Abstract
Purpose
The prognosis of peritoneal carcinomatosis (PC) from colorectal cancer has been improved with cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC). However, benefits of postoperative chemotherapy (CT) are unclear.
Methods
This retrospective, multicenter study included 231 patients treated by CRS and HIPEC for isolated PC of colon cancer in four expert’s centers. Overall survival (OS), progression-free survival (PFS), and peritoneal recurrence-free survival (PRFS) were compared between patients with adjuvant CT (started within 3 months after surgery) and patients with surveillance only.
Results
After exclusion of 10 patients for early postoperative death (4 %), 221 patients were included (CT group: n = 151; surveillance group: n = 70). Main postoperative CT regimens (median of 6 cycles) were Folfox (28 %), Folfiri bevacizumab (24.5 %), Folfiri (16 %), and Folfiri cetuximab (12.5 %). The median OS after surgery was 43.3 months with no difference between CT and surveillance groups. In multivariate analysis, a low peritoneal cancer index (p < 0.0001) and a long delay between diagnosis of CP and HIPEC (p = 0.001) were associated with increased OS. The median PFS and PRFS were 12.4 and 17 months, respectively. At 1 year, more patients were without progression (p = 0.001) or PC recurrence (0.0004) in the CT group, but with prolonged follow-up this difference was no longer significant.
Conclusions
Early postoperative CT does not improve OS after CRS and HIPEC for colon carcinomatosis. However, a transient effect on PFS and PRFS was observed. A subgroup of patients who may benefit more from CT remain to be defined.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Peritoneal carcinomatosis (PC) is a common metastatic location in colorectal cancer.1 Despite new chemotherapy regimens and improvement in survival in colorectal metastatic cancer, prognosis of patients with PC remains poor with approximately 1 year survival even in recent series.2–5 However, in selected patients, complete cytoreductive surgery (CRS) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) has been proven to improve survival.6–10 Prognostic factors currently accepted are the extent of the peritoneal disease, the absence of synchronous extraperitoneal metastasis, and the completeness of the peritoneal carcinomatosis resection.9 To date, the impact of postoperative systemic chemotherapy after CRS and HIPEC is still controversial. Two large studies have suggested a potential interest of this therapeutic approach.9,10 However, chemotherapy was either used in adjuvant or palliative attempt with insufficient data upon treatment modalities in both series. The purpose of our work was to study in a large cohort the effect of postoperative chemotherapy after complete cytoreduction and HIPEC for isolated synchronous or metachronous PC from colon cancer.
Patients and Methods
Patient Population
This multicenter study was conducted in four expert surgical units. The files of all patients who underwent CRS and HIPEC from January 2004 to December 2012 were retrospectively reviewed. Inclusion criteria were histologically proven colon cancer, isolated synchronous or metachronous PC at time of surgery, CRS whatever the peritoneal carcinomatosis index (PCI), and HIPEC whatever the intraperitoneal drug used. Patients were included in the postoperative CT group if they have received at least one cycle regardless of the regimen within 3 months after surgery. Exclusion criteria were low and mid rectal cancer, CRS alone, and synchronous extraperitoneal metastasis (except from ovarian location). Patients were included in the surveillance group if they did not receive postoperative CT in adjuvant intent. Patients who died of early postoperative complications were excluded of analysis. Because postoperative CT depends on expert opinion, no informed consent was needed for this retrospective study, as stated by the Ethics Committee.
Statistical Analysis
Quantitative data were reported as median [interquartile range] and qualitative data as number (percentage). Characteristics of patients were compared between postoperative CT group and surveillance group using Wilcoxon tests for quantitative data and Fisher exact tests for qualitative data. Primary endpoint was overall survival (OS) defined as time from CRS plus HIPEC procedure until death from any cause. Secondary endpoints were progression-free survival (PFS), defined as time from CRS plus HIPEC procedure until relapse regardless of the site or death from any cause, and peritoneal recurrence-free survival (PRFS), defined as time from CRS plus HIPEC procedure until either peritoneal relapse (radiological or histologically proven) or death from any cause.
