Abstract
Background
Esophageal cancer has a poor prognosis, and many patients undergoing surgery have a low chance of cure. Imaging studies suggest that tumor volume is prognostic. The study aimed to evaluate pathological tumor volume (PTV) as a prognostic variable in esophageal cancer.
Methods
This single-center cohort study included 283 patients who underwent esophageal cancer resections between 2000 and 2012. PTVs were obtained from pathological measurements using a validated volume formula. The prognostic value of PTV was analyzed using multivariable regression models, adjusting for age, tumor grade, tumor (T) stage, nodal stage, lymphovascular invasion, resection margin, resection type, and chemotherapy response, which provided hazard ratios (HRs) with 95 % confidence intervals (CIs). Primary outcomes were time to death and time to recurrence. Secondary outcomes were margin involvement and lymph node positivity. Correlation analysis was performed between imaging and PTVs.
Results
On unadjusted analysis, increasing PTV was associated with worse overall mortality (HR 2.30, 95 % CI 1.41–3.73) and disease recurrence (HR 1.87, 95 % CI 1.14–3.07). Adjusted analysis demonstrated worse overall mortality with increasing PTV but reached significance in only one subgroup (HR 1.70, 95 % CI 1.09–2.38). PTV was an independent predictor of margin involvement (OR 2.28, 95 % CI 1.02–5.13) and lymph node–positive status (OR 2.77, 95 % CI 1.23–6.28). Correlation analyses demonstrated significant positive correlation between computed tomography (CT) software and formula tumor volumes (r = 0.927, p < 0.0001), CT and positron emission tomography tumor volumes (r = 0.547, p < 0.0001), and CT and PTVs (r = 0.310, p < 0.001).
Conclusions
Tumor volume may predict survival, margin status, and lymph node positivity after surgery for esophageal cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Esophageal cancer is an aggressive disease, and the majority of patients present with advanced malignancy that precludes surgical resection.1 , 2Curative treatment in the United Kingdom is predominantly, but not exclusively, chemotherapy followed by surgery. Prognosis and management are often guided by tumor stage at diagnosis, but emerging evidence suggests that tumor stage after chemotherapy may be more important prognostically than that at initial presentation.3 , 4
Improvements in imaging technology have generated interest in alternative parameters that may improve outcome prediction. Tumor volume is one such parameter. This logic is based on the hypothesis that larger tumors have an increased probability of lymph node and systemic metastases, as well as higher rates of incomplete surgical resection.5 Tumor volume may also play a role in the assessment of tumor response to neoadjuvant chemotherapy.6 , 7 Some studies have found tumor volume to be a prognostic indicator in esophageal cancer.8 , 9 The focus of research to date has been on the prognostic role of imaging-assessed tumor volume. Studies have concluded that tumor volume, predominantly assessed by positron emission tomography (PET)/computed tomography (CT), is a significant survival indicator. However, it is unclear if tumor volume assessed by such imaging modalities accurately reflects pathological tumor volume (PTV).10 , 11
PTV, assessed after surgical resection, remains the gold standard with regard to definitive tumor volume assessment. If PTV measurement is not associated with any clinically useful outcome measures, then it would seem unnecessary to pursue research into imaging tumor volumes. We therefore evaluated PTV in relation to the outcome measures time to death, time to recurrence, margin status, and lymph node metastasis and correlated PTV with imaging-assessed tumor volumes.
