Abstract
Background
Although the standard of care after recurrence of epithelial ovarian cancer (EOC) is chemotherapy, increasing data suggest that combining cytoreductive surgery with intraoperative hyperthermic intraperitoneal chemotherapy (HIPEC) is a promising option for patients with recurrent EOC. Our aim was to determine the prognostic value of the addition of HIPEC to secondary cytoreductive surgery (SCR) in recurrent EOC.
Methods
We analyzed a series of 79 patients with platinum-sensitive recurrent EOC who were treated from May 2000 to January 2014. Fifty patients who underwent SCR were compared to 29 who had SCR in combination with HIPEC.
Results
The SCR group had a higher median age (58.4 years) compared to the SCR + HIPEC group (51.6 years) (p = 0.006). The median hospital stay length was longer for SCR + HIPEC versus SCR patients (11 and 8 days, respectively; p = 0.009). More subjects experienced National Cancer Institute grade III–IV morbidity in the SCR + HIPEC group (34.5 %) compared to the SCR group (10.6 %) (p = 0.015). Conversely, there were no deaths in the SCR + HIPEC group and 2 (4.0 %) deaths the SCR group. The median disease-free survival did not differ between SCR and SCR + HIPEC patients (18.6 and 15.8 months, respectively; p = 0.82); nor did median overall survival (59.3 and 58.3 months, respectively; p = 0.95). The presence of carcinomatosis was the only variable that remained linked to a higher risk of recurrence and death in the multivariate analysis.
Conclusions
Our data suggest that the addition of HIPEC to cytoreduction in patients with recurrent platinum-sensitive EOC does not improve survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Epithelial ovarian cancer (EOC) is the most frequent cause of death among women with gynecologic malignancies. Surgery is the cornerstone treatment of advanced EOC, and the absence of residual disease is the strongest independent predictor of survival.1
The primary site of dissemination and recurrence in EOC is usually the peritoneum, making it an important target for the development of local therapies.2 Prior studies have reported a pharmacologic advantage of delivering cisplatin and paclitaxel intraperitoneally (IP), wherein a significantly higher concentration is achieved in the peritoneal space compared to intravenous administration.3–7
In phase 3 clinical trials of patients with minimal residual disease after primary surgery, the best survival results were observed with adjuvant IP chemotherapy.2,8 Despite the benefits of IP chemotherapy, clinicians are reluctant to incorporate IP therapy, predominantly as a result of concerns over greater toxicity, inconvenience, and catheter-related complications (blockage and infection).9
Nearly 70 % of patients with advanced EOC experience disease recurrence within 5 years of follow-up, and the optimal strategy for salvage therapy has not been established. Although the standard of care after recurrence of EOC is chemotherapy, depending on the patient’s disease-free interval and other variables, certain retrospective reports have noted better outcomes with secondary cytoreductive surgery (SCR), and 2 prospective randomized trials remain ongoing.10
In contrast to the hesitation in adding IP therapy to routine care, several institutions worldwide have proposed combining maximal cytoreductive surgery with intraoperative hyperthermic intraperitoneal chemotherapy (HIPEC) for patients with advanced EOC, primarily as a result of support from oncologic surgeons who have experience with peritoneal surface malignancies of gastrointestinal origin.11–24
Several small heterogeneous studies have recorded the outcomes of patients who had HIPEC after cytoreductive surgery for advanced-stage or recurrent disease. Despite morbidity rates of approximately 25–35 %, HIPEC continued to gain interest.17–20
Our aim was to determine the prognostic value of the addition of HIPEC to cytoreductive surgery for recurrent EOC in a series of patients who were treated at a single institution.
Materials and Methods
Patients
We analyzed 79 patients with platinum-sensitive recurrent EOC who were treated with SCR from May 2000 to January 2014 at AC Camargo Cancer Center. Fifty-three patients were treated in the Department of Gynecologic Oncology, and 26 were treated in Department of Pelvic Surgery. Fifty subjects had SCR, and 29 underwent SCR + HIPEC. All patients had SCR due to peritoneal recurrence. The median follow-up time after secondary surgery was 49.6 months (range 1–168 months). All 26 patients treated with SCR + HIPEC in the Department of Pelvic Surgery received platinum-based chemotherapy before surgery.
