Abstract
Background
National guidelines endorse adjuvant chemotherapy ± radiotherapy (C ± RT) for early-stage gastric cancer (ESGC). Compliance with these guidelines and the specific impact of adjuvant C ± RT on overall survival (OS) in ESGC have not been extensively explored.
Methods
The National Cancer Data Base was queried for stage IB-II gastric adenocarcinoma patients undergoing gastrectomy (1998–2011). Multivariable modeling identified factors associated with adjuvant C ± RT receipt and compared risk-adjusted OS by treatment type (i.e., adjuvant therapy versus surgery alone).
Results
Of 23,461 ESGC patients (1998–2011), 79.4 % and 20.6 % received surgery alone and adjuvant C ± RT (chemoradiotherapy 17.7 %; chemotherapy alone 2.9 %), respectively. Predictors of adjuvant C ± RT receipt included age <67 years, pathologic nodal positivity, and adequate lymph node staging (LNS; ≥15 nodes examined; all p < 0.001). Survival analyses included 15,748 patients (1998–2006); median, 1-, and 5-year survival were 63.5 months, 86.0 %, and 27.0 % respectively. Omission of adjuvant C ± RT conferred an increased hazard of risk-adjusted mortality in the overall cohort, and stage IB and II subgroups (all p ≤ 0.001). The benefit of adjuvant C ± RT was most pronounced in stage II and node-positive patients—regardless of LNS adequacy (all p < 0.001)—and inadequately staged IB patients (p = 0.003). While associated with a trend toward improved OS in node-negative patients overall (p = 0.051), adjuvant C ± RT did not improve OS if surgical LNS was adequate in this subgroup (p = 0.960).
Conclusions
Adoption of adjuvant C ± RT in ESGC remains incomplete nationally. Receipt of adjuvant therapy is associated with improved risk-adjusted survival relative to surgery alone; however, in adequately staged patients without lymph node metastasis, this benefit is less certain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An estimated 10,720 disease-specific deaths will be attributed to gastric cancer in the United States in 2015.1 While margin-negative surgical resection remains the dominant contributor to survival, poor long-term outcomes with surgical resection alone have compelled a multimodality approach to this disease.2 In 2001, the randomized, phase III, Intergroup-0116 trial demonstrated a disease-specific and overall survival benefit for adjuvant 5-fluorouracil (FU)-based chemoradiotherapy compared with surgery alone for stage IB-IV M0 disease.3 In 2006, the UK-based MAGIC trial demonstrated a similar advantage for perioperative chemotherapy (ECF: epirubicin, cisplatin, 5-FU) compared with surgery alone in stage II-III disease.4 Subsequently, several retrospective analyses have affirmed improved survival with a multimodality approach, particularly in locally advanced disease.5–8 Accordingly, current national guidelines advocate the use of a multimodality approach in resectable gastric cancer, comprising curative-intent surgical resection with either neoadjuvant or adjuvant therapy.9
Use of multimodality therapy is not only recommended for locally advanced (i.e., stage III or IV M0) disease but also has been endorsed for the treatment for early-stage gastric cancer (ESGC; i.e., stage IB-II).9 In clinical practice, ESGC patients are more likely to undergo surgery first, deferring the decision for adjuvant chemotherapy with or without radiotherapy (C ± RT) until after pathologic staging information is available. However, recent retrospective evidence from large population-based cancer registries suggests that omission of adjuvant therapy is frequent in eligible ESGC patients, perhaps reflecting assumptions regarding the dispensability of multimodality therapy in early disease states.7,10,11 While such assumptions have not been supported in the literature, there is, likewise, a paucity of retrospective or prospective evidence indicating a definitive benefit for adjuvant therapy in ESGC.
Drawing on a large cohort of patients with ESGC from the National Cancer Data Base (NCDB), we examined temporal trends in the administration of adjuvant C ± RT in this patient subset, factors associated with adjuvant C ± RT utilization, and the effect of adjuvant therapy receipt on overall survival (OS).
