Abstract
Background
The techniques of intracorporeal anastomosis and specimen extraction after laparoscopic colectomy via a natural orifice have gained interest increasingly. We evaluated the feasibility of our unique techniques for colorectal reconstruction and report immediate postoperative outcomes in patients with rectosigmoid cancer.
Methods
Patients with sigmoid or rectal cancer were selected depending on the size of the tumor and its distance from the anal verge. Demographic data, operative parameters, and postoperative outcomes were assessed. After complete resection of the tumor, all patients underwent an intracorporeal side-to-end colorectal anastomosis following transrectal specimen extraction.
Results
Laparoscopic resection with our technique of intracorporeal anastomosis was successful in 32 patients. The average operative time was 192 ± 29 min, and mean blood loss was 51 ± 18 ml. All patients experienced mild postoperative pain, and bowel function returned before postoperative day 3 in most patients. They had an uneventful postoperative course with a median hospital stay of 6 days. Major perioperative complications or anastomotic leak were not encountered in this study. The mean size of the lesion was 3.3 ± 1.8 cm, and the mean number of harvested nodes was 14 ± 6. During the follow-up period, there were no functional disorders associated with the intracorporeal anastomosis or transrectal specimen extraction.
Conclusions
Intracorporeal side-to-end colorectal anastomosis with transrectal specimen extraction in laparoscopic colorectal surgery is a safe and effective procedure for patients with rectosigmoid malignancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The introduction of laparoscopic surgery has been proven to be both feasible and satisfactory for the treatment of benign and malignant colorectal diseases so that more surgeons would prefer to adopt the technique of laparoscopic colectomy. However, the problems of bowel anastomosis and retrieval of the surgical specimen through an abdominal incision after laparoscopic colectomy remain to be solved. Currently, laparoscopic colectomy continues to progress in an effort to reduce the invasiveness of the procedure and increase the comfort of the patient. The utilization of a natural orifice, obviating the need of an abdominal wound, to facilitate both complex procedures may improve the short-term outcome of laparoscopic colectomy and reduce postoperative wound complications. Natural orifice surgery might reduce postoperative pain, morbidity, and length of hospital stay. The advantages of laparoscopic colectomy using the techniques of intracorporeal anastomosis combined with natural orifice specimen extraction (NOSE) are increasingly reported.1–6
Various surgical techniques for colorectal anastomosis have been used for laparoscopic left colectomy. End-to-end anastomosis with a circular staple is commonly performed either intracorporeally or extracorporeally.1–12 However, a side-to-end colorectal anastomosis after colectomy has gained functional advantages and surgical safety and is becoming increasingly common.13 , 14 We present a novel and simple technique of intracorporeal side-to-end colorectal anastomosis incorporated with transrectal specimen retrieval for patients with sigmoid or rectal neoplasms to verify its feasibility and report immediate postoperative outcomes.
Patients
Between the period of January 2013 and December 2014, a total of 32 patients with sigmoid or rectal cancer were recruited depending on the size of the tumor and its distance from the anal verge. Demographic data, operative parameters, and postoperative outcomes were assessed. Inclusion criteria for this technique were as follows: (1) patients with sigmoid colon cancer or rectal cancer; (2) aged between 18 and 90 years; (3) distance of tumor from the anal verge was >6 cm; (4) tumor size <6.5 cm; and (5) body mass index ≤28.
Preoperative Preparation
All patients started a low-roughage diet 3 days before surgery and drank only clear liquids the day before surgery. Two doses (45 ml/dose) of oral sodium phosphate (Fleet, C.B. Fleet Company, Inc., USA) with an interval of 8 h and oral antibiotic (metronidazole 750 mg) were given the day before surgery.
