retrieved 28 March 2016 at www.nccn.org.
Brennan ME, Turner RM, Ciatto S, Marinovich ML, French JR, Macaskill P, et al. Ductal carcinoma in situ at core-needle biopsy: meta-analysis of underestimation and predictors of invasive breast cancer. Radiology. 2011;260:119–28.
Zavotsky J, Hansen N, Brennan MB, Turner RR, Giuliano AE. Lymph node metastasis from ductal carcinoma in situ with microinvasion. Cancer. 1999;85:2439–43.
Klauber-DeMore N, Tan LK, Liberman L, et al. Sentinel lymph node biopsy: is it indicated in patients with high-risk ductal carcinoma in situ and ductal carcinoma in situ with microinvasion? Ann Surg Oncol. 2000;7:636–42.
Cox CE, Nguyen K, Gray RJ, et al. Importance of lymphatic mapping in ductal carcinoma in situ (DCIS): why map DCIS? Am Surg. 2000;67:513–9.
Wilkie C, White L, Dupont E, Cantor A, Cox CE. An update of sentinel lymph node mapping in patients with ductal carcinoma in situ. Am J Surg. 2005;190:563–6.
Ansari B, Ogston SA, Purdie CA, Adamson DJ, Brown DC, Thompson AM. Meta-analysis of sentinel node biopsy in ductal carcinoma in situ of the breast. Br J Surg. 2008;95:547–54.
Yi M, Krishnamurthy S, Kuerer HM, et al. Role of primary tumor characteristics in predicting positive sentinel lymph nodes in patients with ductal carcinoma in situ or microinvasive breast cancer. Am J Surg. 2008;196:81–7.
Sun X, Li H, Liu YB, et al. Sentinel lymph node biopsy in patients with breast ductal carcinoma in situ: Chinese experiences. Oncol Lett. 2015;10:1932–8.
Park HS, Park S, Cho J, et al. Risk predictors of underestimation and the need for sentinel node biopsy in patients diagnosed with ductal carcinoma in situ by preoperative needle biopsy. J Surg Oncol. 2013;107:388–92.
Moore KH, Sweeney KJ, Wilson ME, et al. Outcomes for women with ductal carcinoma in situ and a positive sentinel node: a multi-institutional audit. Ann Surg Oncol. 2007;14:2911–7.
Prendeville S, Ryan C, Feeley L, O’Connell F, Browne TJ, O’Sullivan MJ, Bennett MW. Sentinel lymph node biopsy is not warranted following a core needle biopsy diagnosis of ductal carcinoma in situ (DCIS) of the breast. Breast. 2015;24:197–200.
Namm JP, Mueller J, Kocherginsky M, Kulkarni S. The utility of sentinel lymph node biopsy in patients with ductal carcinoma in situ suspicious for microinvasion on core biopsy. Ann Surg Oncol. 2015;22:59–65.
Francis AM, Haugen CE, Grimes LM, et al. Is sentinel lymph node dissection warranted for patients with a diagnosis of ductal carcinoma in situ? Ann Surg Oncol. 2015;22:4270–9.
Worni M, Akushevich I, Greenup R, D, Ryser MD, Myers ER, Hwang ES. Trends in treatment patterns and outcomes for ductal carcinoma in situ. J Natl Cancer Inst. 2015;107:djv263.
National Cancer Data Base. Data Dictionary PUF 2013: Surgery of the Primary Site Codes, Breast. Retrieved 28 March 2016 at http://ncdbpuf.facs.org/content/breast, 2009.
National Cancer Data Base. Data Dictionary PUF 2013: Scope of Regional LN Surgery 2012. Retrieved 28 March 2016 at: http://ncdbpuf.facs.org/node/417, 2015.
United States Census Bureau. Census Bureau Regions and Divisions with State FIPS Codes. Retrieved 28 March 2016 at http://www2.census.gov/geo/docs/maps-data/maps/reg_div.txt, 2015.
National Accreditation Program of Breast Centers. NAPBC Standards Manual 2014 Edition, American College of Surgeons, 2014.