Methods
Data Source
After institutional review board approval, data from 1998 to 2011 were acquired from the esophagogastric participant use file of the NCDB, a collaborative effort between the American Cancer Society and American College of Surgeons’ Commission on Cancer (CoC). Established in 1989, the NCDB is a comprehensive oncology surveillance program that captures approximately 70 % of new cancer diagnoses from >1500 CoC-approved centers. Data available in NCDB include site-specific operative codes, American Joint Committee on Cancer (AJCC) pathologic TNM staging (5th–7th editions), and multimodality treatment sequence.12
Patient Selection
Patients with early-stage—AJCC pathologic stage IB (T2N0, T1N1) and II (IIA: T1N2, T2N1, T3N0; IIB: T1N3, T2N2, T3N1, T4aN0)—invasive gastric adenocarcinoma (defined by ICD‐O‐3 topography codes C16.1–C16.9) undergoing curative-intent resection between 1998 and 2011 were selected.13 Patients who received any neoadjuvant therapy (n = 7630) were excluded from analysis because: (a) direct comparison between cohorts receiving neoadjuvant and adjuvant therapy is inherently problematic due to incongruence between clinical and pathologic staging; and (b) a small minority of ESGC patients evaluable for survival analysis received neoadjuvant therapy (6–8 % between 1998 and 2006).
Also excluded from analysis were patients who received adjuvant radiotherapy alone (n = 394), had stage III/IV/unknown stage disease (n = 109,323), did not undergo at least partial gastrectomy (n = 76,186), underwent an indeterminate lymph node (LN) harvest or examination of zero LNs (n = 82,149), underwent palliative resection (n = 1739), or died within 30 days postoperatively (n = 4097). Structured queries allowing for these exclusions yielded a study cohort of 23,461 patients. Because survival information is only abstracted 5 years following diagnosis per NCDB methodology, it was available for patients diagnosed before 2006 (n = 15,748; Fig. 1).
Patient selection flow diagram. After applying initial exclusion criteria in NCDB gastric cancer patients from 1998 to 2011, temporal trends and predictors of adjuvant therapy receipt were examined (n = 23,461). For survival analysis, patients diagnosed between 1998 and 2006 (n = 15,748) were selected. Treatment distribution (i.e., surgery alone vs. adjuvant C ± RT), stratified by stage subgroup, nodal status, and adequacy of lymph node staging are shown. C ± RT chemotherapy with or without radiotherapy, LNS lymph node staging
Variables
The demographic and clinicopathologic NCDB variables utilized in this study have been defined previously.11,14–17 Per NCCN guidelines, adequate LNS was defined as examination of ≥15 LN, whereas examination of <15 LN signified inadequate LNS. Adjuvant therapy was defined as postoperative chemotherapy alone or chemotherapy plus radiotherapy (i.e., C ± RT); nonreceipt of adjuvant C ± RT was designated surgery alone. For purposes of subgroup analysis in the adjuvant C ± RT cohort, patients receiving chemoradiotherapy (CRT) and chemotherapy alone (CA) were identified. OS was defined as the interval between date of diagnosis and date of death or last contact.
Statistical Analysis
Descriptive statistics are presented as frequencies for categorical variables and mean ± standard deviation and median [interquartile range (IQR)] for continuous variables. Pearson’s χ 2 or Fisher’s exact tests and independent Student’s t tests were used to evaluate categorical and continuous variables, respectively. Nonparametric comparisons of continuous variables were performed using the Wilcoxon rank-sum test. Trends in utilization of adjuvant C ± RT were assessed with the Mantel–Haenszel χ 2 test. Backward, stepwise logistic regression analysis identified factors associated with receipt of adjuvant C ± RT.
Univariate OS estimates were calculated using the Kaplan–Meier method, with comparisons between adjuvant therapy (C ± RT, or chemoradiotherapy and chemotherapy alone) and surgery-alone groups performed using the log-rank test. Multivariable survival analysis was conducted using stepwise, Cox proportional hazards modeling. Potential confounders entered into the analysis included demographic, pathologic, and operative variables. Further multivariable analyses evaluated the impact of adjuvant C ± RT on OS within the following patient subsets: AJCC pathologic stage, IB and II; nodal status, node-negative (N0) and node-positive [N1 (1-2 positive), N2 (3–6 positive), or N3 (7+ positive)]; and adequacy of surgical LNS, <15 and ≥15 LNs examined. Finally, separate Cox models evaluated the impact of adjuvant chemotherapy alone and chemoradiotherapy, compared with surgery alone, on overall survival. p values ≤0.05 were considered statistically significant; all tests were two-sided. Statistical analyses were performed using SPSS v22 (IBM Corp., Armonk, NY).
