Abstract
Background
The last decade has seen an increasing prevalence of prophylactic mastectomies with decreasing age of patients treated for breast cancer. Data are limited on the prevalence of histopathologic abnormalities in this population. This study aimed to measure the prevalence of histopathologic findings in contralateral prophylactic mastectomy (CPM) and bilateral prophylactic mastectomy (BPM) patients and identify predictors of findings.
Methods
Our institution’s prophylactic mastectomies from 2004 to 2011 were reviewed. Breast specimens with prior malignancies were excluded. Patient factors and pathology reports were collected. Independent predictive factors were identified with univariate and multivariate logistic analysis.
Results
A total of 524 specimens in 454 patients were identified. Malignancy was found in 7.0 % of CPM and 5.7 % of BPM specimens. In CPM patients, ipsilateral lobular carcinoma-in situ [odds ratio (OR) 4.0] and mammogram risk group (OR 2.0) were predictive of malignancy. Age group (OR 1.5), ipsilateral lobular carcinoma-in situ (OR 2.3), and prior bilateral salpingo-oophorectomy (OR 0.3) were predictive of moderate- to high-risk histopathology. Only increasing age group was predictive of increased moderate- to high-risk histopathology in BPM patients (OR 2.3). There were no independent predictors of malignancy in BPM. BRCA status was not predictive in either CPM or BPM.
Conclusions
Patients with lobular carcinoma-in situ in the index breast or high-risk mammograms have a higher prevalence of malignancies. Although BRCA patients may benefit from prophylactic mastectomy, the genetic diagnosis does not increase the prevalence of detecting occult pathology. BPM patients can be counseled about relative risk, where occult pathology increases with age.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
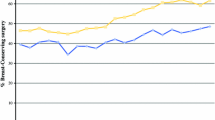
As has been observed nationally, our institution has seen a significant increase in the number of prophylactic mastectomy (PM) procedures. The last decade, we observed a 260 % increase in bilateral breast reconstructions, particularly high-risk patients undergoing PMs.1 Patients pursuing surgery are now on average 6 years younger at our institution. Similarly, patients nationwide are increasingly trying to weigh their cancer risks. With 36 % of BRCA-positive patients in the United States pursuing bilateral prophylactic mastectomy (BPM) and the increasing use of genetic testing, the number of BPMs is likely to continue to rise.2 Patients undergoing BPM are often BRCA mutations carriers or have Li-Fraumeni syndrome, and they are more likely to pursue breast reconstruction.3 However, many patients without a genetic diagnosis are pursuing contralateral prophylactic mastectomy (CPM), as evidenced by the 150 % increase in CPM rates from 1998 to 2003.4 From 2003 to 2010, the percentage of women under 45 years old opting for CPM instead increased from 9.3 to 24.1 %.5 Likely given the 0.6 % per year risk of contralateral breast cancer, younger patients pursue CPM more often, as are those with a cancer history.4 Data are needed to guide patients’, physicians’, and policy makers’ decisions about PMs. With an estimated 232,430 diagnoses of breast cancer in 2013, approximately 10 % of which are in BRCA patients, this topic is timely for many care providers.6
The rate of breast cancer in PM is starting to be elucidated. Most data available are for CPM, with a prevalence of occult malignancies [invasive cancer or ductal carcinoma-in situ (DCIS)] ranging from 2.2 to 5.3 % and moderate- to high-risk lesions (lobular carcinoma-in situ [LCIS], atypical ductal hyperplasia, or atypical lobular hyperplasia) ranging from 12.3 to 18.4 %.7–14 Rai et al. evaluated 301 CPMs and found malignancies in 4.7 % and moderate- to high-risk lesions in 15.0 % of CPMs, with a mean age of 55 years among its patients and 29.9 % with first-degree family history of cancer.11 Age >54 years and lobular histology in the index cancer were independent predictors of malignancies or moderate- to high-risk lesions. Despite varying definitions of family history—with some studies including ovarian cancer, some only breast cancer, and some first-degree relatives versus all relatives—the prevalence of malignancies and moderate- to high-risk lesions is relatively constant. Studies also found higher prevalence of findings in older patients and in those with lobular histopathologic findings in the index breast cancer. Another found estrogen receptor and progesterone receptor positivity in the index cancer to be predictive of contralateral findings.15
Studies evaluating BPM were more varied in their outcomes and only identified age >40 years as predictive of a higher likelihood of findings.16 BRCA-positive patients make up a large percentage of those pursuing BPM, yet no relationship has been found between BRCA status and the occult prevalence of findings. The prevalence of occult malignancies in BPM specimens ranges from 0 to 5.6 % and in moderate- to high-risk lesions from 4.9 to 10.0 %.8–10,16–20 Some prior studies found no predictive factors.7 Nonetheless, patients are increasingly opting for PM despite limited oncologic justification.