Surgical Technique
Dissection of the Sigmoid Colon and Proximal Rectum
Under general anesthesia and with the patient in the Trendelenburg position, four trocars were placed after creation of a pneumoperitoneum with one 10-mm port in the umbilicus, one 12-mm port in the right iliac fossa, and two 5-mm ports in the right and left upper quadrants. After entering the abdominal cavity, the lymphovascular trunk to the rectosigmoid colon were carefully ligated and divided, and then the sigmoid colon with its mesocolon were mobilized in medial to lateral direction as the usual manner, using a tissue sealing-device (ENSEAL® Ethicon Endo-Surgery, Johson & Johnson, USA). Once the sigmoid colon was entirely mobilized, two ligatures (silk tie) were made proximal and distal to the tumor respectively, and the distal rectum was thoroughly irrigated with povidone iodine solution via a rectal tube. The rectum was then transected using a cautery device.
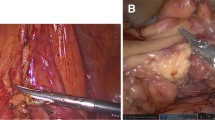
Fixation of the Anvil
A 15-cm suction tube of 12-F size connecting snugly with the taper end of an ancillary trocar was used as the guide tube (Fig. 1). The anvil of a circular stapling device (CDH 29; Ethicon Endo-Surgery, Cincinnati, OH) was delivered into the peritoneal cavity transanally. A sigmoid colotomy proximal to the malignant lesion was made for introducing the anvil of the stapler and, at the 6-cm distance proximal to the colotomy, another small hole for inserting the guide tube was created. The guide tube was inserted through the small hole into the colonic lumen and advanced to the colotomy. The ancillary trocar, being caught by a grasper, was lodged in the anvil shaft. By gently pulling the guide tube in the opposite direction, the anvil shaft was exposed through the small hole extraluminally. After detaching the guide tube from the anvil, the sigmoid colon was divided proximally to the colotomy by a linear stapler and ready for anastomosis (Video 1).
Extraction of the Resected Specimen
A rectoscope (TEO, Karl Storz, Tuttlingen, Germany) for transanal endoluminal microsurgery was inserted transanally into the lower rectum and held in place outside the anal orifice. The resected specimen was then extracted through the rectum and delivered transanally. As the rectoscope was removed, the opened distal rectum was closed using the endoscopic linear stapler (Video 2). In cases of the shorter rectal stump, four stay stitches were made at the edge of the rectal stump for cephalic traction to facilitate proper tissue positioning while stapling the stump opening. In two patients with tumor sizes of 5.1 and 6.2 cm, the tumors could not be extracted freely through the lumen of the rectoscope. They were placed in the specimen bag and then the bag, being caught transanally by a grasping instrument, was simultaneously extracted along with the rectoscope, which served as a dilator of the anorectal canal while it was being withdrawn.
Colorectal Anastomosis
A side-to-end colorectal anastomosis was intracorporeally fashioned with the use of the CDH stapling device introduced transanally. A latex drain was placed in the pelvis, and the 10–12-mm ports were closed with a Vicryl suture meticulously to reduce the risk of port site herniation (Video 3).
Perioperative Care
After completing the colorectal stapling, an anastomotic leak test was performed with air insufflation through the TEO proctoscope, with the anastomotic site under irrigation and with proximal colon occluded in all patients. Intraperitoneal fluid was collected at the end of the surgical procedure in all patients. All fluid samples were sent to the laboratory for bacterial culture. In all patients, leukocyte count and CRP level were routinely checked on the second postoperative day (POD) as the index of inflammatory response. Patient-controlled analgesia (PCA) device was given for pain control postoperatively if necessary. Pain score and the frequency of PCA used also were recorded for POD1 and POD2.
Results
The current technique has been used to treat all 32 patients with colorectal cancers without any conversion to conventional technique. The demographic characteristics of patients with NOSE are given in Table 1. Postoperative outcomes and pain scores are shown in Table 2. Among the 14 patients with stages III, 3 with rectal cancer had preoperative chemoradiotherapy, whereas no additional specific treatment was performed preoperatively in the remaining patients. In patients with neoadjuvant chemotherapy, a temporary loop ileostomy at the 12-mm trocar site was routinely created for fecal diversion for 3 months. In this study, neoadjuvant treatment might not be applicable in four patients with stage II rectal cancer, because the tumors were of relatively small size (<3 cm) and located in the upper rectum.
