Abstract
Purpose
Repeat sentinel node biopsy (SNB) is an alternative to axillary lymph node dissection (ALND) for axillary staging in recurrent breast cancer. This study was conducted to determine factors associated with technical success of repeat SNB.
Methods
A total of 536 patients with locally recurrent nonmetastatic breast cancer underwent lymphatic mapping (LM) and repeat SNB in 29 Dutch hospitals.
Results
A total of 179 patients previously underwent breast-conserving surgery (BCS) with SNB, 262 patients BCS with ALND and 61 patients mastectomy, 35 with SNB and 26 with ALND. Another 34 patients underwent breast surgery without axillary interventions. A repeat sentinel node (SN) was identified in 333 patients (62.1 %) and was successfully removed in 235 (53.5 %). The overall repeat SN identification rate was 62.1 %, varying from 35 to 100 % in the participating hospitals. Previous radiotherapy of the breast [odds ratio (OR) 0.16; 95 % confidence interval (CI) 0.03–0.84], subareolar tracer injection (OR 0.34; 95 % CI 0.16–0.73), and a 2-day LM protocol (OR 0.57; 95 % CI 0.33–0.97) after previous BCS were independently associated with failure of SN identification. Injection of a larger amount of tracer (>180 MBq) led to a higher identification rate (OR 4.40; 95 % CI 1.45–13.32).
Conclusions
Repeat SNB is a technically feasible procedure for axillary staging in recurrent breast cancer patients. Previous radiotherapy appears to be associated with failure of SN identification. Injection with a larger amount of tracer (>180 MBq) leads to a higher identification rate; subareolar injection and a 2-day LM protocol after previous BCS appear to be less adequate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Sentinel node biopsy (SNB) is used for axillary staging in clinically node-negative primary breast cancer patients.1 The SNB replaced the standard axillary lymph node dissection (ALND) because its morbidity is much lower and its staging capacities are comparable to ALND.2 In recurrent breast cancer, clinically node-negative patients treated with a SNB during their primary procedure still undergo an ALND according to the current guidelines.1,3 Previous breast cancer treatment with surgery and/or radiotherapy of the breast and axilla could lead to disrupted lymph drainage by scar tissue and fibrosis. However, several recent studies have shown the feasibility of repeat SNB in recurrent breast cancer.4–7 Even after major surgery of the breast and axilla, a repeat SNB can often be visualized. Moreover, the repeat SNB is regarded to be a safe alternative to ALND. After a tumor-negative repeat SNB, axillary recurrence occurred in only 3.9 % of patients in a cohort with 5-year survival data.6 Even after previous ALND, a repeat SNB can still be successfully collected in 61.7 %, most often in aberrant lymph node basins.5 This provides additional staging information, which would otherwise not be available in this subset of patients and might change adjuvant treatment plans.
Although repeat SNB provides us with answers in a majority of the patients, it has led to some new questions that have remained unanswered up to now. Nonvisualization of the SN occurs more often in repeat SNB. In primary breast cancer, the identification rate of the SNB is approximately 97 %.8,9 Repeat SN identification rate is reported to vary between 53 and 93 %.4–6 Visualization of a repeat SNB appears to be greatly influenced by previous treatment of the breast and axilla with surgery and radiotherapy. However, other factors associated with SN identification remain unclear.
From many studies on technical aspects of SNB in primary breast cancer, it is known that injection of a larger amount of radioactively labeled tracer leads to a higher identification rate.10–12 Also, the injection site and the quadrant of the breast in which the tumor is located have been shown to influence the identification and the amount of extra-axillary SN visualization.10,13–15 Dual mapping with technetium-99m (99mTc) and blue dye improves the SN visualization.16 Finally, patients with tumor-positive lymph nodes tend to show a lower SN identification rate.17
In the Dutch multicenter Sentinel Node and Recurrent Breast Cancer (SNARB) study, identification rate, drainage patterns, and technical details on repeat SNB were registered for 536 patients. The aim of this study was to determine technical factors associated with repeat SNB in recurrent breast cancer to improve the identification rate.