This study evaluates the occult histopathology in CPM and BPM specimens at our institution. First, we aimed to determine the prevalence of occult histopathologic findings in CPM and BPM specimens. Second, we hoped to identify independent predictive factors. We hypothesized that the prevalence of occult histopathologic findings would be higher in our institution’s PM patient population than in the general population, and that possible predictors would be BRCA gene mutation, older age, preoperative imaging, and lobular histology in the index cancer.
Methods
Patient Population
The institutional review board approved this study. Medical records of patients who underwent mastectomy between 2004 and 2011 were retrospectively reviewed. A prospectively maintained registry of implant breast reconstructions was used to identify patients undergoing PMs. Inclusion criteria were having listed PM as the procedure in one or both breasts on the operative report and having the PM specimen’s pathology report available in the electronic medical record. PM was defined as a mastectomy of a breast without a prior biopsy suggestive of DCIS or invasive cancer.
Data Collection
The following variables were collected for each patient: age, body mass index (BMI), history of radiotherapy, history of chemotherapy, history of bilateral salpingo-oophorectomy (BSO), BRCA status, family history of breast or ovarian cancer in first- to third-degree relatives, number of breasts treated with PM, preoperative imaging [(mammogram and magnetic resonance imaging (MRI)], and sentinel node biopsy. Preoperative imaging was considered only if done within the year before surgery. Variables were searched in the operative notes, pathology reports, anesthesia records, and office notes for each patient. For patients undergoing CPM, the index breast pathology was categorized into DCIS, invasive ductal carcinoma, or invasive lobular carcinoma. If patients had both invasive ductal carcinoma and invasive lobular carcinoma, only the lobular carcinoma was counted, as it occurs less frequently. The presence of LCIS on the index cancer side was also noted. Patient age was binned into the following age groups: 20–29, 30–39, 40–49, 50–59, and ≥60 years. The surgical pathology reports were reviewed, and the highest-risk lesion for each PM specimen was noted (lowest to highest: normal, atypia, LCIS, DCIS, carcinoma). Mammogram and MRI risks were binned into low, medium, and high depending on each prophylactic breasts recommendation for follow-up on imaging based on the breast imaging reporting and data system (BI-RADS) score. BI-RADS scores of 1 and 2 are low risk, with routine follow-up continued; 3 is medium risk, with short-interval follow-up imaging recommended; 4 and 5 are high risk, with biopsy recommended.
Statistical Analysis
Data were analyzed by STATA 12.1 for Mac (StataCorp, College Station, TX), using α < 0.05 as statistically significant. Univariate logistic regression determined differences between groups defined by categorical variables. χ 2 tests were used to compared demographic variables. Statistical significance of independent predictive factors was confirmed with a multivariate logistic regression (MLR). Given that mammogram findings, MRI findings, and LCIS in the index breast cancer side correlate, only one of the three was included in each MLR analysis. The baseline analysis was done with the mammogram findings. The significance of MRI findings and ipsilateral LCIS was then evaluated using another MLR to adjust for the other variables from the baseline model. The odds ratio calculated by age group represents the change in odds of developing cancer for increase from one age group level to the next.