Methods
Design
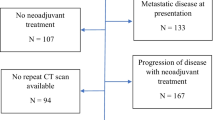
This cohort study was based on a prospectively collected database of 624 consecutive resections for esophageal or gastroesophageal junction tumors (Siewert type 1 and 2). These were performed in a single center (St. Thomas’ Hospital, London) between 2000 and 2012 with follow-up until February 2014, which has been described in detail elsewhere.3 Patients who died within 30 days of surgery (n = 5), for whom tumor histology was not squamous, adenosquamous, adenocarcinoma, or high-grade dysplasia (n = 11), and who had Siewert type 3 tumors (n = 10) or incomplete tumor dimension data (n = 315) were excluded. Thereafter, 283 patients (45 %) remained for the present study. All patients were managed by an upper gastrointestinal cancer multidisciplinary team. Staging investigations included esophagogastroduodenoscopy, CT, endoscopic ultrasound, and, since 2007,18 F-fluorodeoxyglucose PET. Neoadjuvant chemotherapy regimens evolved during the study period. Combination regimens were either cisplatin and 5-fluorouracil or epirubicin, cisplatin, and either 5-fluorouracil or capecitabine. Patients receiving chemotherapy underwent a restaging CT scan before surgery. Surgical resection was either via a transhiatal or 2-stage esophagectomy performed by 1 of 3 surgeons within the center. After surgery, definitive pathological results provided a PTV. Staging was standardized using the 7th edition of the Union for International Cancer Control Classification and Malignant Tumors tumor, node, metastasis classification system (TNM).12 Survival was recorded as the date of surgery to the last verified hospital or general practice attendance, or date of death. Tumor recurrence required radiologic or histologic disease confirmation as agreed by the cancer multidisciplinary team. Ethics permission was granted for use of the database.
Study Exposure
PTV was calculated from tumor dimensions documented in histopathology reports using the following validated formula: v = (ab)π/6, where v = volume, a = maximum tumor length, and b = maximum tumor width.13 , 14 At initial pathological assessment, gross tumor size was recorded and, in the presence of a significant response to chemotherapy, dimensions were adjusted to account for fibrosis. Mandard tumor regression grade was also recorded.
CT tumor volumes were analyzed using open-source, Mac-based DICOM Viewer (OsiriX 3.9) software.15 Volumes were calculated using both CT volume software and the validated formula, using longest axial and craniocaudal tumor dimensions.
PET tumor volumes were obtained from in-house software using a technique aligning PET and CT scans to obtain a region of interest, which was subsequently analyzed using a Feature Analysis Software Tool with tumor volume calculated according to standardized uptake value threshold calculations of 40 %.
Outcome Measures
The primary outcome measures were time to death and time to recurrence, assessed from the date of surgery to the date of death or recurrence, respectively. Secondary outcomes were lymph node positivity and positive resection margin status (R1 resection), assessed from histopathologic evaluation. R1 resection included longitudinal and circumferential resection margin involvement, defined as tumor at or within 1 mm of the margin.16
Statistical Analysis
Crude and multivariable analyses were performed using a Cox’s proportional hazard model for primary outcomes and logistic regression for secondary outcomes. These provided hazard ratios (HRs) and odds ratios (ORs) respectively, with 95 % confidence intervals (CIs). Variables included in the adjusted analysis of time to death and time to recurrence included age, pathological tumor grade (in 3 groups: complete pathological resolution; high grade dysplasia; well differentiated, moderately differentiated, or poorly differentiated), pathological tumor (T) stage (in 2 categories: T0/1/2 or T3/4), pathological nodal stage (in 4 categories: N0, 1, 2, 3), lymphovascular invasion (positive or negative), resection margin (R0 or R1), resection type (transhiatal esophagectomy or 2 stage), pathological response to chemotherapy (in 6 categories: complete pathological response, good response, moderate response, poor response, no response, no chemotherapy) and PTV (divided into quartiles with a further group of PTV 0 cm3, totaling 5 categories: PTV1 [0 cm3], PTV2 [>0–4.7 cm3], PTV3 [>4.7–11.8 cm3 ], PTV4 [>11.8–28.8 cm3], or PTV5 [>28.8–167.6 cm3]).
Variables included in the adjusted analysis of margin involvement included tumor (T) stage and resection type. Variables included for lymph node positivity were tumor (T) stage, tumor grade, resection type, and lymphovascular invasion. Adjusted analyses of these outcomes were also stratified by tumor (T) stage (T1/2 vs. T3/4).