Methods
Patients
The SNARB study is a multicenter national registration study in which 36 Dutch hospitals participated (trial TC1450). In the period February 2008 to July 2011, the data of 150 patients with recurrent breast cancer were prospectively entered into our database. Results on the feasibility, validity, aberrant drainage patterns, and clinical consequences of performing repeat SNB in these first 150 patients have been published previously.5 Details on technical success factors have not been described before. From August 2011 to December 2014, data from 386 additional patients were entered into the database retrospectively after their disease was initially staged with repeat SNB outside of this study but according to the study protocol. The collected data we present here were derived from 29 hospitals, consisting of university hospitals, large non–university teaching hospitals, and community hospitals in the Netherlands. The remaining 7 hospitals that participated were not able to include patients because of lack of patients with recurrent breast cancer who fulfilled the inclusion criteria.
Women older than 18 years with operable locally recurrent breast cancer confirmed by cytology and/or histology were included. Exclusion criteria were ipsilateral or contralateral lymph node metastases proven by ultrasound and fine needle aspiration, distant metastases, and a known allergy to 99mTc or blue dye injection fluids.
Technical Procedure
Lymphatic mapping (LM) was carried out according to the local protocol of the participating hospitals, similar to LM in primary breast cancer. 99mTc was injected peritumoral, intratumoral, or periareolar intracutaneous in the quadrant of the tumor, in the subareolar plexus, or in a combination of these injection sites on the day before or the day of the surgery. In patients who previously underwent breast-conserving surgery (BCS), injection of the radiolabeled tracer could be performed at all of the aforementioned injection sites. After previous mastectomy, only intratumoral or peritumoral injection remained possible. Peritumoral injection after previous mastectomy is defined as a superficial tracer injection in the overlying (subcutaneous) tissue around the breast cancer recurrence. Lymphoscintigraphy was performed, and the detected SNs were marked on the skin. In case of nonvisualization of the SN, injection of a second dose of radiolabeled tracer was allowed, or physicians could act in concordance with their local protocol. After induction of anesthesia, blue dye was injected to facilitate identification of the SN. No detailed information on the dose of blue dye used was available for further analysis. During surgery the SN was identified using gamma probe and visualization of blue-colored lymph drainage pathways. An attempt was made to excise all SNs in any lymph node basin identified by lymphoscintigraphy.
Statistical Analysis
Differences in surgical management of the primary tumor and differences in repeat SN identification rates were compared by the χ 2 test. A logistic regression analysis was performed that included the following factors to assess their ability to predict the visualization of the SN: previous type of surgery of the breast (BCS vs. mastectomy) and axilla (SNB vs. ALND), use of adjuvant radiotherapy for the primary tumor, and amount of 99mTc (MBq) and the 1- versus 2-day LM protocol. For the amount of 99mTc, a cutoff point of 180 MBq was used. A P value of >0.05 was considered statistically significant. We calculated odds ratios (OR) and their 95 % confidence intervals (95 % CI). A separate logistic regression analysis, stratified for previous breast surgery, was conducted to determine possible differences between previous mastectomy and BCS in SN identification for different 99mTc injection sites. All analyses were performed by SPSS Statistics 22 (IBM, Armonk, NY).
Results
Patients
A total of 536 women with locally recurrent breast cancer were included in this study. Their mean age at the time of diagnosis of recurrent breast cancer was 63.4 years (range 26–93 years). The previous interventions of the breast and axilla in the patient population are shown in Table 1. A total of 179 patients (33.4 %) previously underwent BCS and SNB, and 262 underwent BCS and ALND (48.9 %). In 35 patients (6.5 %) mastectomy and SNB were carried out previously, and in 26 (4.9 %) mastectomy and ALND. Finally, 34 patients (6.3 %) underwent breast surgery without any axillary interventions—for example, in cases of ductal carcinoma-in situ or plastic surgery. Of the 288 patients who underwent an ALND, information on the number of collected lymph nodes was retrieved in 174 patients. The median number of collected lymph nodes per ALND was 13.7, and in 82.1 % of patients 10 or more lymph nodes were collected. Of the 29 hospitals that participated in the SNARB study, the number of included patients per hospital was 1 to 88 patients.