Results
Histopathologic Findings
A total of 524 specimens in 454 patients met the inclusion criteria. BPM patients were more likely to be BRCA positive, have a family history, and have a prior BSO. CPM patients were more likely to undergo chemotherapy and radiotherapy (Table 1). Two-thirds of patients who underwent CPM had invasive ductal carcinoma as the index cancer, but 20.8 % of CPM patients also had LCIS in the index cancer breast. The characteristics of the occult invasive cancers found are presented in Table 2.
Among the CPM specimens, 7 (1.8 %) had invasive cancer, 20 (5.2 %) had DCIS, 52 (13.5 %) had LCIS, and 82 (21.4 %) had atypia, for a total of 161 (41.9 %) specimens with findings. In univariate analysis, the likelihood of malignancies per specimen increased with each decade of life (P = 0.006), with higher-risk mammogram findings (P = 0.025), and when the index cancer breast had LCIS (P < 0.001) (Table 3). Moderate- to high-risk lesions per CPM also increased with each decade of life (P = 0.007) and if the index breast cancer side had LCIS (P < 0.001) (Table 4). The prevalence decreased in patients with a history of a BSO (P = 0.037). Multivariate analysis confirmed that mammogram findings (P = 0.034) and ipsilateral LCIS were independently predictive of malignancies (P = 0.002), but age group and prior BSO were not (Table 5). When only age group, family history, BSO status, and mammogram findings were in the multivariate model (C-statistic = 0.721), age group reached statistical significance (P = 0.044). For moderate- to high-risk lesions, multivariate analysis inclusive of all variables confirmed that age group (P = 0.018), BSO status (P = 0.035), and ipsilateral LCIS (P = 0.001) were independently predictive of contralateral findings.
In BPM specimens, 3 (2.1 %) had invasive cancer, 5 (3.6 %) had DCIS, 15 (10.7 %) had LCIS, and 28 (20.0 %) had atypia—a total of 36.4 % of specimens. In BPM specimens, there were no predictive factors of malignancy in univariate analysis. Increasing age group was predictive of increasing prevalence of moderate- to high-risk lesions in univariate analysis (P = 0.025), whereas BRCA carriers were less likely to have similar findings (P = 0.001). In multivariate analysis, there were no independently predictive variables for malignancies, and only age group was predictive of findings for moderate- to high-risk lesions.
Across CPM and BPM specimens, those with BRCA mutations had malignancy in 4.9 % of patients, whereas BRCA-negative specimens had malignancies 7.6 % of the time (P = 0.250). Mean age for BRCA-positive patients was 43.2 years compared to 45.5 for non-BRCA-positive patients.
Sentinel nodes were assessed in 14 of the 25 PMs with DCIS, all of which were negative. Eight of ten PM specimens with invasive cancer also underwent sentinel node biopsies, two of which were positive for malignancy.
Discussion
Patients are increasingly seeking proactive ways to reduce their risk of breast cancer, often driven by anxiety over breast cancer risk or recurrence. In patients with LCIS, rates of BPM have recently increased by 50 %.21 Although satisfactory outcomes can be possible after breast reconstruction, prophylactic procedures increase surgical risks, and the decisions to pursue them should be driven by medical necessity. More information is needed regarding the presence of occult histopathologic findings and their predictors in PM. To our knowledge, this is one of the largest studies evaluating PM specimens and predictive factors of occult histopathology, and we present data not easily obtained through national patient registries.