Goyal A, Douglas-Jones A, Monypenny I, Sweetland H, Stevens G, Mansel RE. Is there a role of sentinel lymph node biopsy in ductal carcinoma in situ? Analysis of 587 cases. Breast Cancer Res Treat. 2006;98:311–4.
Mittendorf EA, Arciero CA, Gutchell V, Hooke J, Shriver CD. Core biopsy diagnosis of ductal carcinoma in situ: an indication for sentinel lymph node biopsy. Curr Surg. 2005;62:253–7.
Yen TW, Hunt KK, Ross MI, et al. Predictors of invasive breast cancer in patients with an initial diagnosis of ductal carcinoma in situ: a guide to selective use of sentinel lymph node biopsy in management of ductal carcinoma in situ. J Am Coll Surg. 2005;200:516–26.
Lee CH, Carter D, Philpotts LE, Couce ME, Horvath LJ, Lange RC, et al. Ductal carcinoma in situ diagnosed with stereotactic core needle biopsy: can invasion be predicted? Radiology. 2000;217:466–70.
Guillot E, Vaysse C, Goetgeluck J, et al. Extensive pure ductal carcinoma in situ of the breast: identification of predictors of associated infiltrating carcinoma and lymph node metastasis before immediate reconstructive surgery. Breast. 2014;23:97–103.
Huo L, Sneige N, Hunt KK, Albarracin CT, Lopez A, Resetkova E. Predictors of invasion in patients with core-needle biopsy-diagnosed ductal carcinoma in situ and recommendations for a selective approach to sentinel lymph node biopsy in ductal carcinoma in situ. Cancer. 2006;107:1760–8.
Hoorntje LE, Schipper ME, Peeters PH, Bellot F, Storm RK, Borel Rinkes IH. The finding of invasive cancer after a preoperative diagnosis of ductal carcinoma in situ: causes of ductal carcinoma in situ underestimates with stereotactic 14-gauge needle biopsy. Ann Surg Oncol. 2003;10:748–53.
Lee SK, Yang JH, Woo SY, Lee JE, Nam SJ. Nomogram for predicting invasion in patients with a preoperative diagnosis of ductal carcinoma in situ of the breast. Br J Surg. 2013;100:1756–63.
Sato Y, Kinoshita T, Suzuki J, et al. Preoperatively diagnosed ductal carcinoma in situ: risk prediction of invasion and effects on axillary management. Breast Cancer 2015. doi:10.1007/s12282-015-0636-5.
Barnes NL, Dimopoulos N, Williams KE, Howe M, Bundred NJ. The frequency of presentation and clinico-pathological characteristics of symptomatic versus screen-detected ductal carcinoma in situ of the breast. Eur J Surg Oncol. 2014;40:249–54.
Rutstein LA, Johnson RR, Poller WR, et al. Predictors of residual invasive disease after core needle biopsy diagnosis of ductal carcinoma in situ. Breast J. 2007;13:251–7.
Renshaw AA. Predicting invasion in the excision specimen from breast core-needle biopsy specimens with only ductal carcinoma in situ. Arch Pathol Lab Med. 2002;126:39–41.
Jackman RJ, Burbank F, Parker SH, et al. Stereotactic breast biopsy of nonpalpable lesions: determinants of ductal carcinoma in situ underestimation rates. Radiology. 2001;218:497–502.
Houssami N, Ambrogetti D, Marinovich ML, et al. Accuracy of a preoperative model for predicting invasive breast cancer in women with ductal carcinoma in situ on vacuum-assisted core-needle biopsy. Ann Surg Oncol. 2011;18:1364–71.
Disclosures
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miller, M.E., Kyrillos, A., Yao, K. et al. Utilization of Axillary Surgery for Patients With Ductal Carcinoma In Situ: A Report From the National Cancer Data Base. Ann Surg Oncol 23, 3337–3346 (2016). https://doi.org/10.1245/s10434-016-5322-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5322-0