Results
Descriptive Statistics and Temporal Trends in Treatment Utilization
Of 23,461 patients with stage IB-II gastric adenocarcinoma who met study criteria, median age was 71 (IQR 62.0–79.0) years; a majority of patients were male (63.4 %), white (72.7 %), held non-private insurance (69.5 %), and had income <$46,000 (62.0 %). Facility type and location with the largest relative case contributions were nonacademic (62.2 %) and southern (32.4 %) centers, respectively. The majority of tumors were characterized by: (a) nondistal (i.e., proximal stomach or lesser/greater curvature) gastric location (65.0 %); (b) size >2 cm (72.5 %); and (c) well/moderate tumor differentiation (52.0 %). Final pathologic staging revealed 60.6 % stage IB versus 39.4 % stage II, 86.4 % T1/T2 versus 13.6 % T3/T4, and 67.5 % node-negative versus 32.5 % node-positive tumors. Most patients (58.0 %) underwent subtotal/partial gastrectomy, and an R0 resection was achieved in a large majority of cases (92.7 %); however, only a third of patients underwent examination of at least 15 LNs (i.e., adequate LNS).
In the overall cohort (1998–2011), 18,630 (79.4 %) patients underwent surgery alone and 4,831 (20.6 %) patients received adjuvant C ± RT (chemoradiotherapy: 4152 [85.9 %]; chemotherapy alone: 1191 [14.1 %]). Demographic and clinical characteristics of these treatment groups are summarized in Table 1. Between 1998 and 2011, the proportion of patients undergoing surgery alone decreased from 91.9 to 77.3 %, corresponding to a significant increase in the use of adjuvant C ± RT: from 8 to 22.7 % (p < 0.001; Supplementary Fig. S1).
Predictors of Adjuvant Therapy Utilization
Multivariable analysis identified patient-, tumor-, and hospital-based characteristics predicting administration of adjuvant therapy in the overall cohort (1998–2011; Table 1). Patients were less likely to receive adjuvant C ± RT if they were older, female, had lower household income, held nonprivate insurance, were treated at a facility located in the western United States, presented with smaller (<2 cm) or nondistal tumors, or underwent a near total/total gastrectomy; age >76 years was the strongest predictor of failure to receive adjuvant C ± RT [odds ratio (OR) 0.17, 95 % confidence interval (CI) 0.15–0.19, p < 0.001]. Patients were more likely to receive adjuvant C ± RT if they were treated at a nonacademic institution or a facility located in the Midwest, presented with poorly differentiated or T3/T4 tumors, stage II disease, pathologic LN positivity, or underwent margin-positive resection or adequate LNS. Nodal positivity was most strongly associated with the receipt of adjuvant C ± RT (OR 5.86, 95 % CI 5.15–6.66, p < 0.001).
Impact of Adjuvant Therapy on Overall Survival
At a median follow-up of 93.7 (95 % CI 92.4–95.0) months, median OS in the cohort evaluable for survival analysis (n = 15,748) was 63.5 months; 1- and 5-year actuarial survival rates were 86 and 27 %, respectively. In stage-stratified Kaplan–Meier analysis, receipt of adjuvant C ± RT was associated with improved median survival compared with surgery alone (IB: 101.1 vs. 85.4 months, p = 0.009; II: 45.6 vs. 30.9 months; p < 0.001; Supplementary Table S1). Stage IB patients receiving adjuvant C ± RT demonstrated improved 1-year (94 vs. 89 %, p = 0.018), but not 5-year (both 61 %), actuarial survival compared with surgery alone. Conversely, stage II patients receiving adjuvant C ± RT demonstrated improved short- and long-term survival compared with surgery alone (1- and 5-year OS: 86 and 44 % vs. 77 and 34 %, respectively; both p < 0.001).
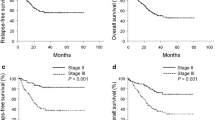
The impact of adjuvant C ± RT on OS was corroborated after controlling for potential confounders in Cox proportional hazards modeling. Undergoing surgery alone increased the relative risk of death [hazard ratio (HR) 1.24, 95 % CI 1.17–1.33, p < 0.001] relative to adjuvant C ± RT. Other factors independently associated with worse OS were higher pathologic stage (stage II: HR 1.25, 95 % CI 1.14–1.37), pathologic LN positivity (HR 1.68, 95 % CI 1.54–1.83), inadequate LNS (HR 1.38, 95 % CI 1.30–1.48), poor tumor differentiation (HR 1.15, 95 % CI 1.10–1.21), margin-positive resection (HR 1.79, 95 % C.I. 1.58–2.02), and nondistal/proximal tumor location (HR 1.12, 95 % CI 1.06–1.18; all p < 0.001; Table 2). Undergoing surgery alone also was associated with worse risk-adjusted OS compared with adjuvant C ± RT in each AJCC stage subgroup (IB: HR 1.23, 95 % CI 1.09–1.39, p = 0.001; II: HR 1.30, 95 % CI 1.20–1.40, p < 0.001; Fig. 2).