The patients’ clinical and pathologic data were retrieved from their medical records. Morbidity was analyzed according to the National Cancer Institute (NCI) common toxicity criteria. The extent of peritoneal carcinomatosis was determined on the basis of the peritoneal carcinomatosis index (PCI).25 The PCI is usually used to quantify peritoneal spread in HIPEC reports. Briefly, the PCI is a quantitative assessment of distribution and implant size of cancer throughout the abdomen and pelvis. The PCI scores 12 abdominal locations from 0 to 3 points, depending on the size of the lesion. Two components are involved in calculating this index: the distribution of the tumor in the abdomen or pelvic regions and the lesion size score.
The complexity of surgical procedures was categorized per the surgical complexity score (SCS) as follows: 1 (low complexity), 2 (intermediate), and 3 (high).26 The completeness of cytoreduction score (CC), introduced by Sugarbaker and Chang, was used to record residual disease.25 CC was scored as follows: CC-0, no macroscopic tumor visible; CC-1, largest residual tumor ≤2.5 mm; CC-2, largest residual tumor >2.5 mm and ≤2.5 cm; and CC-3, largest residual tumor >2.5 cm.
After SCR, HIPEC was performed by the closed technique, with the temperature ranging from 41 to 42 °C over 90 min. The agents were chosen at the surgical assistant’s discretion. Mitomycin C (10 mg/m2) and cisplatin (50 mg/m2) were administered in 15 cases (51.7 %), cisplatin (50 mg/m2) and doxorubicin were given in 8 cases (27.6 %), cisplatin alone (50 mg/m2) in 3 cases (10.3 %), and oxaliplatin alone in 3 cases (10.3 %). The IP drugs were diluted in 4000 mL of dialysis solution.
Patients were categorized into 2 groups: SCR and SCR + HIPEC.
Statistical Analysis
Follow-up time was defined as the interval from the date of surgery to the last date for which information was available. Disease-free survival (DFS) was considered the time from SCR to the date of recurrence or last follow-up. Overall survival (OS) was defined as the time from SCR to the date of death or last follow-up.
A database was constructed using SPSS 20.0 for Mac (IBM, Armonk, NY). The correlations between variables were assessed by Chi square test, Fisher’s exact test, Kruskal–Wallis test, or Mann–Whitney test. Survival curves were generated by Kaplan–Meier life table analysis and compared by log-rank test. Multivariate analysis was performed by Cox regression. For all tests, a p value of <0.05 was considered to be significant.
Results
Clinical and Pathologic Characteristics
The patients’ clinical and pathologic data are summarized in Table 1. The overall median age of the patients was 56.4 years (range 30–80 years). The SCR group had a higher median age (58.4 years) compared to SCR + HIPEC subjects (51.6 years) (p = 0.006). The median length of hospital stay was longer in the SCR + HIPEC (11 days) versus SCR group (8 days) (p = 0.009). The median PCI was 6 for both groups (p = 0.78). The presence of carcinomatosis (p = 0.30), SCS (p = 0.47), CC, and presence of any residual disease did not differ significantly between groups.
There were more subjects with grade III–IV NCI morbidity in the SCR + HIPEC (34.5 %) versus the SCR group (10.6 %) (p = 0.015). Conversely, there were no perioperative deaths (within 30 days after surgery) in the SCR + HIPEC group and 2 (4.0 %) deaths in the SCR group. These deaths were due to mesenteric ischemia and bowel fistula, respectively, and both patients were American Society of Anesthesiologists (ASA) grade III. Further, in the SCR group, there were 6 (12.8 %) ASA III patients but none in the SCR + HIPEC cohort (p = 0.078).
Recurrence and Survival
After a median follow-up of 49.6 months (range 1–168 months), 63 patients (79.9 %) experienced recurrence. Further, 19 patients (24.1 %) were alive with no evidence of disease, 18 (22.8 %) were alive with disease, 40 (50.6 %) died, and 2 (2.5 %) were lost follow-up. The median disease-free interval from primary cytoreduction to the first recurrence was 27.9 months (range 11–178 months).