The effect of post-HIPEC CT and other potential prognostic factors on the three endpoints was assessed using Cox proportional hazards models. As the proportional hazard assumption was clearly violated for effect of postoperative CT group on both PFS and PRFS, model with time-dependent effect (an early effect during the first year and a late effect after first year) were fitted. Moreover, early and late impact of postoperative CT was assessed using restricted mean PFS and restricted mean PFRS, with restriction at 1, 2, and 3 years. Finally, a qualitative interaction between chemotherapy effect and PCI was searched using the Gail and Simon test.
Results
Patient’s Characteristics
During the study period, 231 patients (women 53 %; median age 56 years) were included. Primary tumors were mainly well or moderately differentiated (90 %), T3/T4 stage (97 %), with positive node (76 %). PC was mainly synchronous (55 %). In case of metachronous PC, the mean time between colon cancer diagnosis and PC occurrence was 19 months. Twenty-three patients (10 %) presented nonovarian extraperitoneal metastasis before CP surgery leading to hepatic resection (n = 12) or resection of various sites (n = 11). Sixty-six patients (28 %) presented ovarian metastasis leading to resection before CP surgery in 32 cases. Patients in CT or Surveillance group were comparable in clinical or in tumor’s characteristics (Table 1). There was only a trend for more women and for more N1/N2 tumors in the surveillance group.
Preoperative Regimens
A total of 127 patients (55 %) received adjuvant CT after colon cancer resection with 5FU alone or FOLFOX regimen (Leucovorin, 5FU bolus, and Oxaliplatin at day 1 followed by infusional 5FU for 2 consecutive days every 2 weeks), in almost all cases (n = 120; 94 %). A total of 177 patients (77 %) received also a neoadjuvant regimen with at least one chemotherapy cycle within 3 months prior to CRS and HIPEC with a median number of 6 cycles (IQR: 4–8 cycles). Neoadjuvant chemotherapy regimens were based on fluoropyrimidines combined with irinotecan (59 %) or oxaliplatin (40 %) or both (1 %). Response or stability was achieved in 87 % of cases assessed by local CT scan according to RECIST 1.1 criteria or surgical evaluation.
HIPEC and Adjuvant Chemotherapy Regimens
All patients had CC0 resection. HIPEC was conducted through an open abdominal procedure in 125 patients (54 %) and a closed abdominal procedure in 106 patients (46 %) according to local practice of each surgical center.
Ten patients (4 %) died postoperatively. The causes of death were septic shock (n = 3), hemorrhagic shock (n = 3), multiorgan failure (n = 2), respiratory distress syndrome (n = 1), and pulmonary bronchospasm (n = 1). At all, 151 patients received postoperative chemotherapy (CT group) and were compared to the remaining 70 patients who did not received postoperative chemotherapy. Both groups were comparable regarding demographic, neoplastic and surgical characteristics. Chemotherapy characteristics are listed in Table 2.
Among the 151 patients, 50 (53 %) needed dose reduction or chemotherapy stopping according to toxicity (Common toxicity Criteria (CTC) of at least grade 3): combined toxicities (22 %), gastrointestinal disorders (20 %), neuropathy (18 %), hematological (16 %), and unknown in 24 % of the cases.
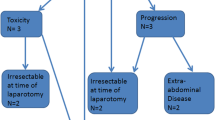
Among the 151 patients, 48 % (n = 73) received perioperative chemotherapy using the same protocol in neoadjuvant and adjuvant settings. In the 70 patients of the surveillance group, the reasons for nonprescription of postoperative CT were medical decision according to the local multidisciplinary team choice on a case-by-case basis due to the lack of evidence-based national consensus (n = 38; 60 %), delay to recover from surgery (n = 14; 22 %; Clavien–Dindo score ≥III: n = 7), patient’s choice (n = 7; 10 %), and early tumor recurrence (n = 5; 8 %); data were missing in 6 patients. During follow-up, 176 patients relapsed (missing data: n = 7) requiring reintroduction of a systemic CT in 81 % of cases (n = 142).