Impact of adjuvant chemotherapy ± radiotherapy (C ± RT) versus surgery alone on risk-adjusted overall survival in resected early stage gastric adenocarcinoma patients, stratified by AJCC pathologic stage subgroup (i.e., stage IB and stage II). The relative hazard (95 % CI) of undergoing surgery alone is indicated on each adjusted Kaplan–Meier curve, with adjuvant C ± RT serving as reference. For stage subgroups, unadjusted median survival statistics are provided at the bottom of each figure. HR hazard ratio, OS overall survival, mo months
Next, separate Cox models dissected the stage-stratified impact of adjuvant chemoradiotherapy compared with chemotherapy alone in ESGC. Both adjuvant regimens were associated with improved OS compared with undergoing surgery alone (overall cohort: p = 0.006 [CA], p < 0.001 [CRT]; stage IB: p = 0.023 [CA], p = 0.005 [CRT]; stage II: p = 0.016 [CA], p < 0.001 [CRT]; Supplementary Table S2; Fig. S2).
Influence of Surgical Lymph Node Staging on the Survival Impact of Adjuvant Therapy in ESGC Subgroups
We have previously demonstrated that inadequate LNS is not only an independently poor prognosticator of long-term outcomes, but also influences the survival impact of adjuvant therapy in resected gastric cancer in the United States.14,15 In order to specifically evaluate the effect of surgical lymph node staging on outcomes in early-stage disease, multivariable Cox regression analyses were stratified by adequacy of LNS in the overall cohort (n = 15,748), as well as stage IB (n = 9439), stage II (n = 6301), node-positive (n = 5301), and node-negative (n = 10,439) subgroups. In the overall cohort, surgery alone was associated with an increased hazard of risk-adjusted mortality relative to adjuvant C ± RT in both inadequately (HR 1.24, 95 % CI 1.15–1.34, p < 0.001) and adequately (HR 1.23, 95 % CI 1.09–1.39, p = 0.001) staged ESGC patients.
In the stage IB subgroup, surgery alone was associated with worse risk-adjusted OS in inadequately staged (HR 1.24, 95 % CI 1.08–1.43, p = 0.003) but not adequately staged (p = 0.355), patients. Conversely, in stage II patients, OS was significantly worse with surgery alone regardless of LNS adequacy (<15 LN: HR 1.29, 95 % CI 1.18–1.41, p < 0.001; ≥15 LN: HR 1.31, 95 % CI 1.14–1.51, p < 0.001).
In the subgroup of ESGC patients with node-positive disease, surgery alone was strongly associated with worse OS relative to adjuvant C ± RT (HR 1.36, 95 % CI 1.26–1.48, p < 0.001), regardless of LNS adequacy (<15 LN: HR 1.36, 95 % CI 1.23–1.50, p < 0.001; ≥15 LN: HR 1.37, 95 % CI 1.19–1.59, p < 0.001; Fig. 3). In node-negative patients overall, adjuvant C ± RT receipt was associated with a trend toward improved OS compared with surgery alone (HR 1.11, 95 % CI 1.00–1.24, p = 0.051). While this trend persisted in inadequately staged patients (HR 1.12, 95 % CI 1.00–1.27, p = 0.061), surgery alone was not associated with worse OS compared with adjuvant C ± RT in adequately staged node-negative patients (p = 0.960).
Impact of adjuvant chemotherapy ± radiotherapy (C ± RT) versus surgery alone on risk-adjusted overall survival in node-positive early stage gastric adenocarcinoma patients, stratified by adequacy of lymph node (LN) staging (inadequate:<15 LN examined; adequate: ≥15 LN examined). The relative hazard (95 % CI) of undergoing surgery alone is indicated on each adjusted Kaplan–Meier curve, with adjuvant C ± RT serving as reference. For the overall node-positive subgroup, unadjusted median survival statistics are provided at the bottom of the figure. HR hazard ratio, OS overall survival, mo months
Discussion
The present study indicates that consistent application of adjuvant therapy following gastrectomy in ESGC (i.e., stage IB-II) remains incomplete in the United States; nearly 80 % of resected ESGC patients did not commence national guideline-compliant adjuvant regimens as of 2011. Several demographic-, hospital-, and tumor-related factors appear to contribute to such omission, identifying opportunities for improvement in the delivery of cancer care. More importantly, these data affirm a stage-stratified survival benefit for adjuvant therapy (i.e., C ± RT, CRT, or CA) over surgery alone in ESGC patients undergoing curative-intent gastrectomy in the United States. The advantage of adjuvant C ± RT is most pronounced in stage II patients—regardless of LNS adequacy—and inadequately staged IB patients. Nodal status appears to be a critical determinant of the survival impact of adjuvant multimodality therapy in early stage disease; node-positive, but not adequately staged node-negative, patients derive benefit from post-gastrectomy C ± RT.