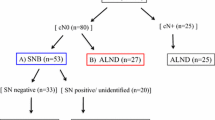
Success Rate and Outcome of Repeat SNB
The success rates of repeat SN identification are shown in Table 1. Overall, a SN was identified in 333 (62.1 %) of 536 patients. Lymphatic drainage on lymphoscintigraphy was observed in 141 (65.9 %) of 214 patients after previous SNB and in 166 (57.6 %) of 288 (P = 0.36) after ALND. Comparing SN identification according to type of previous breast surgery, a SN was identified in 251 (56.9 %) of 441 patients who had undergone BCS and in 56 (91.8 %) of 61 patients (P = 0.02) with previous mastectomy. In 153 patients a SN was visualized in the ipsilateral axilla, and in 143 patients it was found in aberrant sites, outside the ipsilateral axilla. In the 37 remaining patients, SNs were visualized in the ipsilateral axilla as well as in aberrant locations.
A SN was surgically collected in 287 patients (53.5 %), using the dual mapping technique with both 99mTc and blue dye. In 24 of these patients, a SN was difficult to visualize on lymphoscintigraphy but was detected by blue dye only during surgery.
Hospital Variation
A large variation in the SN identification rate was observed between the participating hospitals. Excluding the hospital with small numbers (data from hospitals with <10 included patients not shown), the repeat SN identification rate varied from 35.4 to 100 % (Fig. 1). Major differences in local SN protocols were observed.
The amount of 99mTc injected was 19 to 440 MBq. The injection sites varied widely. In 139 patients (25.9 %) 99mTc was injected peritumorally after BCS, in 54 (10.1 %) peritumorally after mastectomy, in 110 (20.5 %) periareolar and intracutaneous in the quadrant of the tumor, in 70 (13.1 %) intratumorally, and in 59 (11.0 %) subareolarly. Table 2 lists SN identification rates for the different injection sites. Subareolar injection appeared to have a significantly lower identification rate compared to all other injection sites (P < 0.001).
In 350 patients a 1-day lymphoscintigraphy protocol was carried out (65.3 %) and in 151 (28.2 %) a 2-day protocol. In 35 patients (6.5 %) the protocol was not known.
Of the 29 hospitals, 27 (93.1 %) had a single-photon emission computed tomography (SPECT) scanner at their disposal. In 6 hospitals, SPECT was always performed in case of SN nonvisualization. In 9 hospitals, SPECT was never used for this indication. The other hospitals reported that they sometimes used SPECT—when this was expected to aid the surgeon in search of the SN location. A total of 24 hospitals (82.7 %) used cobalt flood sources to outline the patient.
Factors Associated with Technical Success
Logistic regression analysis was performed to determine the factors independently associated with repeat SN identification (Table 3). Although the type of previous breast surgery has a significant impact on SN identification in univariate analysis, logistic regression revealed no significant difference between previous BCS and mastectomy (OR 2.76; 95 % CI 0.51–15.10). Previous axillary surgery did not influence SN identification rate (OR 0.71; 95 % CI 0.46–1.09). Radiotherapy for the treatment of the primary tumor, however, significantly reduced the likelihood of identifying the SN (OR 0.16; 95 % CI 0.03–0.84). Several factors within the LM protocol influenced repeat SN identification rate. Injection of more 99mTc (>180 MBq vs. 0–180 MBq) appeared to result in significantly better identification rates (OR 4.40; 95 % CI 1.45–13.32). Comparing 2-day LM protocol versus 1-day protocols, no significant difference was observed (OR 0.89; 95 % CI 0.56–1.41).
In patients who underwent an ALND as their primary axillary intervention, the amount of lymph nodes previously collected did not influence the identification rate of a repeat SNB.
To determine the effect of different injection sites on SN identification, a separate analysis was performed for previous BCS versus mastectomy because type of previous breast surgery has a major impact on 99mTc injection techniques (Table 4). Stratification for patients who previously underwent mastectomy only did not reveal a significant impact of 99mTc injection sites on the SN identification rate.
In patients after BCS, however, it appeared that subareolar injection led to a lower SN identification rate (OR 0.34; 95 % CI 0.16–0.73) compared to patients who underwent peritumoral tracer injection. Also, in patients who underwent BCS, it appeared that a 2-day protocol led to a lower SN identification rate (OR 0.57; 95 % CI 0.33–0.97).