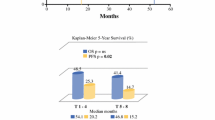
The median DFS after secondary surgery was 18.3 months (95 % confidence interval 13.8–22.7). The presence of carcinomatosis correlated with a worse DFS compared to the absence of carcinomatosis (median DFS: 11.5 vs. 30.9 months; p < 0.001). The other factors that were associated with a worse DFS were PCI > 6 versus ≤6 (median DFS: 13.4 vs. 29.1 months, p < 0.001) and SCS ≥ 2 versus 1 (median DFS: 16.4 vs. 25.8 months; p = 0.011). Age, disease-free interval from primary cytoreduction of <18 months, and presence of residual disease were not linked to DFS in the univariate analysis (Table 2). Also, the median DFS did not differ between the SCR and SCR + HIPEC groups (18.6 and 15.8 months, respectively; p = 0.82) (Fig. 1).
The median OS was 62 months (95 % confidence interval 26.8–97.2). The presence of carcinomatosis was associated with a worse OS compared to its absence (median OS: 36.2 vs. 109 months; p = 0.001). PCI > 6 also negatively impacted the OS compared to PCI ≤ 6 (median OS: 49.7 and 109 months; p = 0.020). Age, SCS ≥ 2, disease-free interval from primary cytoreduction of <18 months, and presence residual disease did not correlate negatively with OS in the univariate analysis (Table 2).
There was no difference in OS between the SCR and SCR + HIPEC groups. The median OS for SCR patients was 59.3 months (5-year OS rate: 49.5 %) and 58.3 months for the SCR + HIPEC group (5-year OS: 49.7 %) (p = 0.95) (Fig. 1).
When only patients with CC ≤ 1 were analyzed, OS remained unchanged between groups, with a median OS of 59.3 months for SCR patients (5-year OS: 47.7 %) and 58.3 months for SCR + HIPEC subjects (5-year OS: 49.4 %) (p = 0.95). In the multivariate analysis, the presence of carcinomatosis was the only variable that retained its association with a higher risk of recurrence and death (Table 3).
Discussion
The use of HIPEC in treating peritoneal carcinomatosis of ovarian origin is considered to be an attractive option by many groups.16,17,20,22 However, in our study, there was no impact on survival in recurrent EOC when HIPEC was added to SCR. In contrast, HIPEC was more significantly associated with grade III–IV morbidity.
Two major arguments support hyperthermic chemotherapy based on the reported increase in cytotoxicity of cisplatin and other drugs in human cell lines and animal models. First, cytotoxicity is elevated at higher temperatures and might overcome platinum resistance. Second, the penetration of intraperitoneally administered cisplatin improves when combined with hyperthermia and might raise intracellular drug concentrations. Other advantages include the ability to ensure that the entire peritoneal surface is exposed to chemotherapy before the expected perioperative adhesions develop.27–31
Nevertheless, the data regarding this matter are heterogeneous and incomplete. More than 20 publications have focused on ovarian cancer and HIPEC, including more than 900 patients in the recurrent setting.18 Yet most of these trials have been small and have had broad entry criteria. Further, it is difficult to analyze and define the factors (extent of surgery, IP chemotherapy, and hyperthermia) of HIPEC that actually mediate the improved outcomes in these patients. The largest retrospective series is a multi-institutional French study that included 566 patients, 474 of whom were in the recurrent setting. Bakrin et al. reported a 45.7-month median survival for recurrent ovarian cancer, recording mortality and grade III–IV morbidity rates of 0.8 and 31.3 %, respectively.17 Notably, there was no significant difference in overall survival between patients with chemosensitive and chemoresistant recurrence.
There are 4 comparative trials that have analyzed the survival benefits of HIPEC (Table 4), all of which have reported favorable survival outcomes with HIPEC.21–24 However, the small number of patients and the inclusion of patients who did not undergo surgery in these studies make the comparison between groups difficult. Conversely, our study compared patients who were treated with SCR with or without HIPEC during the same period and in the same institution.
In contrast to these studies, we did not find any impact on survival in favor of HIPEC. The strength of our study is that we compared 2 groups that were treated at the same institution but by 2 departments. Further, all surgeons were trained in surgical oncology at the same institution and have performed extensive cytoreductive procedures. Notably, the groups did not differ regarding the extent of disease or surgery, which might have decreased the impact of selection bias.