The prevalence of histopathologic findings in CPM and BPM specimens was higher than the general population, as we hypothesized.22 Malignancies in patients of prior reduction mammoplasty studies ranged from 0.3 to 1.0 %, and only 0.6–1.6 % had moderate- to high-risk lesions. The one study that also measured specimen-specific numbers found that 0.3 % had malignancies—significantly lower than our detection of malignancies in 6.7 % of specimens.22–25
The 7.0 % of malignancies in our CPMs are slightly higher compared to previous studies, which range from 2.2 to 5.3 %. The difference could be explained by a difference in patient age, as well as some other components previously found to be predictive, such as estrogen and progesterone receptor positivity, or lobular histology in the index breast. However, our observation of 34.9 % of CPM specimens with moderate- to high-risk lesions is far higher than the 12.3–18.4 % previously reported, perhaps suggestive of a higher-risk population of patients not explained by average age, or perhaps suggesting that the Department of Pathology’s tissue handling and sectioning may have been performed differently at our institution. Our average CPM patient age was 44.9 years; prior studies often had average patient ages of >45 years of age, not younger, suggesting that age alone does not explain the difference.
As reported in other studies, older patients were more likely to have pathologic findings, though our study only reached statistical significance in multivariate analysis for moderate- to high-risk lesions. Only ipsilateral LCIS was predictive of both malignancy and moderate- to high-risk lesions in the CPM, also consistent with prior findings. The finding that prior BSO is associated with a lower likelihood of moderate- to high-risk lesions had not been identified in prior PM studies, but it is consistent with data that suggest that BSO decreases breast cancer risk by up to 50 % in high-risk patients.26
For BPM, prior studies reported malignancies in 0–5.6 % of specimens and moderate- to high-risk lesions in 4.9–10.0 % of specimens, both of which are also lower than our observations of 5.7 and 30.7 %, respectively. The higher rate of detecting malignancies may be somewhat explained by age, as our patients were slightly older, at 44.3 years, whereas only one of the studies we used as a comparison had an average patient age of >41 years. However, the difference in moderate- to high-risk lesions is too large to be simply explained by age, as our odds ratio increase per decade of life was only 2.3.
Our hypothesis that BRCA-positive patients may have higher likelihood of findings was not demonstrated. BRCA-positive malignancies in other studies ranged from 2.7 to 3.0 %, slightly below our 4.9 % of specimens.10,16,17 In our study, BRCA-negative patients had a higher odds ratio of malignancies and moderate- to high-risk lesions, even after adjusting for other variables. However, the difference was not statistically significant. Larger sample sizes will be necessary to settle that question, given that BRCA mutations do increase a patient’s lifetime risk of cancer.
Overall, these findings suggest that patients with LCIS in the index cancer breast have the highest likelihood of malignancies and moderate- to high-risk findings in the contralateral breast, as well as patients with concerning mammogram findings on the CPM side, and thus derive benefit from CPM. Also, although not measured in our study, tamoxifen chemoprevention has also been shown to decrease the risk of breast cancer among BRCA carriers, and it is an alternative to BPM or prophylactic BSO that all patients should also consider.
This study is limited by multiple factors. For one, a small percentage of patients have neoplastic cells in their nipples, so the higher use of nipple-sparing mastectomies at our institution may underestimate the prevalence of histopathologic findings.27 Also, although we defined PM as no history of biopsy-proven DCIS or invasive cancer, given that mastectomy after LCIS is still considered risk reducing, some studies defined it differently—for example, patients with no radiologic or clinical evidence of disease, which may predispose our subjects to a higher prevalence of findings in our study because these were not considered exclusion criteria. Additionally, our registry included patients who underwent immediate prosthetic-based reconstructions and did not include patients who underwent autologous reconstruction or no reconstruction, which potentially skews our findings against patients with higher BMI, the elderly, or those with comorbid medical conditions. The lower BMI of our patients may limit the study’s detection effect on occult breast cancer. Patients with higher BMIs may opt for autologous reconstruction, and older patients more commonly do not opt for reconstruction.28 Both BMI and age can affect breast cancer risk, so this cohort may have slightly different rates of findings.29,30 Rate and method of reconstruction can also vary by surgeon and region, but our institution’s patients mostly undergo immediate, prosthetic-based reconstruction, which is the dominant method in the United States and worldwide, so the findings of this study should still generally be applicable.31
This study provides data on detecting occult pathology after PM, documenting a low incidence for younger patients, where pharmacologic treatment may further reduce risk. In contrast, LCIS is a marker for future breast cancer, and consideration of CPM may be appropriate. Preoperatively, mammogram findings are still critical in helping patients decide whether to pursue CPM. Nonetheless, PM remains a difficult and personal decision for many patients, as it has many physical and psychologic implications that can only be appropriately weighed by individual patients with counsel from their physicians, whom this study aims to inform.
