Abstract
Background
Papillary lesions of the breast are a relatively rare, but heterogeneous group ranging from benign to atypical and malignant. Debate exists regarding the optimal management of these lesions. In the absence of more accurate risk-stratification models, traditional management guidelines recommend surgical excision, despite the majority of lesions proving benign. This study sought to determine the rate of malignancy in excised breast papillomas and to elucidate whether there exists a population in which surgical excision may be unnecessary.
Methods
A multicenter international retrospective review of core biopsy diagnosed breast papillomas and papillary lesions was performed between 2009 and 2013, following institutional ethical approval. Patient demographics, histopathological, and radiological findings were recorded. All data was tabulated, and statistical analysis performed using Stata.
Results
A total of 238 patients were included in the final analysis. The age profile of those with benign pathology was significantly younger than those with malignant pathology (p < 0.001). Atypia on core needle biopsy was significantly associated with a final pathological diagnosis of malignancy (OR = 2.73). The upgrade rate from benign core needle biopsy to malignancy on the final pathological sample was 14.4 %; however, only 3.7 % had invasive cancer.
Conclusions
This international dataset is one of the largest in the published literature relating to breast papillomas. The overall risk of malignancy is significantly associated with older age and the presence of atypia on core needle biopsy. It may be possible to stratify higher-risk patients according to age and core needle biopsy findings, thereby avoiding surgery on low-risk patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Papillary lesions of the breast are a heterogeneous group encompassing a wide range of lesions ranging from benign to atypical and malignant. Papillomas are proliferative breast lesions and include solitary intraductal papillomas, multiple papillomas, papillomatosis, and juvenile papillomatosis. Pathologically, these lesions are characterized by an intraductal proliferation of epithelial and myoepithelial cells overlying fibrovascular stalks.1 They can be central or peripheral in location and are not always readily detectable on radiological imaging. Women with papillomas often present with either serous or serosanguinous nipple discharge. Historically, papillomas of the breast have fallen under a B3 histological classification or lesion of uncertain clinical significance, based on core biopsy results. In general, these lesions proceed to surgical excision, as solitary papillomas can harbor areas of atypia, carcinoma in situ, or invasive cancer. Radiological imaging while helpful, cannot reliably distinguish between benign and malignant lesions. Recognized as a difficult diagnostic and therapeutic dilemma by Haagensen et al. in 1951, these lesions still present problems today.2 Preliminary data have suggested that benign papillary lesions can be safely followed using a watchful waiting approach in combination with close radiological follow-up.3,4 However, many of these studies have suffered from inadequate sample size. Other studies have suggested that all benign papillary lesions of the breast should be excised, due to the high upgrade rate to atypia or malignancy.5 Hence, the aim of this study was to characterize the malignancy rate in excised breast papillomas in order to ascertain the upgrade rate to malignancy and to determine whether there exists a population, in which these lesions can be managed nonoperatively.
Methods
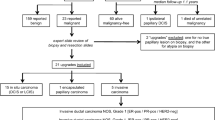
A multicenter, retrospective, institutional review of core needle biopsy diagnosed papillary breast lesions that proceeded to surgical excision was performed. Five institutions took part in the study, namely (1) Cork University Hospital, Cork, Ireland, (2) the Department of Surgical Oncology, University of Toronto, Ontario, Canada, (3) the Department of Surgery, Beaumont Hospital, Dublin, Ireland, (4) the Departments of Breast Surgery, Radiology & Pathology, Victoria Infirmary, Glasgow, United Kingdom, and (5) the Department of Breast and Sarcoma Surgery, National Institute of Oncology, Budapest, Hungary.