Based on the findings of sample fluid culture, the incidence of intraperitoneal contamination was extremely high, accounting for 75 % (24/32) of all patients with NOSE-colectomy. Contamination of mixed aerobic and anaerobic pathogens was present in five patients. However, the development into clinically significant peritoneal infection was not observed in this series. Escherichia coli was the most common aerobic pathogen in eight patients, followed by Klebsiella pneumoniae in four patients and Pseudomonas aeruginosa in two patients. In the anaerobic group, Bacteroides fragilis in five patients was most frequently found, followed by Peptostreptococcus sp. in two patients and Clostridium perfringens in one patient. Other pathogens were found by intraperitoneal fluid culture, including Enterococcus faecium, Enterobacter aerogenes, Acinetobacter baumannii, Staphylococcus hominis, and Stenotrophomonas maltophilia.
Major perioperative complications or anastomotic leak were not encountered in this study. The average operative time was 192 ± 29 min and blood loss was 51 ± 18 ml. All patients experienced mild postoperative pain with a mean VAS score of 3.7 ± 1.0, and their bowel function returned before POD 3 in most patients. Surgical specimen was pathologically confirmed an adenocarcinoma in all patients, and all surgical margins were free from cancer involvement. The mean tumor size was 3.3 ± 1.8 cm, and the mean lymph nodes harvested were 14 ± 6. They had an uneventful postoperative course with a median hospital stay of 6.5 days. Postoperative morbidities were evaluated for 30 days after surgery both in hospital stay and outpatient department (OPD) visits, and all patients were then followed at our OPD monthly in the first half-year after operation. During the follow-up period between 6 and 20 months, there was no case with anal dysfunction and all patients were continent.
Discussion
The advantages of laparoscopically assisted colectomy that include less pain, fewer wound-related complications, and faster recovery during the short-term period have been well recognized. Nevertheless, an abdominal minilaparotomy for extraction of the specimen or extracorporeal bowel anastomosis is generally required in most conventional laparoscopic approaches after the bowel has been laparoscopically mobilized. To reduce the invasiveness of laparoscopic colectomy as much as possible, a great variety of techniques have been developed regarding totally intracorporeal anastomosis combined with extraction of the specimen through natural orifices, and favorable results were obtained.3–5 , 8–12 NOSE colectomy may represent the intermediate step of the evolution from conventional laparoscopic surgery to scarless surgery. NOSE procedure may increase the benefit of laparoscopic surgery to a great extent by eliminating the minilaparotomy wound. In addition, compared with extracorporeal reconstruction intracorporeal bowel anastomosis is superior in term of postoperative pain, return of bowel function, hospital stay, and morbidity.11 However, technical complexity and difficulty with totally intracorporeal anastomosis have limited extensive acceptance of these procedures by most laparoscopic surgeons.9 , 10
In this report, we have simplified the procedure of anvil insertion and fixation, and thus a side-to-end colorectal anastomosis can be elegantly accomplished. In the literature, several procedures of intracorporeal colorectal anastomosis have been demonstrated with varying degrees of advantages and disadvantages, including the use of an Endo-loop (Ethicon Endo-Surgery, Cincinnati, OH), a handsewn pursestring suture or a 2-0 monofilament suture (Prolene; Ethicon, Inc., Somerville, NJ) on the colonic wall.3 , 5–7 , 13 Our procedures have several advantages superior to conventional techniques.3 , 6 , 7 , 13 , 15 According to the present technique, the planned location for a suitable side-to-end anastomosis, instead of an end-to-end type, can be properly determined. If the anastomotic site can be designated at adequate distance apart from the suture line of the stump, a well-perfused anastomosis is guaranteed to enhance better wound healing. Recent studies regarding the stapled colorectal anastomosis have emphasized the use of side-to-end colorectal anastomosis as an alternative to a colonic pouch due to its similar functional outcome.16 Contrary to the other techniques, no multiple firing of the rectal stump is required, and more disposable staplers and medical expense can be spared.3 , 6 , 15 The pursestring suture by hand sewing requires more skillful technique and is relatively time-consuming. The technique using an Endo-loop, if a slip of the Endo-loop entrapment happened, can lead to anastomotic failure.