References
Fitzpatrick AM, Gao LL, Smith BL, et al. Cost and outcome analysis of breast reconstruction paradigm shift. Ann Plast Surg. 2014;73:141–9.
Metcalfe KA, Birenbaum-Carmeli D, Lubinski J, et al. International variation in rates of uptake of preventive options in BRCA1 and BRCA2 mutation carriers. Int J Cancer. 2008;122:2017–22.
Metcalfe KA, Semple JL, Narod SA. Satisfaction with breast reconstruction in women with bilateral prophylactic mastectomy: a descriptive study. Plast Reconstr Surg. 2004;114:360–6.
Tuttle TM, Abbott A, Arrington A, Rueth N. The increasing use of prophylactic mastectomy in the prevention of breast cancer. Curr Oncol Rep. 2010;12:16–21.
Pesce CE, Liederbach E, Czechura T, Winchester DJ, Yao K. Changing surgical trends in young patients with early stage breast cancer, 2003 to 2010: a report from the National Cancer Data Base. J Am Coll Surg. 2014;219:19–28.
National Cancer Institute. SEER Stat Facts Sheet. 2014. Available at: http://seer.cancer.gov/statfacts/html/breast.html. Accessed 20 Jan 2014.
Barry PN, Johnson RR, Harkenrider MM, et al. Contralateral prophylactic mastectomy: clinical and pathological features from a prospective database. Am J Med Sci. 2012;344:452–6.
Boughey JC, Khakpour N, Meric-Bernstam F, et al. Selective use of sentinel lymph node surgery during prophylactic mastectomy. Cancer. 2006;107:1440–7.
Heemskerk-Gerritsen BAM, Brekelmans CTM, Menke-Pluymers MBE, et al. Prophylactic mastectomy in BRCA1/2 mutation carriers and women at risk of hereditary breast cancer: long-term experiences at the Rotterdam Family Cancer Clinic. Ann Surg Oncol. 2007;14:3335–44.
Kaas R, Verhoef S, Wesseling J, et al. Prophylactic mastectomy on BRCA1 and BRCA2 mutation carriers: very low risk for subsequent breast cancer. Ann Surg. 2010;251:488–92.
Rai SS, Mahabir RC, Roberts JW, Song J, Hamid KS, White RR. Contralateral prophylactic mastectomy. Ann Plast Surg. 2011;67:215–9.
Schrenk P, Wölfl S, Bogner S, Huemer GM, Huemer G, Wayand W. Symmetrization reduction mammaplasty combined with sentinel node biopsy in patients operated for contralateral breast cancer. J Surg Oncol. 2006;94:9–15.
Soran A, Falk J, Bonaventura M, Keenan D, Ahrendt G, Johnson R. Is routine sentinel lymph node biopsy indicated in women undergoing contralateral prophylactic mastectomy? Magee-Womens Hospital Experience. Ann Surg Oncol. 2006;14:646–51.
Yi M, Meric-Bernstam F, Middleton LP, et al. Predictors of contralateral breast cancer in patients with unilateral breast cancer undergoing contralateral prophylactic mastectomy. Cancer. 2009;115:962–71.
Goldflam K, Hunt KK, Gershenwald JE, et al. Contralateral prophylactic mastectomy. Predictors of significant histologic findings. Cancer. 2004;101:1977–86.