Ethical approval was obtained through each institution’s ethical review board. “Papillary breast lesions” encompassed: papillary lesion, papilloma with or without atypia, intraductal papilloma, sclerosing papilloma, and complex papillary lesion. All patients older than 18 years diagnosed with breast papillomas between the years 2009 and 2013 were included. Data collected included basic demographic data and core biopsy pathology along with the final excisional biopsy result. Preoperative radiological imaging findings were recorded. All radiological examinations were reported by dedicated breast radiologists. Pathology was reported in each institution by dedicated breast pathologists. Patients with an incomplete dataset or those with a preoperative diagnosis of cancer or DCIS were excluded. B3 lesions are typically discussed at multidisciplinary meetings in the institutions involved in this study. All data were entered into an Excel spreadsheet initially. All statistical analyses were performed using Stata (version 9.2, StataCorp, LP, College Station, TX). All tests were 2-sided and a p value of <0.05 was considered statistically significant. For comparisons between the final pathology groups, the independent samples t test was used for continuous variables and the Fisher exact test was used for categorical variables. Multiple logistic regression was used to investigate factors associated with a final diagnosis on excisional biopsy of a benign or malignant lesion. Age and core biopsy were included as independent variables in the model.
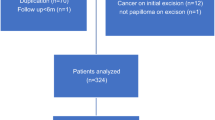
Results
Overall, 238 patients undergoing 247 procedures were identified initially for inclusion; however, seven patients had more than one surgical procedure. For these patients, only one episode was included in order to avoid skewing the data, as there was essentially identical data at two or more separate visits. Therefore, a total of 238 patients (with one procedure per patient) were included in the final analysis. For the purpose of this study, only those patients who proceeded to excisional biopsy were included; therefore, 100 % of patients who underwent core needle biopsy proceeded to definitive surgical excision. Among 188 lesions with core biopsies showing benign papilloma, 27 (14.3 %) were upgraded to malignancy on excision, whereas among 50 lesions with core biopsies showing papillary lesion with atypia, 18 (36 %) were upgraded. Patients who were upgraded were, on average, 10 years older than patients with benign final pathology on excision (Table 1). When the final pathology was subcategorized into benign, atypia, carcinoma in situ, and invasive cancer, age and core biopsy results remained significantly associated with malignancy (p < 0.001) (Table 2). The upgrade rate from benign to atypia on final pathology was 11.2 %, and again, age was seen to be significantly associated with atypia (p < 0.001). Radiological findings for all cases were recorded including ultrasonographic and mammographic findings. The ultrasound and mammographic findings were condensed into groups. Ultrasonographic findings were not statistically different between the benign and malignant final pathology groups. The most common ultrasound finding was a solid lesion, likely benign. The most common mammographic finding in both the benign and malignant final pathology groups was a mass (Table 2). Despite the fact that no lesion with a completely normal ultrasound was upgraded to malignancy, there was no statistically significant correlation between radiological findings and core needle biopsy or final pathology results. Of interest, no patient with a normal mammogram and benign core needle biopsy was upgraded to malignancy; however, five patients with a normal mammogram, but atypia on core needle biopsy, were upgraded to malignancy.
On multivariate analysis, examining the correlation between age, core biopsy, and final pathology results, we found that older age (p < 0.001) and atypia on core biopsy (p = 0.009) were significantly associated with malignant final pathology (Table 3). We did not observe carcinoma in situ in any patient under 35 years of age or invasive cancer in any patient under 50 years of age.
Discussion
This case series of clinical and radiological features, associated with benign and malignant papillary breast lesions, represents one of the largest in the published literature. Papillomas of the breast are extraordinarily diverse clinical entities and account for approximately 1–4 % of findings at core needle biopsy. Breast papillomas can occur anywhere in the ductal system, but tend to favor the terminal ductules, lactiferous sinuses, and peripheries of the ductal system.6 Whereas women with benign duct papillomas have a 1.5–2 times higher incidence of future breast cancer, women with atypia have an approximately 4.3 times higher risk of breast cancer compared with the general population.7–9 Multiple intraductal papillomas, which occur in approximately 10 % of cases of intraductal papillomas, also confer an increased breast cancer risk.6,10 At triple assessment breast clinics, where lesions are examined utilizing the three modalities of clinical, radiological, and cytological features, patients may present with a pathological nipple discharge that may occasionally be reproducible. Nipple smears can sometimes suggest features consistent with an intraductal papillary proliferation. Imaging findings in papillary breast lesions can be as varied as the pathological findings. Mammograms are frequently normal. If present, findings on imaging may be a circumscribed benign appearing mass (often subareolar) or, less commonly, a suspicious cluster of calcifications.11 Multiple papillomas are frequently peripheral and can be bilateral.12 On breast ultrasound, the lesions may be seen as well defined, smooth walled, hypoechoic masses. Alternatively, a dilated duct with or without an intraductal mass or cyst may be visible.13 Imaging can present diagnostic difficulties, as small lesions can be radiologically occult or have equivocal findings, though central papillomas are more likely to be benign.12,14 Interestingly, this study found that in patients without an abnormality on ultrasound imaging, none were upgraded to malignancy on final pathology.