Discussion
LM and repeat SNB appear to be feasible procedures in recurrent breast cancer.5,6 However, unlike SNB in primary breast cancer, the procedure is technically challenging, and several pitfalls can be encountered. In this series of 536 patients, we found an overall repeat SN identification rate of 62.1 %, which is much lower than the approximately 97 % identification rate of the SNB in primary breast cancer.8,9 Several previous studies described SN identification in recurrent breast cancer, which varied from 55 to 92.5 %.4–6,18,19 A large meta-analysis showed a significantly lower SN identification rate in patients who previously underwent ALND.4
Previous treatment and technical factors of the LM procedure appear to influence repeat SN visualization. Interestingly, we found in multivariate analysis that surgery of the breast and axilla has no significant impact on repeat SN identification rate. Only previous treatment with radiotherapy is strongly associated with a lower identification rate. This discrepancy between univariate and multivariate analysis is most likely explained by the distribution of patients who received radiotherapy between the BCS and mastectomy group. The majority of patients who underwent previous BCS received adjuvant radiotherapy as well, which could explain why BCS is no longer associated with a lower identification rate in the multivariate analysis after adjustment for the use of radiotherapy. Although the number of patients undergoing BCS without adjuvant radiotherapy is small, the effect of radiotherapy is statistically significant and appears to be biologically plausible. The extent of surgically induced scar tissue and damage to the lymph drainage system seems to be larger in patients who underwent mastectomy. Therefore, the administration of radiotherapy in BCS would be a logical explanation of the lower repeat SN identification. In other repeat SN series, radiotherapy has never been independently assessed. However, a study on SN lymphoscintigraphy in patients with previous mantle field irradiation showed a decreased identification rate of 86 % and a higher probability of extra-axillary SNs.20 To our knowledge, this is the first time that the influence of several technical aspects on the success rate of repeat SNB has been studied.
In this study, LM was carried out according to local protocols of the participating centers. With a variation in the identification rate of 35.4 to 100 % between these hospitals, these data suggest that technical differences in LM protocols play a substantial role in the success rate of the procedure. Our multivariate analysis indicated that injection of a larger amount of 99mTc leads to higher SN identification. Also, the data suggest that a 1-day LM protocol might lead to a higher identification rate in patients who previously underwent BCS only. In primary breast cancer, the injection of a larger amount of 99mTc appears to lead to a higher identification rate, which is comparable to our findings in the recurrent breast cancer setting.10–12 In the current European Association of Nuclear Medicine and Society of Nuclear Medicine and Molecular Imaging Guideline on lymphoscintigraphy, a dose of 5 to 30 MBq is considered sufficient in a 1-day LM protocol. For a 2-day protocol in primary breast cancer, injection of 150 MBq 99mTc is advised.21,22 In primary breast cancer, no difference between 1- and 2-day LM protocols has been observed.21 The present study shows the benefit of injection of more 99mTc, with a cutoff point of 180 MBq. Therefore, we advise injection of at least 180 MBq for future repeat SNB procedures. In patients who previously underwent BCS, a 1-day LM protocol could be considered, although the difference is small.
The appropriate injection site of 99mTc primary breast cancer remains a topic of debate. However, the results of several studies have confirmed that the identification of SNs is not affected by the injection method. Superficial injections are easy to perform and show a rapid drainage toward the axillary lymph nodes.22,23 When deep parenchymal injections are used, extra-axillary SNs are visualized more often. Also, this procedure seems to be less painful.22,24,25 Anatomic studies show that the subareolar plexus drains toward the axilla. This is the basis for the rationale on subareolar 99mTc injection for SNB, which is performed in some hospitals. Literature on primary breast cancer patients shows an identification rate of 94.2 % after subareolar tracer injection.26 This is comparable to the identification rates of other deep parenchymal injection sites. In our study on repeat SNB, the subareolar injection of tracer is inferior to other injection sites, with an identification rate of only 32.2 %. Therefore, subareolar injection is not advisable in repeat SNB procedures.
In conclusion, repeat SNB for clinically node-negative recurrent breast cancer is a technically feasible procedure. Previous radiotherapy of the breast appears to reduce SN identification and thereby explains the difference in SN identification after previous mastectomy versus BCS. Subareolar tracer injection and a 2-day LM protocol after BCS leads to lower SN identification rates, so we consider them less adequate. Injection of a larger amount of 99mTc (>180 MBq) leads to higher SN identification. Further research might elucidate the optimal amount of 99mTc that should be injected.