Survival
The median OS of the entire cohort (n = 231) was 43.3 months, with an OS of 58 % [50–66 %] at 3 years and 34 % [25–45 %] at 5 years. No significant difference was observed between the postoperative CT group and the surveillance group with median OS of 49 versus 43 months, respectively (p = 0.93; Fig. 1). An elevated PCI and a shorter duration between colon cancer diagnosis and CRS with HIPEC was independent predictor of shorter OS (Table 3). Survivals are presented in Fig. 2.
Median PFS and median PRFS in the whole population were 12.4 and 17 months, respectively. Median PFS and median PRFS in the postoperative chemotherapy group were 13 and 19 months, respectively. Median PFS and median PRFS in the surveillance group were 10 and 14 months, respectively. In multivariate analysis, the presence of intra-abdominal lymph node involvement at the time of CRS and extended PC were significantly associated with poorer PFS. An elevated PCI and a shorter duration between colon cancer diagnosis and CRS with HIPEC were associated with poorer PRFS. At 1 year after surgery, benefit for both PFS and PRFS (HR 0.426, 95 % CI 0.263–0.689, p = 0.001) in the postoperative CT group was observed with an adjusted difference of mean PFS restricted at 1 year of 47 days [95 % CI 17–], (p = 0.002) and 50 days [22–78], (p = 0.00056), respectively. However, this was no longer significant thereafter at 2 and 3 years following HIPEC.
In the chemotherapy group, a separate analysis according to the chemotherapy regimen (oxaliplatin vs. irinotecan-based) also was performed. In those patients (142/151 patients received one or other of these two drugs), there was no significant difference. PFS was 13 months in the oxaliplatin group (n = 62) and 14 months in the irinotecan group (n = 80; p = 0.46) and PRFS was 18 months in the oxaliplatin group and 24 months in the irinotecan group (p = 0.55).
Among patients who received perioperative CT (less than 3 months before and after HIPEC), a similar regimen for both pre- and post-operative chemotherapy (n = 72) or the modification of postoperative regimen regardless of the reason (n = 44) had no prognostic value for OS (HR = 0.73 [0.37–1.44], p = 0.36), PFS (HR = 0.97 [0.64–1.48], p = 0.89) and PRFS (HR = 0.86 [0.54–1.36], p = 0.51). No evidence of qualitative interaction between effect of postoperative chemotherapy and PCI was found, neither for the early or the late effect.
Discussion
CRS with HIPEC has demonstrated its therapeutic efficacy in colorectal PC.8 While CRS with HIPEC is proven to increase survival, the benefit of adding early postoperative adjuvant CT remains controversial. Our series performed in a highly selected population who underwent complete CRS showed a prolonged survival but with no benefit of chemotherapy in terms of overall survival, PFS, or PRFS.
We report the largest study evaluating the efficacy of postoperative chemotherapy in a population who underwent complete CRS and HIPEC for isolated PC of colon cancer in reference surgical centers. The median OS was 43.3 months with no difference in surveillance and postoperative CT groups. This very prolonged survival is one of the longest observed in patients with PC. This illustrate the high benefit of CRS with HIPEC in highly selected cases as previously reported.11 In our series, two selection criteria can explain these results. First, our study only includes isolated PC and absence of extraperitoneal metastatic site is a widely recognized prognostic factor. Second, we have only included patients with complete cytoreduction, which is known to have a strong impact on survival. In the study by Glehen et al., CT was used after CRS or incomplete resection with inadequate or unspecified CT regimens (5-FU alone: 46 %, unknown or various: 20 %, 5-FU-cisplatin: 17 %, 5-FU with oxaliplatin or irinotecan: 17 %).10 Furthermore, after exclusion of patients deceased of early postoperative death, the OS between postoperative CT group and surveillance group was similar. In the study by Elias et al., postoperative CT was used in different situations (after CRS, incomplete resection or relapse) with no details upon CT modalities.9
Our study found no additional effect of chemotherapy after complete cytoreduction and contrasts with these two large cohorts studies. The beneficial effect in those series may be explained by the benefit of systemic chemotherapy in patients with residual PC or previous extraperitoneal disease.