B3 lesions, which are considered benign but are of unknown biological potential, are generally discussed at multidisciplinary team meetings in the institutions involved in this study. The standard treatment of papillary breast lesions which, in general, are classified as B3 lesions on core needle biopsy, is surgical excision of the involved duct. One of the limitations of this study is a lack of data on long-term outcome, as the primary aim was to ascertain the upgrade rate from core biopsy result to final pathology at definitive surgical excision. A further limitation of the study, is the disparity in case numbers from different centers; however, this is balanced against the strength of having an international dataset. Additionally, we do not have information about the clinical presentations of the lesions or the baseline risk of breast cancer in the study patients. Furthermore, core biopsy may miss a neoplastic lesion within the sample being biopsied. Other limitations include lack of data about the needle gauge, lesional size, and concordance with imaging. All data presented here, refers to patients who underwent a definitive surgical procedure for a B3 lesion. This potentially selects out a higher incidence of malignant disease. Another point to mention is that vacuum-assisted biopsy was not being performed in the participating institutions at the time of this study. It is postulated that this could potentially lower the number of surgical procedures for benign papillomas, while the overall upgrade rate may increase as those lesions with suspicious features may proceed preferentially to surgical excision. A recent study showed no difference in the upgrade rate between those with core needle biopsy and vacuum-assisted biopsy, and a further study published in 2011 suggested that regardless of whether patients had a vacuum-assisted biopsy or core needle biopsy, all B3 lesions should proceed to definitive surgical excision.15,16
There is considerable debate as to the optimal management of breast papillomas with benign pathology on core needle biopsy. Disparate reports exist throughout the literature of the upgrade rates from benign papillomas on core biopsy to malignancy on the final pathology. Table 4 contains papers published with larger case series and with variable upgrade rates. Jakate et al. had an overall upgrade rate of 22.5 %, higher than the overall upgrade rate of 18.9 % seen in this study.17 We have shown a low upgrade rate in younger women, suggesting it is reasonable in young women with benign pathology on core needle biopsy to offer radiological follow-up given the low risk of malignancy in this population. On multivariate analysis, we found that older age was independently associated with malignancy and that the odds ratio was equal to 1.07 for each year increase in age. Many studies have found older age to be associated with an increased risk of malignancy at surgical excision, though a recent smaller study did not find any significant difference with age, and this was concordant with one of the larger case series published, in which again, no correlation was found between malignancy and older age.18–22 The largest case series to date did find a statistically significant effect with advancing age, similar to the results seen in this study.23 The differences among these studies as to whether age is a contributing factor to upgrade rate may be accounted for by the actual upgrade rate. Rizzo et al. had an overall upgrade rate to a lesion of greater clinical significance of 28.6 % with age being statistically significant.24 However Fu et al., who found age not to be statistically significant, had a lower upgrade rate of 15.4 % for atypical lesions and 5.9 % for benign lesions.22 Sohn et al. did not find any statistically significant difference in the mammographic findings in those who were upgraded to malignancy, albeit they had low population numbers (n = 34 patients).21 Fu et al., along with others, did not find any statistically significant correlation between radiological findings and malignancy.18,20,22 Some studies have shown watchful waiting to be a reasonable approach, particularly in those who are averse to surgical intervention or in those unfit for surgery.23 However, Rizzo et al. disagree with this approach given the high upgrade rate (26.9 %) they observed when they looked at 234 intraductal papillomas.24 Another study found only a 3 % upgrade rate in benign papillomas (n = 1 of 38) and 17 % in sclerotic papillomas (n = 1 of 6).4 A further study reported a 0 % malignancy upgrade rate in benign papillomas (0 of 49), but an 18.2 % upgrade rate in atypical papillomas (2 of 11).18 In this study the upgrade rate from a benign core biopsy result to a malignant final pathological result was 14.4 %. However, further analysis revealed only 3.7 % of patients with benign core needle biopsy results had invasive cancer on final pathology, and age was a statistically significant factor. Therefore, although the upgrade rate in young women with breast papillomas is low, it is not zero and better proven radiological follow-up tools are necessary before we can fully recommend this option to our patients.