References
NABON. Richtlijn behandeling van het mammacarcinoom. 2012. http://www.oncoline.nl/. Accessed 1 May 2015.
Kim T, Giuliano AE, Lyman GH. Lymphatic mapping and sentinel lymph node biopsy in early-stage breast carcinoma: a metaanalysis. Cancer. 2006;106:4–16.
Burger AE, Pain SJ, Peley G. Treatment of recurrent breast cancer following breast conserving surgery. Breast J. 2013;19:310–8.
Maaskant-Braat AJ, Voogd AC, Roumen RM, Nieuwenhuijzen GA. Repeat sentinel node biopsy in patients with locally recurrent breast cancer: a systematic review and meta-analysis of the literature. Breast Cancer Res Treat. 2013;138:13–20.
Maaskant-Braat AJ, Roumen RM, Voogd AC, Pijpers R, Luiten EJ, Rutgers EJ, et al. Sentinel Node and Recurrent Breast Cancer (SNARB): results of a nationwide registration study. Ann Surg Oncol. 2013;20:620–6.
Intra M, Viale G, Vila J, Grana CM, Toesca A, Gentilini O, et al. Second axillary sentinel lymph node biopsy for breast tumor recurrence: experience of the European Institute of Oncology. Ann Surg Oncol. 2015;22:2372–7.
Roumen RM, Kuijt GP, Liem IH. Lymphatic mapping and sentinel node harvesting in patients with recurrent breast cancer. Eur J Surg Oncol. 2006;32:1076–81.
Lyman GH, Giuliano AE, Somerfield MR, Benson AB 3rd, Bodurka DC, Burstein HJ, et al. American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol. 2005;23:7703–20.
Donker M, van Tienhoven G, Straver ME, Meijnen P, van de Velde CJ, Mansel RE, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014;15:1303–10.
Valdes-Olmos RA, Jansen L, Hoefnagel CA, Nieweg OE, Muller SH, Rutgers EJ, et al. Evaluation of mammary lymphoscintigraphy by a single intratumoral injection for sentinel node identification. J Nucl Med. 2000;41:1500–6.
Heuts EM, van der Ent FW, van der Pol HA, von Meyenfeldt MF, Voogd AC. Additional tracer injection to improve the technical success rate of lymphoscintigraphy for sentinel node biopsy in breast cancer. Ann Surg Oncol. 2009;16:1156–63.
Tanis PJ, van Sandick JW, Nieweg OE, Valdes Olmos RA, Rutgers EJ, Hoefnagel CA, et al. The hidden sentinel node in breast cancer. Eur J Nucl Med Mol Imaging. 2002;29:305–11.
Pelosi E, Bello M, Giors M, Ala A, Giani R, Bussone R, et al. Sentinel lymph node detection in patients with early-stage breast cancer: comparison of periareolar and subdermal/peritumoral injection techniques. J Nucl Med. 2004;45:220–5.
Chakera AH, Friis E, Hesse U, Al-Suliman N, Zerahn B, Hesse B. Factors of importance for scintigraphic non-visualisation of sentinel nodes in breast cancer. Eur J Nucl Med Mol Imaging. 2005;32:286–93.
Shen P, Glass EC, DiFronzo LA, Giuliano AE. Dermal versus intraparenchymal lymphoscintigraphy of the breast. Ann Surg Oncol. 2001;8:241–8.
Cody HS 3rd, Fey J, Akhurst T, Fazzari M, Mazumdar M, Yeung H, et al. Complementarity of blue dye and isotope in sentinel node localization for breast cancer: univariate and multivariate analysis of 966 procedures. Ann Surg Oncol. 2001;8:13–9.
Pelosi E, Ala A, Bello M, Douroukas A, Migliaretti G, Berardengo E, et al. Impact of axillary nodal metastases on lymphatic mapping and sentinel lymph node identification rate in patients with early stage breast cancer. Eur J Nucl Med Mol Imaging. 2005;32:937–42.
Cox CE, Furman BT, Kiluk JV, Jara J, Koeppel W, Meade T, et al. Use of reoperative sentinel lymph node biopsy in breast cancer patients. J Am Coll Surg. 2008;207:57–61.