The median PFS and PRFS were respectively 12.4 and 17 months and also showed no differences in CT and surveillance group. We have only observed a transient benefit at 1 year in the postoperative CT group for both parameters. Apart from our study, three retrospective studies analyzed the specific role of systemic CT in patients who underwent HIPEC. One study have suggested in a cohort of 90 patients that neoadjuvant chemotherapy had no significant prognostic impact whatever the response rate contrarily to adjuvant chemotherapy.12 In a recent study of 73 patients with PC from both colorectal and appendiceal origin, it was observed a better PFS and OS in the CT group versus CRS and HIPEC alone but with no benefit of postoperative CT alone compared to preoperative CT on both PFS and OS.13 Another retrospective study comparing 110 patients who underwent CRS and HIPEC followed by CT with 184 patients non eligible for surgery who had either base supportive care (38 %) or exclusive palliative CT showed a strong increase of OS (38 vs. 9 months) in the combined group.14 Nevertheless, these two groups were not comparable (selected patients with no data on the number of incomplete resection in the combined group, unfit patients for surgery in the CT group). Subsequently, our conclusions in an homogeneous surgical population with well-defined CT modalities cannot be compared with studies with undefined population. We have noticed a better percentage of patient without progression of PC recurrence at 1 year in the postoperative CT group. This could reflect a trend to CT benefit in a subgroup of patients. However, with a median follow-up of 34 months, no additional benefit was observed in postoperative CT group.
As expected, the PCI index was a major prognosis factor significantly correlated with OS, PFS, and PRFS in our cohort. Positive nodal status on colectomy specimen, synchronous, or metachronous occurence of PC and major postoperative complications defined by a Clavien-Dindo score ≥3 were not associated with different OS, PFS, or PRFS.
Interestingly, a long duration between the diagnosis of PC and CRS with HIPEC was also associated with a better OS. More than a higher sensitivity to chemotherapy, it may reflect the fact that the patients with slow tumor growth have a better prognostic by theirselves with a lower rate of recurrence.
Despite the retrospective design of our study, we address special attention to chemotherapy modalities, which are poorly studied in literature to date; the previous cohorts being mainly focused on surgery procedure. We fail to demonstrate a benefit of oxaliplatin- or irinotecan-based postoperative regimen. Folfox is the reference schedule in the adjuvant setting of node-positive colorectal cancer and as perioperative adjunct after complete resection of hepatic metastases contrasting with negative results with Folfiri.15,16 We also have not demonstrated the influence of perioperative CT modifications on outcome. The type of chemotherapy prescribed mainly depends of investigator decision. Postoperative chemotherapy regimen is guided by tumor response (imaging or surgeon evaluation), pathological response, residual toxicities of previous drugs, and number of chemotherapy received before surgery. However, whatever the reason of postoperative CT prescription, we have not observed any difference of various strategies (early modification for poor response to preoperative chemotherapy, same regimen for response, drug withdrawal for toxicity). Impact of targeted therapies has not been evaluated in our cohort because of protocol’s heterogeneity with a subsequent number of patients treated before KRAS and NRAS determination era. However, bevacizumab and cetuximab fail to demonstrate an interest in the adjuvant setting of stage III colorectal cancer predicting poor interest of these drugs after CRS and HIPEC.17–19 It seems confirmed by preliminary data by Chua et al. who showed no benefit of triplet including targeted agents after cytoreduction and HIPEC.14
The main strengths of our study are the inclusion of a large number of patients with complete CRS, precise description of CT regimen, specific analysis of two groups of patients according to their postoperative CT status, and the long duration of follow-up. Yet, several limitations need to be acknowledged. First, this a retrospective study. However, the population analyzed was homogeneous, because all patients were treated in referal HIPEC centers. Second, 80 % of our population (176/221 patients) underwent relapse leading to CT reintroduction in 81 % of cases. The high proportion of treated patients with chemotherapy at progression may partially explain the absence of benefit on OS. Third, we can’t exclude that the relative heterogeneity of CT regimen may lead to underestimate the efficacy of a specific protocol.
A standardised approach remains desperately needed after CRS and HIPEC. Currently, in the absence of evidence-based data, a pragmatic approach according to the regimen and the number of cycles received preoperatively appears useful to decide the best strategy. The establishment of an algorithm modeling various prognostic factors (tumor characteristics including biological profile, chemosensitivity to preoperative CT, histological response, quality of resection, PCI) could help to identify patients eligible for postoperative treatment.20
References
Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010;46:765–81.