The current procedures seem to be technically simple, safe, and time-saving without making additional abdominal incision or extending the trocar wound. Moreover, elimination of the abdominal incision will theoretically reduce the risk of wound comorbidity.9 , 15 , 17 The concern that laparoscopic colectomy with intracorporeal anastomosis might be associated with a significantly longer operating time compared with the open technique has been addressed. Published clinical data have suggested that either transvaginal or transanal NOSE do not prolong operating time for laparoscopic colorectal surgery.12 On the contrary, another case–control study indicated that NOSE still took longer to perform intracorporeal suturing and anastomosis than the conventional laparoscopically assisted procedure.9 In this study, surgical dissection was greatly facilitated by the use of the laparoscopic energy device to reduce the operation time and control bleeding. Blood loss in our surgery was minimal. Another matter of concern is the risk of pelvic contamination during transrectal specimen extraction. The rectal stump for delivering the specimen and the colotomy for inserting the anvil were manipulated during the procedure, causing the risk of intraperitoneal soiling. Although high risk of peritoneal contamination was evident and there was elevation of CRP level in the POD 2 in our series, no patient developed peritoneal infection clinically. Recent, prospective studies demonstrated that although a higher peritoneal contamination was found in the NOSE procedures, there were no significant differences in clinical outcomes relative to a standard approach.5 , 18 The risk of contamination can be minimized by thorough distal rectal washout before delivering the surgical specimen via the rectum.
In this study, the use of a rectoscope to extract the specimen serves to decrease local soiling, protect rectal trauma, and prevent rectal prolapse. A recent systemic review, referring to a total of 462 patients in different centers, on NOSE-colectomy has reported that 33 % of the 12 studies had NOSE-colectomy using various rigid rectoscopes for rectal protection, including TEO, TEM, or a McCartney Tube.18 It appears that this technique has not been widely adopted due to potential limitation in a hospital without a TEM system for transanal procedures. Although laparoscopic NOSE-colectomy has been found to be safe and feasible in most cases, a drawback of the present study is that our patients were highly selected with low BMI of 23 and small tumor of 3.3 cm. The limited diameter of the TME rectoscope also can be the determining factor for easy and successful tumor extraction transrectally. Therefore, it should be logically emphasized that our approach is not recommended in patients with high BMI and a bulky mesocolon, and patients with large tumors >6.5 cm in size or locally advanced transmural cancer due to the difficulties of tumor resection and specimen extraction, and high risk of tumor cell seeding.
Because of the differences in operative technique and small population of included patients, it is impossible to make comparison of the data on operative details and postoperative outcomes, such as duration of surgery, complications, and length of hospital stay, among various studies. However, in reviewing the literature regarding NOSE surgery, our short-term postoperative outcomes seem to be comparable to these of available studies. It has been reported that avoiding a minilaparotomy to extract the specimen resulted in a significantly lower postoperative analgesic requirement in the NOSE technique.7 , 19 Our results also confirmed low VAS score in NOSE patients; therefore, the use of analgesics in the recovery period can be reduced. Moreover, our findings suggest that NOSE techniques do not prolong either operative time or length of hospitalization for laparoscopic colorectal surgery compared with published data in multicentre trials.4 , 18
Conclusions
Totally laparoscopic colectomy with intracorporeal side-to-end anastomosis and NOSE provides satisfactory short-term advantages of early recovery and short hospital stay and can be considered as an alternative treatment for patients with colorectal tumors. Moreover, our technique may maximize the benefits of laparoscopic surgery and can be universally adopted in left colectomies or anterior resection for rectosigmoid diseases to facilitate a safe and easy intracorporeal anastomosis and specimen extraction.
References
Palanivelu C, Rangarajan M, Jategaonkar PA, Anand NV. An innovative technique for colorectal specimen retrieval: a new era of “natural orifice specimen extraction” (N.O.S.E). Dis Colon Rectum. 2008;51:1120–4.
Leroy J, Costantino F, Cahill RA, et al. Laparoscopic resection with transanal specimen extraction for sigmoid diverticulitis. Br J Surg. 2011;98:1327–34.