Correlation between CT, PET, and PTVs was assessed by Pearson’s correlation coefficients.
All statistical analyses were performed by SAS 9.4 software (SAS Institute, Cary, NC, USA).
Results
Patients
Demographic and clinical characteristics of the 283 included patients are presented in Table 1. The majority were male (84 %); median age was 64 (range 58–82) years, and 201 (71 %) underwent neoadjuvant chemotherapy. Resected tumors were predominantly located at the gastroesophageal junction (76 %) and were adenocarcinomas (79 %). PTVs ranged 0–167.6 cm3. Twenty-seven patients had a PTV of 0 cm3, 25 had high-grade dysplasia/complete pathological resolution and 28 were tumor (T) stage 0. The discrepancy between these figures is as a consequence of 2 patients with carcinoma-in situ and 1 with node-positive disease despite no residual primary tumor after chemotherapy. During follow-up, 146 (52 %) patients died, and 132 patients (47 %) had disease recurrence, with a median recurrence time of 12.2 (range 1.4–59.3) months.
PTV in Relation to Time to Death and Time to Recurrence
On crude analysis, both PTV (HR 2.30, 95 % CI 1.41–3.73 and HR 1.87, 95 % CI 1.14–3.07) and tumor (T) stage (HR 2.55, 95 % CI 1.83–3.55 and HR 3.06, 95 % CI 2.15–4.36) were strong predictors of overall mortality and disease recurrence, respectively (Figs. 1, 2; Table 2).
On multivariable analysis, higher HRs were seen with increasing PTV; this reached statistical significance, in relation to overall mortality, in one of the subgroups (HR 1.70, 95 % CI 1.09–2.38) (Table 2). Pathological tumor (T) stage (HR 1.60, 95 % CI 1.09–2.38), N stage (HR 2.15, 95 % CI 1.28–3.62), lymphovascular invasion (HR 1.54, 95 % CI 1.04–2.26), and poorly differentiated tumors (HR 1.54, 95 % CI 1.06–2.22) were other significant predictors of worse overall mortality. These results were replicated when the surgery alone, and chemotherapy and surgery groups were analyzed separately (data not shown).
Regarding disease recurrence, PTV was not statistically significant in multivariable analysis (HR 1.15, 95 % CI 0.67–1.97), whereas pathological tumor (T) stage (HR 1.68, 95 % CI 1.12–2.53) and N stage (HR 2.04, 95 % CI 1.19–3.51) were (Table 2).
PTV in Relation to Margin Involvement and Lymph Node Positivity
On unadjusted analysis, a significant, albeit non-linear, association was demonstrated between increasing PTV and both R1 resection (HR 4.50, 95 % CI 2.13–9.48) and positive nodal status (HR 2.72, 95 % CI 1.31–5.62) (Table 3).
On multivariable analysis, PTV demonstrated significance in 2 subgroups, PTV 4 (HR 4.10 95 % CI 1.80–9.33) and PTV 5 (HR 2.28, 95 % CI 1.02–5.13), and a non-significant association was found with an R1 resection in the remaining group, PTV 3 (HR 1.34, 95 % CI 0.59–3.07). When stratified by tumor (T) stage, PTV demonstrated significance in both subgroups for an R1 resection (T1/2: HR 4.24, 95 % CI 1.34–13.48 and T3/4: HR 7.10, 95 % CI 2.02–25.06). Pathological tumor (T) stage (HR 6.34, 95 % CI 3.56–11.51) was also a significant predictor of an R1 resection.