The best evidence of HIPEC in EOC comes from a phase 3 trial by Spiliotis et al., who randomized 120 patients with recurrent EOC (platinum sensitive and resistant) to SCR or SCR + HIPEC and reported better survival in the group that received HIPEC.32 However, the comparison between groups was not evaluated statistically and might be heterogeneous. Specifically, there were more patients with stage IV and residual disease in the group that did not receive HIPEC. Moreover, the statistical analysis was unclear because the authors focused their findings on mean overall survival. However, according to the survival plots, median survival was not reached. Although a subgroup analysis might not allow such conclusions to be reached, the group reported no differences in survival for platinum-sensitive disease.
Nevertheless, important published clinical trials, such as OCEANS and CALYPSO, that have included platinum-sensitive recurrent disease have shown a median survival of 33 to 35 months for patients who received chemotherapy only.33,34 Conversely, many retrospective studies have demonstrated that patients with platinum-sensitive disease who received secondary surgery at the time of recurrence experienced a median survival of approximately 50 months. Harter et al. reported better outcomes of more than 60 months for patients with positive arbeitsgemeinschaft gynaekologische onkologie studiengruppe ovarialkarzinom (AGO-OVAR) scores (good performance status, absence of ascites, and no residual disease after primary surgery).35 Zang et al. published a review that included 1100 patients and noted a median survival of 57.7 months after SCR with no residual disease.36 Finally, in the largest retrospective analysis of data on tertiary cytoreduction (n = 406), Fotopoulou et al. suggested that complete debulking retains its impact on survival, effecting a median survival of 49 months, even without HIPEC.37 Our findings are consistent with these studies: our patients had a median survival of 62 months after secondary surgery.
Wide ranges of toxicity in HIPEC trials have been reported in the recurrent setting. Severe surgical mortality and morbidity range from 0 to 7 and 19 to 40 %, respectively.18–20 These results might be attributed to the complexity of the surgical procedures that are required to obtain complete cytoreduction. However, these rates are higher than in the literature on SCR without HIPEC—approximately 10 to 12 %.38 In our series, 10.6 and 34.5 % of SCR and SCR + HIPEC patients, respectively, had NCI grade III–IV morbidity. Notably, the group that did not receive HIPEC was older and more likely to be ASA III, and the only 2 perioperative deaths occurred in patients who did not receive HIPEC. HIPEC patients had a longer length of hospital stay. Future trials should more accurately separate the adverse events that are related to HIPEC from the inherent risks of aggressive cytoreduction.
The sole method of distinguishing the impact of a novel therapeutic strategy from selection bias is performing phase 3 clinical trials, which we eagerly await for HIPEC. Meanwhile, as a result of insufficient evidence, the relevant international guidelines and a recent consensus do not include HIPEC as a standard treatment for primary or recurrent ovarian cancer.39 Moreover, the AGO-OVAR group recently published a formal statement against the use of HIPEC outside of clinical trials.40
We have presented a single-institution comparative series that provides valuable data. Unfortunately, in a retrospective setting, it may suffer from inherent bias. Despite the current controversy, our data indicate that HIPEC after SCR has no impact on survival.
References
du Bois A, Reuss A, Pujade-Lauraine E, et al. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe dʼInvestigateurs Nationaux Pour les Etudes des Cancers de lʼOvaire (GINECO). Cancer. 2009;115:1234–44.
Tewari D, Java JJ, Salani R, et al. Long-term survival advantage and prognostic factors associated withintraperitoneal chemotherapy treatment in advanced ovarian cancer: a Gynecologic Oncology Group study. J Clin Oncol. 2015;33:1460–6.
Lopez JA, Krikorian JG, Reich SD, et al. Clinical pharmacology of intraperitoneal cisplatin. Gynecol Oncol. 1985;20:1–9.
Pretorius RG, Hacker NF, Berek JS, et al. Pharmacokinetics of IP cisplatin in refractory ovarian carcinoma. Cancer Treat Rep. 1983;67:1085–92.
Francis P, Rowinsky E, Schneider J, et al. Phase I feasibility and pharmacologic study of weekly intraperitoneal paclitaxel: a Gynecologic Oncology Group pilot study. J Clin Oncol. 1995;13:2961–7.
Markman M, Rowinsky E, Hakes T, et al. Phase I trial of intraperitoneal taxol: a Gynecologic Oncology Group study. J Clin Oncol. 1992;10:1485–91.