Isern AE, Loman N, Malina J, Olsson H, Ringberg A. Histopathological findings and follow-up after prophylactic mastectomy and immediate breast reconstruction in 100 women from families with hereditary breast cancer. Eur J Surg Oncol. 2008;34:1148–54.
Arver B, Isaksson K, Atterhem H, et al. Bilateral prophylactic mastectomy in Swedish women at high risk of breast cancer: a national survey. Ann Surg. 2011;253:1147–54.
Wickman M, Sandelin K, Arver B. Technical aspects and outcome after prophylactic mastectomy and immediate breast reconstruction in 30 consecutive high-risk patients. Plast Reconstr Surg. 2003;111:1069–77.
Black D, Specht M, Lee JM, et al. Detecting occult malignancy in prophylactic mastectomy: preoperative MRI versus sentinel lymph node biopsy. Ann Surg Oncol. 2007;14:2477–84.
Bunting PW, Cyr AE, Gao F, Margenthaler JA. Sentinel lymph node biopsy during prophylactic mastectomy: is there a role? J Surg Oncol. 2014;109:747–50.
Portschy PR, Marmor S, Nzara R, Virnig BA, Tuttle TM. Trends in incidence and management of lobular carcinoma in situ: a population-based analysis. Ann Surg Oncol. 2013;20:3240–6.
Colwell AS, Kukreja J, Breuing KH, Lester S, Orgill DP. Occult breast carcinoma in reduction mammaplasty specimens: 14-year experience. Plast Reconstr Surg. 2004;113:1984–8.
Ishag MT, Bashinsky DY, Beliaeva IV, Niemann TH, Marsh WL. Pathologic findings in reduction mammaplasty specimens. Am J Clin Pathol. 2003;120:377–80.
Kakagia D, Fragia K, Grekou A, Tsoutsos D. Reduction mammaplasty specimens and occult breast carcinomas. Eur J Surg Oncol. 2005;31:19–21.
Goyal A, Coulson SG, Wu JM, Suvarna SK, Reed MWR, Caddy CM. Occult breast carcinoma in breast reduction specimens in European women. Breast Cancer Res Treat. 2011;128:749–53.
Rebbeck TR, Kauff ND, Domchek SM. Meta-analysis of risk reduction estimates associated with risk-reducing salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers. J Natl Cancer Inst. 2009;101:80–7.
Colwell AS, Gadd M, Smith BL, Austen WG. An inferolateral approach to nipple-sparing mastectomy: optimizing mastectomy and reconstruction. Ann Plast Surg. 2010;65:140–3.
VanderWalde LH, Edge SB. Decision shared or otherwise: the ongoing evolution of local therapy for breast cancer. J Clin Oncol. 2014;32:873–5.
Van den Brandt PA, Spiegelman D, Yaun SS, et al. Pooled analysis of prospective cohort studies on height, weight, and breast cancer risk. Am J Epidemiol. 2000;152:514–27.
Lahmann PH, Hoffman K, Allen N, et al. Body size and breast cancer risk: findings from the European Prospective Investigation into Cancer And Nutrition (EPIC). Int J Cancer. 2004;111:762–71.
Cemal Y, Albornoz CR, Disa JJ, et al. A paradigm shift in US breast reconstruction: part 2. The influence of changing mastectomy patterns on reconstructive rate and method. Plast Reconstr Surg. 2013;131:320e–6e.
Disclosure
Amy S. Colwell is a consultant for LifeCell and Allergan. William G. Austen is a consultant for Mentor. Eric C. Liao is the principal investigator on a research study funded by Musculoskeletal Transplant Foundation. No funds were received for this study. The other authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mattos, D., Gfrerer, L., Ling, I.T.C. et al. Occult Histopathology and Its Predictors in Contralateral and Bilateral Prophylactic Mastectomies. Ann Surg Oncol 23, 767–775 (2016). https://doi.org/10.1245/s10434-015-4896-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4896-2