PTV (HR 2.77, 95 % CI 1.23–6.28), pathological tumor (T) stage (HR 1.81, 95 % CI 1.01–3.23), and lymphovascular invasion (HR 2.42, 95 % CI 1.35–4.36) were significant independent predictors of positive lymph nodal status. After stratifying by tumor (T) stage, there was a non-significant trend between increasing PTV and node-positive status for both T1/2 and T3/4 tumors (HR 2.17 and 3.11, respectively). A similar but non-significant trend was demonstrated with increasing tumor grade and node positive status. Lymphovascular invasion was a significant predictor of positive nodal status in T3/4 tumors alone (HR 4.21, 95 % CI 1.65–10.74).
Imaging-Assessed Tumor Volumes and Correlation Analyses
Of the 283 patients with PTVs, 123 had staging CT tumor volumes, 115 staging PET tumor volumes, and 68 had restaging CT tumor volumes after neoadjuvant chemotherapy.
Correlation analysis of 231 tumor volumes, measured by both CT volume software and by a validated formula, demonstrated a significant strong positive linear correlation (r = 0.927, p < 0.0001).
For 115 patients with both diagnostic staging CT and PET scans, correlation analysis demonstrated a significant positive linear correlation (r = 0.547, p < 0.0001). Correlation analysis of 68 restaging CT tumor volumes and PTVs demonstrated a significant moderately positive linear correlation (r = 0.310, p < 0.001).
Discussion
Results from this study indicate that larger PTVs may predict survival, margin involvement, and lymph node positivity in esophageal cancer, irrespective of tumor (T) stage. However, not all subgroups reached significance in the multivariable model, suggesting that numerous parameters contribute to prognosis, some of which may have strong interrelations.
Some aspects of methodology merit further discussion. This was a comparatively large study, in terms of patient numbers, from a prospectively maintained database with mature follow-up data. Nevertheless, the statistical power was limited, and statistically negative associations with substantially increased point HRs should be interpreted cautiously. Patients underwent either a transhiatal or transthoracic esophagectomy. Although radicality of resection, specifically lymphadenectomy, may differ between approaches, studies, including this one, have consistently demonstrated no survival difference.17 , 18 Adjusting for surgical approach did not affect the influence of tumor volume or our outcome measures. Furthermore, it is unlikely that surgical approach per se would alter the recorded PTV.
A number of patients, with incomplete tumor dimensions, were excluded from the initial cohort. Although this reduced patient numbers, the retrospective nature of the study meant that their omission did not introduce data bias. It did, however, highlight the need for consistency in pathology reporting, much of which has improved over the study duration. For patients with complete tumor dimensions, a validated conical formula was used to assess PTVs. This formula was further validated by the strong positive correlation between formula and software CT tumor volumes seen in this study. However, it was unable to adjust for non-uniform tumor dimensions and made assessment of multifocal tumors complex. A degree of post resection and post fixation esophageal shrinkage also occurs.19 Although we were unable to mitigate for this, all specimens underwent an identical preparation process using formalin fixation. Whilst this may affect absolute PTV measurement, it should not have affected the study results, as specimen shrinkage should be proportional, and positive linear relations on correlation analyses are unaffected by scale. Nonetheless, we acknowledge that tumor volumes are not absolute but rather are the most accurate approximation possible within the confines of the study.
To our knowledge, this study is the first to assess the relation between PTV and mortality in esophageal cancer and to correlate imaging and PTVs. Imaging-assessed tumor volume has previously been studied in a prognostic capacity and also to quantify response to neoadjuvant chemotherapy. A study of PET parameters, including metabolic tumor volume, in esophageal carcinoma patients demonstrated a significant prognostic role for tumor volume.8 This study differed from ours in that the majority of tumors (96 %) were squamous cell carcinomas. Further studies from the United Kingdom, France, and the United States using PET, endoscopic ultrasound, and PET/CT tumor characteristics have consistently demonstrated imaging-assessed tumor volumes and lengths to be independent survival indicators in esophageal cancer.10 , 11 , 20 Furthermore, the demographics of these study populations, with adenocarcinoma the predominant histology, more closely reflect ours. A further study of PET/CT and pathological tumor lengths demonstrated positive correlation between variables, indicating, like our study, that imaging-assessed parameters appear to reflect their pathological counterparts.21
Although imaging tumor volume may be a significant prognostic indicator, PTV remains the gold standard with regard to definitive tumor volume measurement. Its ability to predict prognosis is vital in assessing whether the use of a surrogate, such as imaging volume, is worthy of further investigation. Our correlation results validate imaging tumor volume as a surrogate and suggest that its further investigation is justified.