These data reinforce growing evidence indicating that omission of adjuvant therapy in ESGC patients is pervasive in clinical practice. Drawing from a Surveillance, Epidemiology, and End Results (SEER)-Medicare database cohort from 1991 to 2009, Snyder and colleagues demonstrated that omission of evidence-based adjuvant regimens was particularly frequent in ESGC patients; 72.4 % of stage IB and 50.6 % of stage II patients underwent surgery alone.10 A retrospective analysis from the Oregon State Cancer Registry (1996–2006) indicated that patients with stage IB disease were significantly less likely to receive adjuvant chemoradiotherapy.7 Using the NCDB, we recently developed a bootstrap-validated risk model predicting omission of adjuvant therapy following gastric resection; patients with T1/T2 and N0 tumors were significantly less likely to receive adjuvant C ± RT following gastrectomy.11
Omission in this cohort may, in part, reflect a perception that adjuvant therapy is dispensable, offering little advantage over surgery alone. This perception, however, is not clearly supported by data. On the contrary, subset analysis of 10-year follow-up data from the Intergroup-0116 trial suggested a putative benefit for adjuvant chemoradiotherapy in T1/T2, but not T3/T4, tumors.18 Beyond this, however, there is little evidence that specifically addresses the survival impact of a multimodality approach in ESGC patients.
Beyond indicating that a multimodality approach should be applied more consistently in ESGC patients overall, these data suggest that a more nuanced strategy may be appropriate: (a) if a patient is adequately staged at the time of gastrectomy—a scenario frequently unrealized in U.S. patients—adjuvant therapy should be strongly recommended in pathologic stage II and/or node-positive disease.14 Conversely, omission of adjuvant therapy may be considered in select adequately staged stage IB and/or node-negative (e.g., T2N0) patients; and (b) while the benefit of adjuvant C ± RT in inadequately staged stage II and/or node-positive patients is not surprising, its superiority in inadequately staged stage IB patients [and trend toward a similar benefit in node-negative patients (p = 0.061)] may be reflective of stage migration, wherein surgical understaging precludes identification of occult LN metastasis in overlooked nodal stations.
Several study limitations—characteristic of retrospective database analyses—warrant discussion, such as bias from missing data, misclassification of adjuvant therapy receipt, and inability to ascertain patient selection and referral patterns for adjuvant therapy. These factors may have inadvertently under- or over-estimated the impact of C ± RT in this study. Second, use of anatomically based LN dissection techniques (i.e., D1 vs. D2) are not captured by the NCDB, limiting ready translation from the numerically-based LNS definitions utilized herein. Moreover, the quality of pathologic assessment of resected specimens—an undoubted contributor to LNS adequacy and/or nodal status—cannot be discerned in this study. Third, a study of this nature cannot account for certain pertinent treatment-related details: (a) treatment intent; (b) specific chemotherapy regimens; (c) completion of prescribed treatment schedules; and (d) toxicities of administered therapies. Fourth, this analysis does not address the optimal adjuvant regimen (i.e., chemotherapy alone vs. chemoradiotherapy) for early-stage disease; indeed, this question is important and warrants prospective evaluation. Finally, lack of relapse data precludes assessment of disease-free survival; nonetheless, OS is an established surrogate for disease-specific mortality in gastric cancer.19
In summary, this report specifically addresses the impact of adjuvant multimodality therapy in resected early stage gastric cancer in the United States. While conclusions drawn from the present study are not intended to supplant clinical judgment, they may allow a more personalized approach to adjuvant therapy selection in specific ESGC patient subgroups. In particular, node-positive and stage II patients most obviously benefit from adjuvant C ± RT, regardless of LNS adequacy. Conversely, adequately staged node-negative and/or stage IB patients may represent populations in whom the morbidity of adjuvant systemic or locoregional therapies could be avoided. In this regard, these data emphasize the need for studies prospectively examining the relative impact of adjuvant C ± RT after standardized surgery.