Akamatsu H, Omori T, Oyama T, et al. Totally laparoscopic sigmoid colectomy: a simple and safe technique for intracorporeal anastomosis. Surg Endosc. 2009;23:2605–9.
Franklin ME Jr, Kelley H, Kelley M, et al. Transvaginal extraction of the specimen after total laparoscopic right hemicolectomy with intracorporeal anastomosis. Surg Laparosc Endosc Percutan Tech. 2008;18:294–8.
Knol J, D’Hondt M, Dozois EJ, Vanden Boer J, Malisse P. Laparoscopic-assisted sigmoidectomy with transanal specimen extraction: a bridge to NOTES? Tech Coloproctol. 2009;13:65–8.
Inoue Y, Noro H, Komoda H, et al. Completely laparoscopic total colectomy for chronic constipation: report of a case. Surg Today. 2002;32(6):551–4.
Wolthuis AM, Meuleman C, Tomassetti C, et al. Laparoscopic sigmoid resection with transrectal specimen extraction: a novel technique for the treatment of bowel endometriosis. Hum Reprod. 2011;26:1348–55.
Msika S, Iannelli A, Flamant Y, Hay JM. Laparoscopic sigmoid colectomy with intracorporeal hand-sewn anastomosis. Surg Endosc. 2000;14:866.
Park JS, Choi GS, Kim HJ, Park SY, Jun SH. Natural orifice specimen extraction versus conventional laparoscopically assisted right hemicolectomy. Br J Surg. 2011;98:710–5.
Nishimura A, Kawahara M, Suda K, et al. Totally laparoscopic sigmoid colectomy with transanal specimen extraction. Surg Endosc. 2011;25:3459–63.
Grams J, Tong W, Greenstein AJ, Salky B. Comparison of intracorporeal versus extracorporeal anastomosis in laparoscopic-assisted hemicolectomy. Surg Endosc. 2010;24:1886–91.
Franklin ME Jr, Liang S, Russek K. Natural orifice specimen extraction in laparoscopic colorectal surgery: transanal and transvaginal approaches. Tech Coloproctol. 2013;17(Suppl 1):S63–7.
Bucher P, Wutrich P, Pugin F, et al. Totally intracorporeal laparoscopic colorectal anastomosis using circular stapler. Surg Endosc. 2008;22:1278–82.
Makela J, Kivniemi H, Laitinene S. Risk factors for anastomotic leakage after left-sided colorectal resection with rectal anastomosis. Dis Colon Rectum. 2003;46(5):653–60.
Ooi BS, Quah HM, Fu CW, Eu KW. Laparoscopic high anterior resection with natural orifice specimen extraction (NOSE) for early rectal cancer. Tech Coloproctol. 2009;13:61–4.
Machado M, Nygren J, Goldman S, Ljungqvist O. Similar outcome after colonic pouch and side-to-end anastomosis in low anterior resection for rectal cancer: a prospective randomized trial. Ann Surg. 2003;238:214–20.
Fabozzi M, Allieta R, Contul RB, et al. Comparison of short- and medium-term results between laparoscopically assisted and totally laparoscopic right hemicolectomy: a case-control study. Surg Endosc. 2010;24: 2085–91.
Wolthuis AM, de Buck van Overstraeten A, D’Hoore A. Laparoscopic natural orifice specimen extraction-colectomy: a systematic review. World J Gastroenterol. 2014;20:12981–92.
Costantino FA, Diana M, Wall J, et al. Prospective evaluation of peritoneal fluid contamination following transabdominal vs. transanal specimen extraction in laparoscopic left-sided colorectal resections. Surg Endosc. 2012;26:1495–500.
Disclosure
All authors disclose no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Huang, CC., Chen, YC., Huang, CJ. et al. Totally Laparoscopic Colectomy with Intracorporeal Side-to-End Colorectal Anastomosis and Transrectal Specimen Extraction for Sigmoid and Rectal Cancers. Ann Surg Oncol 23, 1164–1168 (2016). https://doi.org/10.1245/s10434-015-4984-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4984-3