In this study, PTV mirrored the aforementioned results of imaging tumor volume, with worse survival observed in patients with larger tumor volumes. However, not all subgroups achieved statistical significance on adjusted analysis. The approach to tumor volume analysis in this study, however, differed from previous series. As a relatively unknown variable, we undertook categorical PTV analysis, prospectively dividing it into quartiles and comparing it alongside tumor (T) stage. In previous studies, threshold tumor volumes were defined retrospectively, an inherent source of bias, using 2 volume groups.9 , 11 We believe our approach to be a more robust assessment of tumor volume.
We hypothesized that larger volume tumors would have an increased likelihood of positive resection margins and nodal spread, giving rise to worse survival. In this study, nodal status was the strongest predictor of both overall mortality and disease recurrence. Of particular interest, therefore, was that PTV appeared to be associated with lymph node–positive status and involved resection margins, independent of other known confounders.
The majority of tumors considered for resection may be classified as locally advanced, i.e. T3 and lymph node positive, mandating a multimodal therapeutic approach. This poses several pertinent questions. Why are outcomes in patients with similarly staged tumors difficult to predict? Is this observed diversity purely a manifestation of tumor biology and an individual’s response to chemotherapy? Is there truly a difference between a “big” and “little” T3? Results from this study suggest that TNM staging, although important, remains a relatively crude classification which may be enhanced by supplementary prognostic parameters. The potential role for tumor volume in risk stratifying selected patients for resection margin or lymph node involvement would be of great interest. In the United Kingdom, this could directly influence management, as a patient with a higher-volume tumor at risk of margin involvement could be selected for neoadjuvant chemoradiotherapy and a 2-stage resection to mitigate this risk. Furthermore, we hypothesize that changes in tumor volume may be clinically useful as a surrogate for response to chemotherapy, therefore justifying its further study. Both of the above may conceivably be used to support the modern philosophy of individually tailored therapy.
In conclusion, this study highlights an interesting role for PTV in predicting survival, lymph node positivity, and R1 resection in esophageal malignancy. Its use would be alongside pathological tumor (T) stage and nodal stage, both confirmed as significant indicators of overall mortality and disease recurrence. These findings justify ongoing radiologic measurement of tumor volume in a research setting. Whether this may be incorporated into algorithms for personalized esophageal cancer treatment in the future remains to be seen.
References
Enzinger PC, Mayer RJ. Esophageal cancer. N Engl J Med. 2003;349:2241–52.
Wu PC, Posner MC. The role of surgery in the management of esophageal cancer. Lancet Oncol. 2003;4:481–8.
Davies AR, Gossage JA, Zylstra J, et al. Tumor stage after neoadjuvant chemotherapy determines survival after surgery for adenocarcinoma of the esophagus and esophagogastric junction. J Clin Oncol. 2014;32:2983–90.
Davies AR, Pillai A, Sinha P, et al. Factors associated with early recurrence and death after esophagectomy for cancer. J Surg Oncol. 2014;109:459–64.
Lagarde SM, ten Kate FJ, Reitsma JB, Busch OR, van Lanschot JJ. Prognostic factors in adenocarcinoma of the esophagus or gastroesophageal junction. J Clin Oncol. 2006;24:4347–55.
Sloof G. Response monitoring of neoadjuvant therapy using CT, EUS and FDG-PET. Best Pract Res Clin Gastroenterol. 2006;20:941–57.