Dedrick RL, Myers CE, Bungay PM, DeVita Jr, VT. Pharmacokinetic rationale for peritoneal drug administration in the treatment of ovarian cancer. Cancer Treat Rep. 1978;62:1–11.
Armstrong DK, Bundy B, Wenzel L, et al; Gynecologic Oncology Group. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med. 2006;354:34–43.
Walker JL, Armstrong DK, Huang HQ, et al. Intraperitoneal catheter outcomes in a phase III trial of intravenous versus intraperitoneal chemotherapy in optimal stage III ovarian and primary peritoneal cancer: a Gynecologic Oncology Group study. Gynecol Oncol. 2006;100:27–32.
Al Rawahi T, Lopes AD, Bristow RE, et al. Surgical cytoreduction for recurrent epithelial ovarian cancer. Cochrane Database Syst Rev. 2013;2:CD008765.
Di Giorgio A, Naticchioni E, Biacchi D, et al. Cytoreductive surgery (peritonectomy procedures) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) in the treatment of diffuse peritoneal carcinomatosis from ovarian cancer. Cancer. 2008;113:315–25.
Pavlov MJ, Kovacevic PA, Ceranic MS, Stamenkovic AB, Ivanovic AM, Kecmanovic DM. Cytoreductive surgery and modified heated intraoperative intraperitoneal chemotherapy (HIPEC) for advanced and recurrent ovarian cancer—12-year single center experience. Eur J Surg Oncol. 2009;35:1186–91.
Helm CW, Richard SD, Pan J, et al. Hyperthermic intraperitoneal chemotherapy in ovarian cancer: first report of the HYPER-O registry. Int J Gynecol Cancer. 2010;20:61–9.
Roviello F, Pinto E, Corso G, et al. Safety and potential benefit of hyperthermic intraperitoneal chemotherapy (HIPEC) in peritoneal carcinomatosis from primary or recurrent ovarian cancer. J Surg Oncol. 2010;102:663–70.
Parson EN, Lentz S, Russell G, Shen P, Levine EA, Stewart JH. Outcomes after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal surface dissemination from ovarian neoplasms. Am J Surg. 2011;202:481–6.
Deraco M, Kusamura S, Virzì S, et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy as upfront therapy for advanced epithelial ovarian cancer: multi-institutional phase-II trial. Gynecol Oncol. 2011;122:215–20.
Bakrin N, Bereder JM, Decullier E, et al; FROGHI (FRench Oncologic and Gynecologic HIPEC) Group. Peritoneal carcinomatosis treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) for advanced ovarian carcinoma: a French multicentre retrospective cohort study of 566 patients. Eur J Surg Oncol. 2013;39:1435–43.
Chiva LM, Gonzalez-Martin A. A critical appraisal of hyperthermic intraperitoneal chemotherapy (HIPEC) in the treatment of advanced and recurrent ovarian cancer. Gynecol Oncol. 2015;136:130–5.
Chua TC, Robertson G, Liauw W, Farrell R, Yan TD, Morris DL. Intraoperative hyperthermic intraperitoneal chemotherapy after cytoreductive surgery in ovarian cancer peritoneal carcinomatosis: systematic review of current results. J Cancer Res Clin Oncol. 2009;135:1637–45.
Bakrin N, Classe JM, Pomel C, Gouy S, Chene G, Glehen O. Hyperthermic intraperitoneal chemotherapy (HIPEC) in ovarian cancer. J Visc Surg. 2014;151:347–53.
Munoz-Casares FC, Rufian S, Rubio MJ, et al. The role of hyperthermic intraoperative intraperitoneal chemotherapy (HIPEC) in the treatment of peritoneal carcinomatosis in recurrent ovarian cancer. Clin Transl Oncol. 2009;11:753–9.
Fagotti A, Costantini B, Petrillo M, et al. Cytoreductive surgery plus HIPEC in platinum-sensitive recurrent ovarian cancer patients: a case-control study on survival in patients with two-year follow-up. Gynecol Oncol. 2012;127:502–5.
Le Brun J, Campion L, Berton-Rigaud D, et al. Survival benefit of hyperthermic intraperitoneal chemotherapy for recurrent ovarian cancer: a multi-institutional case-control study. Ann Surg Oncol. 2014;21:3621–7.