Evidence supporting the excision of breast lesions containing atypia is certainly incontrovertible. MacGrogan et al. showed an upgrade rate from atypical lesions to cancer of 27.7 %.25 The upgrade rate in this series from atypia at core needle biopsy to invasive cancer at final pathology was 18 %, indicating that atypia in papillomas on core needle biopsy warrants excision. Of interest, the latest edition of the WHO classification of breast tumors avoids the term atypical papilloma, instead focusing on the classification of ADH and DCIS within papillomas.26 Breast surgery has been changing rapidly over the last number of years with an increase in conservative surgical management.
The ability to stratify patients with breast papillomas at higher risk of atypia or malignancy into risk categories based on age and adverse pathological features is potentially advantageous. Based on these results, and the results from other large case series in the published literature, all breast papillomas should be excised because of the upgrade rate to a lesion of greater clinical significance. These authors, however, do feel that there is a role for prospective observational trials in younger women with benign core needle biopsy, e.g., in those younger than 35 years, as we found no upgrade to invasive cancer in women of this age; this may allow for more accurate risk stratification of breast papillomas in the future, thereby reducing the need for unnecessary operations. For example, women younger than 35 years could simply be followed with a watchful waiting approach. Optimal imaging in this age group has yet to be defined. In this cohort of patients, those under the age of 35 years were unlikely to have had mammograms, but almost all had ultrasonographic imaging; therefore, we would recommend ultrasound and/or MRI follow-up.
References
Sinn HP, Kreipe H. A brief overview of the WHO Classification of Breast Tumors, 4th edition, focusing on issues and updates from the 3rd edition. Breast Care (Basel), 2013;8:149–54.
Haagensen CD, Stout AP, Phillips JS. The papillary neoplasms of the breast. I Benign intraductal papilloma. Ann Surg. 1951;133:18–36.
Liberman L, Tornos C, Huzjan R, Bartella L, Morris EA, Dershaw DD. Is surgical excision warranted after benign, concordant diagnosis of papilloma at percutaneous breast biopsy? AJR Am J Roentgenol. 2006;186:1328–34.
Syndor MK, Wilson JD, Hijaz TA, Massey HD, Shaw de Paredes ES. Underestimation of the presence of breast carcinoma in papillary lesions initially diagnosed at core-needle biopsy. Radiology. 2007;242:58–62.
Mercado CL, Hamele-Bena D, Oken SM, Singer CI, Cangiarella J. Papillary lesions of the breast at percutaneous core-needle biopsy. Radiology. 2006;238:801–8.
Oyama T, Koerner FC. Noninvasive papillary proliferations. Semin Diagn Pathol. 2004;21:32–41.
Hartmann LC, Sellers TA, Frost MH, et al. Benign breast disease and the risk of breast cancer. N Engl J Med. 2005;353:229–37.
Page DL, Salhany KE, Jensen RA, Dupont WD. Subsequent breast carcinoma risk after biopsy with atypia in a breast papilloma. Cancer. 1996;78:258–66.
Dupont WD, Parl FF, Hartmann WH, et al. Breast cancer risk associated with proliferative breast disease and atypical hyperplasia. Cancer. 1993;71:1258–65.
Al Sarakbi W, Worku D, Escobar PF, Mokbel K. Breast papillomas: current management with a focus on a new diagnostic and therapeutic modality. Int Semin Surg Oncol. 2006;3:1.
http://radiopaedia.org/articles/intraductal-papilloma-of-breast.
Jagmohan P, Pool FJ, Putti TC, Wong J. Papillary lesions of the breast: imaging findings and diagnostic challenges. Diagn Interv Radiol. 2013;19:471–8.
Ganesan S, Karthik G, Joshi M, Damodoron V. Ultrasound spectrum in intraductal papillary neoplasms of breast. Br J Radiol. 2006;79;843–9.