Blom RLGM, Steenbakkers IR, Lammering G, et al. PET/CT-based metabolic tumor volume for response prediction of neoadjuvant chemoradiotherapy in esophageal cancer. Eur J Nucl Med Mol Imaging. 2013;40:1500–6.
Hyun SH, Choi JY, Shim YM, et al. Prognostic value of metabolic tumor volume measured by 18F-fluorodeoxyglucose positron emission tomography in patients with esophageal carcinoma. Ann Surg Oncol. 2010;17:115–22.
Crehange G, Bosset M, Lorchel F, et al. Tumor volume as outcome determinant in patients treated with chemoradiation for locally advanced esophageal cancer. Am J Clin Oncol. 2006;29:583–7.
Hatt M, Visvikis D, Albarghach NM, Tixier F, Pradier O, Cheze-le RC. Prognostic value of (18)F-FDG PET image-based parameters in esophageal cancer and impact of tumor delineation methodology. Eur J Nucl Med Mol Imaging. 2011;38:1191–202.
Chan DSY, Fielding P, Roberts SA, Reid TD, Ellis-Owen R, Lewis WG. Prognostic significance of 18-FDG PET/CT and EUS defined tumor characteristics in patients with esophageal cancer. Clin Radiol. 2013. 68:352–7.
Wittekind C, Yamasaki S. Digestive system tumours—oesophagus including oesophagogastric junction. In: Sobin LH, Gospodarowicz MK, Wittekind CW, editors TNM classification of malignant tumours. 7th ed. New York: Wiley-Blackwell; 2009:66.
Schwartz M. A biomathematical approach to clinical tumor growth. Cancer. 1961;14:1272–94.
Hasegawa M, Sone S, Takashima S, et al. Growth rate of small lung cancers detected on mass CT screening. Br J Radiol. 2000;73(876):1252–9.
Roset A, Spadola L, Ratib O. OsiriX: an open-source software for navigating in multidimensional DICOM images. J Digit Imaging. 2004;17:205–16.
Mapstone NP. Dataset for the histopathological reporting of esophageal carcinoma. 2nd Edition. Royal College of Pathologists G006. 2007. https://www.rcpath.org/Resources/RCPath/Migrated%20Resources/Documents/G/G006OesophagealdatasetFINALFeb07.pdf. Accessed 22 Jan 2015.
Davies AR, Sandhu H, Pillai A, et al. Surgical resection strategy and the influence of radicality on outcomes in oesophageal cancer. Br J Surg. 2014;101:511–7.
Omloo JM, Lagarde SM, Hulscher JB, et al. Extended thoracic resection compared with limited transhiatal resection for adenocarcinoma of the mid/distal oesophagus: five year survival of a randomized clinical trial. Ann Surg. 2007;246:992–1000.
Siu KF, Cheung HC, Wong J. Shrinkage of the esophagus after resection for carcinoma. Ann Surg. 1986;203:173–6.
Boggs DH, Hanna A, Burrows W, Horiba N, Suntharalingham N. Primary gross tumor volume is an important prognostic factor in locally advanced esophageal cancer patients treated with trimodality therapy. J Gastrointest Cancer. 2015;46:131–7.
Jeganathan R, McGuigan J, Campbell F, Lynch T. Does pre-operative estimation of esophageal tumor metabolic length using 18F-fluorodeoxyglucose PET/CT images compare with surgical pathology length? Eur J Nucl Med Mol Imaging. 2011;38:656–62.
Acknowledgment
This research was undertaken as an ESSQ MSc thesis (L.G.C.T.).
Disclosure
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
For the Guy’s St. Thomas’ Oesophago-Gastric Research Group.
Rights and permissions
About this article
Cite this article
Tullie, L.G.C., Sohn, HM., Zylstra, J. et al. A Role for Tumor Volume Assessment in Resectable Esophageal Cancer. Ann Surg Oncol 23, 3063–3070 (2016). https://doi.org/10.1245/s10434-016-5228-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5228-x