Chu DZ, Lang NP, Thompson C, Osteen PK, Westbrook KC. Peritioneal carcinomatosis in nongynecologic malignancy. A prospective study of prognostic factors. Cancer. 1989;63:364–7.
Sadeghi B, et al. Peritoneal carcinomatosis from non-gynecologic malignancies. Cancer. 2000;88:358–63.
Jayne DG, Fook S, Loi C, Seow-Choen F. Peritoneal carcinomatosis from colorectal cancer. Br J Surg. 2002;89:1545–50.
Pelz JO, et al. Evaluation of best supportive care and systemic chemotherapy as treatment stratified according to the retrospective peritoneal surface disease severity score (PSDSS) for peritoneal carcinomatosis of colorectal origin. BMC Cancer. 2010;10:689.
Sugarbaker PH. Peritonectomy procedures. Ann. Surg. 1995;221:29–42.
Sugarbaker PH, et al. Early postoperative intraperitoneal chemotherapy as an adjuvant therapy to surgery for peritoneal carcinomatosis from gastrointestinal cancer: phgroupacological studies. Cancer Res. 1990;50:5790–4.
Verwaal VJ, et al. Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. J Clin Oncol. 2003;21:3737–43.
Elias D, et al. Peritoneal colorectal carcinomatosis treated with surgery and perioperative intraperitoneal chemotherapy: retrospective analysis of 523 patients from a multicentric French study. J Clin Oncol. 2010;28:63–8.
Glehen O, et al. Cytoreductive surgery combined with perioperative intraperitoneal chemotherapy for the management of peritoneal carcinomatosis from colorectal cancer: a multi-institutional study. J Clin Oncol. 2004;22:3284–92.
Elias D, et al. Prognostic similarities and differences in optimally resected liver metastases and peritoneal metastases from colorectal cancers. Ann Surg. 2015;261:157–63.
Passot G, et al. Progression following neoadjuvant systemic chemotherapy may not be a contraindication to a curative approach for colorectal carcinomatosis. Ann Surg. 2012;256:125–9.
Baumgartner JM et al. (2014) Predictors of progression in high-grade appendiceal or colorectal peritoneal carcinomatosis after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann. Surg. Oncol. 22:1–6.
Chua TC, et al. Influence of modern systemic therapies as adjunct to cytoreduction and perioperative intraperitoneal chemotherapy for patients with colorectal peritoneal carcinomatosis: a multicenter study. Ann Surg Oncol. 2011;18:1560–7.
Mitry E, et al. Adjuvant chemotherapy after potentially curative resection of metastases from colorectal cancer: a pooled analysis of two randomized trials. J Clin Oncol. 2008;26:4906–11.
Nordlinger B et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet 2008;371:1007–1016.
Allegra CJ, et al. Phase III Trial assessing bevacizumab in stages II and III carcinoma of the colon: results of NSABP Protocol C-08. J Clin Oncol. 2011;29:11–6.
de Gramont A, et al. Bevacizumab plus oxaliplatin-based chemotherapy as adjuvant treatment for colon cancer (AVANT): a phase 3 randomised controlled trial. Lancet Oncol. 2012;13:1225–33.
Taieb J, et al. Oxaliplatin, fluorouracil, and leucovorin with or without cetuximab in patients with resected stage III colon cancer (PETACC-8): an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15:862–73.
Passot G et al. (2014) Pathological response to neoadjuvant chemotherapy: a new prognosis tool for the curative management of peritoneal colorectal carcinomatosis. Ann Surg Oncol. 21:1–7.
Acknowledgments
The authors thank Isabelle Bonnefoy for all the help provided during the study.
Conflict of interest
The authors declared no conflict of interest of any kind for this study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Maillet, M., Glehen, O., Lambert, J. et al. Early Postoperative Chemotherapy After Complete Cytoreduction and Hyperthermic Intraperitoneal Chemotherapy for Isolated Peritoneal Carcinomatosis of Colon Cancer: A Multicenter Study. Ann Surg Oncol 23, 863–869 (2016). https://doi.org/10.1245/s10434-015-4914-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4914-4