Kestelman FP, Gomes CFA, Fontes FB, Marchiori E. Imaging findings of papillary breast lesions: a pictorial review. Clin Radiol. 2014;69:436–41.
Jakate K, De Brot M, Goldberg F, Muradali D, O’Malley FP, Mulligan AM. Papillary lesions of the breast: impact of breast pathology subspecialization on core biopsy and excision diagnoses. Am J Surg Pathol. 2012;36:544–51.
Londero V, Zuiani C, Linda A, Battigelli L, Brondani G, Bazzocchi M. Borderline breast lesions: comparison of malignancy underestimation rates with 14-gauge core needle biopsy versus 11-gauge vacuum-assisted device. Eur Radiol. 2011;21:1200–6.
Bianchi S, Caini S, Renne G, et al. Positive predictive value for malignancy on surgical excision of breast lesions of uncertain malignant potential (B3) diagnosed by stereotactic vacuum-assisted needle core biopsy (VANCB): a large multi-institutional study in Italy. The Breast. 2011;20:264–70.
Chang JM, Han W, Moon WK, et al. Papillary lesions initially diagnosed at ultrasound-guided vacuum-assisted breast biopsy: rate of malignancy based on subsequent surgical excision. Ann Surg Oncol. 2011;18:2506–14.
Glenn ME, Throckmorton AD, Thomison JB, Bienkowski RS. Papillomas of the breast 15 mm or smaller: 4-year experience in a community-based dedicated breast imaging clinic. Ann Surg Oncol. 2015;24:1133–9.
Cheng TY, Chen CM, Lee MY, et al. Risk factors associated with conversion from nonmalignant to malignant diagnosis after surgical excision of breast papillary lesions. Ann Surg Oncol. 2009;16:3375–9.
Sohn YM, Park SH. Comparison of sonographically guided core needle biopsy and excision in breast papillomas. Clinical and sonographic features predictive of malignancy. J Ultrasound Med. 2013;32:303–11.
Fu CY, Chen TW, Hong ZJ, et al. Papillary breast lesions diagnosed by core biopsy require complete excision. Eur J Surg Oncol. 2012;38;1029–35.
Swapp RE, Glazebrook KN, Jones KN, et al. Management of benign intraductal solitary papilloma diagnosed on core needle biopsy. Ann Surg Oncol. 2013;20:1900–5.
Rizzo M, Linebarger J, Lowe MC, Pan L, Gabram SG, Vasquez L, Cohen MA, Mosunjac M. Management of papillary breast lesions diagnosed on core-needle biopsy: clinical pathologic and radiologic analysis of 276 cases with surgical follow-up. J Am Coll Surg. 2012;214:280–7.
MacGrogan G, Tavassoli FA. Central atypical papillomas of the breast: a clinicopathological study of 119 cases. Virchows Archiv. 2003;443:609–17.
Tan PH, Schnitt SJ, van de Vijver MJ, Ellis IO, Lakhani SR. Papillary and neuroendocrine breast lesions: the WHO stance. Histopathology. 2015;66:761–70.
Ahmadiyeh N, Stoleru MA, Raza S, Lester SC, Golshan M. Management of intraductal papillomas of the breast: an analysis of 129 cases and their outcome. Ann Surg Oncol. 2009;16:2264–9.
Jaffer S, Nagi C, Bleiweiss IJ. Excision is indicated for intraductal papilloma of the breast diagnosed on core needle biopsy. Cancer. 2009;115:2837–43.
Sohn V, Keylock J, Arthurs Z, Wilson A, Herbert G, Perry J. Breast papillomas in the era of percutaneous needle biopsy. Ann Surg Oncol. 2007;14:2979–84.
Disclosure
This study was financially supported by the Aid Cancer Treatment Charity, (ACT) Cork University Hospital, Wilton, Cork, Ireland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Foley, N.M., Racz, J.M., Al-Hilli, Z. et al. An International Multicenter Review of the Malignancy Rate of Excised Papillomatous Breast Lesions. Ann Surg Oncol 22 (Suppl 3), 385–390 (2015). https://doi.org/10.1245/s10434-015-4773-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4773-z