Port ER, Garcia-Etienne CA, Park J, Fey J, Borgen PI, Cody HS 3rd. Reoperative sentinel lymph node biopsy: a new frontier in the management of ipsilateral breast tumor recurrence. Ann Surg Oncol. 2007;14:2209–14.
van der Ploeg IM, Russell NS, Nieweg OE, Oldenburg HS, Kroon BB, Olmos RA, et al. Lymphatic drainage patterns in breast cancer patients who previously underwent mantle field radiation. Ann Surg Oncol. 2009;16:2295–9.
Gray RJ, Pockaj BA, Roarke MC. Injection of (99m)Tc-labeled sulfur colloid the day before operation for breast cancer sentinel lymph node mapping is as successful as injection the day of operation. Am J Surg. 2004;188:685–9.
Giammarile F, Alazraki N, Aarsvold JN, Audisio RA, Glass E, Grant SF, et al. The EANM and SNMMI practice guideline for lymphoscintigraphy and sentinel node localization in breast cancer. Eur J Nucl Med Mol Imaging. 2013;40:1932–47.
Nieweg OE, Estourgie SH, van Rijk MC, Kroon BB. Rationale for superficial injection techniques in lymphatic mapping in breast cancer patients. J Surg Oncol. 2004;87:153–6.
Noguchi M, Inokuchi M, Zen Y. Complement of peritumoral and subareolar injection in breast cancer sentinel lymph node biopsy. J Surg Oncol. 2009;100:100–5.
Linehan DC, Hill AD, Akhurst T, Yeung H, Yeh SD, Tran KN, et al. Intradermal radiocolloid and intraparenchymal blue dye injection optimize sentinel node identification in breast cancer patients. Ann Surg Oncol. 1999;6:450–4.
Klimberg VS, Rubio IT, Henry R, Cowan C, Colvert M, Korourian S. Subareolar versus peritumoral injection for location of the sentinel lymph node. Ann Surg. 1999;229:860–4.
Acknowledgment
The authors thank the following clinicians for patient recruitment and providing the study data: Mw. Dr. M. Bessems, Mw. Dr. M. F. Ernst, Dr. J. M. Klaase, Dr. F. C. Den Boer, Mw. Drs. S. Muller, Dr. J. E. De Vries, Mw. Dr. A. B. Francken, Mw. J. P. J. Burgmans, Dr. T. Van Dalen, Mw. Dr. L. Jansen, Mw. Drs. C. I.E. Scheeren, Dr. S. A. Koopal, Dr. F. W. C. van der Ent, Mw. Dr. Y. L. J. Vissers, Mw. Dr. M. L. Smidt, Dr. J. W. S. Merkus, Mw. Dr. C. M. E. Contant, Dr. P. H. J. M. Veldman, Dr. R. F. Schmitz, Mw. Dr. E. Linthorst-Niers, Dr. J. R. M. van der Sijp, Dr. O. R. Guicherit, Mw. Dr. M. B. E. Menke-Pluymers, Mw. Dr. L. B. Koppert, Mw. Dr. A. M. Bosch, Dr. L. J. A. Strobbe, Prof. Dr. H. De Wilt, Mw. Drs. M. S. Schlooz-Vries, Mw. Dr. P. G. Boelens, Dr. H. W. P. M. Kemperman, Dr. J. A. van Essen, Dr. J. W. D. de Waard, Dr. B. C. Vrouenraets, and Dr. B. van Ooijen. The authors thank the Dutch Breast Cancer Trialists’ Group (BOOG) for their support in promoting, coordinating, and facilitating the SNARB study. This study was supported by a Grant from the Dutch Cancer Society—KWF (Grant 2009-4466) for data registration and management.
Disclosure
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the Sentinel Node and Recurrent Breast Cancer (SNARB) study group.
Rights and permissions
About this article
Cite this article
Vugts, G., Maaskant-Braat, A.J.G., Voogd, A.C. et al. Improving the Success Rate of Repeat Sentinel Node Biopsy in Recurrent Breast Cancer. Ann Surg Oncol 22 (Suppl 3), 529–535 (2015). https://doi.org/10.1245/s10434-015-4787-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4787-6