References
National Cancer Institute. SEER Cancer Statistics Factsheets: Stomach Cancer. NCI, Bethesda, MD. http://seer.cancer.gov/statfacts/html/stomach.html. Accessed 5 June 2015.
Hundahl SA, Phillips JL, Menck HR. The National Cancer Data Base Report on poor survival of U.S. gastric carcinoma patients treated with gastrectomy: Fifth Edition American Joint Committee on Cancer staging, proximal disease, and the “different disease” hypothesis. Cancer. 2000;88(4):921–32.
Macdonald JS, Smalley SR, Benedetti J, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001;345(10):725–30.
Cunningham D, Allum WH, Stenning SP, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20.
Coburn NG, Guller U, Baxter NN, et al. Adjuvant therapy for resected gastric cancer: rapid, yet incomplete adoption following results of intergroup 0116 trial. Int J Radiat Oncol Biol Phys. 2008;70(4):1073–80.
Kozak KR, Moody JS. The survival impact of the intergroup 0116 trial on patients with gastric cancer. Int J Radiat Oncol Biol Phys. 2008;72(2):517–21.
Enestvedt CK, Diggs BS, Shipley DK, Thomas CR, Billingsley KG. A population-based analysis of surgical and adjuvant therapy for resected gastric cancer: are patients receiving appropriate treatment following publication of the intergroup 0116 results? Gastrointest Cancer Res. 2009;3(6):233–8.
Ejaz A, Spolverato G, Kim Y, et al. Impact of external-beam radiation therapy on outcomes among patients with resected gastric cancer: a multi-institutional analysis. Ann Surg Oncol. 2014;21(11):3412–21.
Ajani JA, Bentrem DJ, Besh S, et al. Gastric cancer, version 2.2013: featured updates to the NCCN Guidelines. J Natl Compr Cancer Netw. 2013;11(5):531–46.
Snyder RA, Penson DF, Ni S, Koyama T, Merchant NB. Trends in the use of evidence-based therapy for resectable gastric cancer. J Surg Oncol. 2014;110(3):285–90.
Datta J, McMillan MT, Shang EK, et al. Omission of adjuvant therapy after gastric cancer resection: development of a validated risk model. J Natl Compr Cancer Netw. 2015;13(5):531–41.
Bilimoria KY, Stewart AK, Winchester DP, Ko CY. The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol. 2008;15(3):683–90.
Fritz AG, Colton SW Jr. Memorial Fund. International classification of diseases for oncology: ICD-O. 3rd ed. Geneva: World Health Organization; 2000
Datta J, Lewis RS Jr, Mamtani R, et al. Implications of inadequate lymph node staging in resectable gastric cancer: a contemporary analysis using the National Cancer Data Base. Cancer. 2014;120(18):2855–65.
Datta J, McMillan MT, Ecker BL, et al. Implications of lymph node staging on selection of Adjuvant therapy for gastric cancer in the United States: a propensity score-matched analysis. Ann Surg.2015;263(2): 298–305.
Lowenfeld L, Datta J, Lewis RS Jr, et al. Multimodality treatment of T4 gastric cancer in the United States: utilization trends and impact on survival. Ann Surg Oncol. 2015;22(3): 863–872.
McMillan MT, Ojerholm E, Roses RE, et al. Adjuvant radiation therapy treatment time impacts overall survival in gastric cancer. Int J Radiat Oncol Biol Phys. 2015;21(2):326–336.
Smalley SR, Benedetti JK, Haller DG, et al. Updated analysis of SWOG-directed intergroup study 0116: a phase III trial of adjuvant radiochemotherapy versus observation after curative gastric cancer resection. J Clin Oncol. 2012;30(19):2327–33.
Coburn NG, Swallow CJ, Kiss A, Law C. Significant regional variation in adequacy of lymph node assessment and survival in gastric cancer. Cancer. 2006;107(9):2143–51.
Acknowledgment
None.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jashodeep Datta and Matthew T. McMillan have contributed equally to this manuscript.
Matthew T. McMillan is co first-author.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Datta, J., McMillan, M.T., Ruffolo, L. et al. Multimodality Therapy Improves Survival in Resected Early Stage Gastric Cancer in the United States. Ann Surg Oncol 23, 2936–2945 (2016). https://doi.org/10.1245/s10434-016-5224-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5224-1