Safra T, Grisaru D, Inbar M, et al. Cytoreduction surgery with hyperthermic intraperitoneal chemotherapy in recurrent ovarian cancer improves progression-free survival, especially in BRCA-positive patients—a case-control study. J Surg Oncol. 2014;110:661–5.
Sugarbaker P, Chang D. Results of treatment of 385 patients with peritoneal surface spread of appendiceal malignancy. Ann Surg Oncol. 1999;6:727–31.
Aletti GD, Santillan A, Eisenhauer EL, et al. A new frontier for quality of care in gynecologic oncology surgery: multi-institutional assessment of short-term outcomes for ovarian cancer using a risk-adjusted model. Gynecol Oncol. 2007;107:99–106.
Hahn GM. Potential for therapy of drugs and hyperthermia. Cancer Res. 1979;73:2264–8.
Alberts DS, Peng YM, Chen HS, et al. Therapeutic synergism of hyperthermia-cis-platinum in a mouse tumor model. J Nat Cancer Inst. 1980;73:455–61.
Xu MJ, Alberts DS. Potentiation of platinum analogue cytotoxicity by hyperthermia. Cancer Chemother Pharmacol. 1988;21:191–6.
Maymon R, Bar-Shira Maymon B, Holzinger M, Tartakovsky B, & Leibovici J. Augmentative effects of intracellular chemotherapy penetration combined with hyperthermia in human ovarian cancer cells lines. Gynecol Oncol. 1994;55:265–70.
Istomin YP, Zhavrid EA, Alexandrova EN, Sergeyeva OP, & Petrovich SV. Dose enhancement effect of anticancer drugs associated with increased temperature in vitro. Exp Oncol. 2008;30:56–9.
Spiliotis J, Halkia E, Lianos E, et al. Cytoreductive surgery and HIPEC in recurrent epithelial ovarian cancer: a prospective randomized phase III study. Ann Surg Oncol. 2015;22:1570–5.
Aghajanian C, Blank SV, Goff BA, et al. OCEANS: a randomized, double-blind, placebo-controlled phase III trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent epithelial ovarian, primary peritoneal, or fallopian tube cancer. J Clin Oncol. 2012;30:2039–45.
Wagner U, Marth C, Largillier R, et al. Final overall survival results of phase III GCIG CALYPSO trial of pegylated liposomal doxorubicin and carboplatin vs paclitaxel and carboplatin in platinum-sensitive ovarian cancer patients. Br J Cancer. 2012;107:588–91.
Harter P, Beutel B, Alesina PF, et al. Prognostic and predictive value of the Arbeitsgemeinschaft Gynaekologische Onkologie (AGO) score in surgery for recurrent ovarian cancer. Gynecol Oncol. 2014;132:537–41.
Zang RY, Harter P, Chi DS, et al. Predictors of survival in patients with recurrent ovarian cancer undergoing secondary cytoreductive surgery based on the pooled analysis of an international collaborative cohort. Br J Cancer. 2011;105:890–6.
Fotopoulou C, Zang R, Gultekin M, et al. Value of tertiary cytoreductive surgery in epithelial ovarian cancer: an international multicenter evaluation. Ann Surg Oncol. 2013;20:1348–54.
Kommoss S, Rochon J, Harter P, et al. Prognostic impact of additional extended surgical procedures in advanced-stage primary ovarian cancer. Ann Surg Oncol. 2010;17:279–86.
Morgan RJ Jr, Alvarez RD, Armstrong DK, et al; National Comprehensive Cancer Networks. Ovarian cancer, version 2.2013. J Natl Compr Canc Netw. 2013;11:1199–209.
Harter P, Mahner S, Hilpert F, et al. Statement by the Kommission OVAR of the AGO Study Group on the use of HIPEC (Hyperthermic Intraperitoneal Chemotherapy) to treat primary and recurrent ovarian cancer. Geburtshilfe Frauenheilkd. 2013;73:221–3.
Disclosure
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baiocchi, G., Ferreira, F.O., Mantoan, H. et al. Hyperthermic Intraperitoneal Chemotherapy after Secondary Cytoreduction in Epithelial Ovarian Cancer: A Single-center Comparative Analysis. Ann Surg Oncol 23, 1294–1301 (2016). https://doi.org/10.1245/s10434-015-4991-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4991-4