Abstract
Background
Newer multigene molecular profiling assays for breast carcinoma rely heavily on the quantification of genes of proliferation, whereas traditional histological grading reports the mitotic count. The mitotic activity of invasive breast carcinomas may be undervalued; therefore, an evaluation of the prognostic significance of mitotic score in predicting prognosis was performed.
Methods
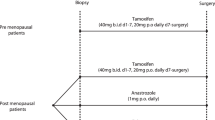
Retrospective analysis of a single institutional cohort of newly diagnosed estrogen receptor positive (ER+), HER2 negative (HER2−) unilateral invasive breast carcinomas was performed. Mitotic scores from the 3-part Nottingham combined histological grade were compared with clinical parameters. Mitoses were counted on Olympus BX50 microscopes and assigned scores of 1–3 based on observed mitoses.
Results
A total of 1292 ER+, HER2− invasive breast carcinoma patients were identified, with a median follow-up time of 2.6 years (range 0–14 years). Higher mitotic score was significantly associated with younger age, larger tumor size, angiolymphatic invasion, node-positive disease, higher stage, and the use of hormonal and cytotoxic chemotherapy. Mitotic score was significant in modeling time to local/regional recurrence (p = 0.02), recurrence-free survival/RFS (p < 0.001), and overall survival/OS (p = 0.01) with higher mitotic scores associated with worse outcomes. Higher mitotic score correlated significantly with intermediate/high risk Oncotype Dx recurrence scores (p = 0.009).
Conclusions
First-generation molecular profiling assays for estrogen receptor positive invasive breast carcinomas derive much of their predictive power from quantifying genes of proliferation into a single score. Sometimes overlooked in the profusion of molecular data, the time-tested, mitotic count in the Nottingham combined histological grade is a good single-parameter predictor of survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The term “breast cancer” encompasses a heterogeneous spectrum of tumors of the breast that vary in their prognosis and optimal treatment. The treatments of these tumors comprise the entire current arsenal of surgical, radiation, endocrine, and chemotherapy. However optimal selection of these treatments is difficult given the variable efficacy of treatment modalities dependent on patient and tumor characteristics, as well as the risks associated with treatment.
Historically, tumor staging for prognosis has consisted of tumor size, lymph node invasion, and histological grade. The histologic grade typically is assessed according to the Scarff-Bloom-Richardson grading system with the Elston–Ellis modification or Nottingham combined histologic grade or Nottingham grading system (NGS).1–3 The NGS has been validated for its prognostic significance through multiple studies and is the recommended grading system by the WHO, AJCC, American College of Pathologists, and Royal College of Pathologists (UK RCPath).4–12 The Nottingham Grading System consists of 3 components: tubule formation, nuclear pleomorphism, and mitotic counts.
Multigene assays, such as Oncotype DX (Genomic Health Inc., Redwood City, CA), are now commonly used to help determine adjuvant treatment. These arrays have shown prognostic significance, yet are they a genetic description of what was already observed underneath the microscope or do they truly present clinicians with new prognostic information?13–16 More aggressive, or high-risk tumors, likely are more mitotically active in their behavior. The mitotic count is a potentially undervalued component of the NGS, often overlooked in an era of advancing genetic testing.
Does the traditional grading system with a focus on mitosis give us prognostic information we can use to treat our patients? We performed a retrospective review to compare outcomes against mitotic counts in patients with estrogen receptor positive breast cancer. We hypothesized that mitotic score can be used to stratify high-risk individuals.
Methods
Patients
After institutional review board approval, a retrospective review was performed of a prospectively collected database of all patients at Mayo Clinic Arizona from 2000 to 2014 with newly diagnosed estrogen receptor positive (ER+), HER2 negative (HER2−) unilateral invasive breast carcinomas with known grade and mitotic rate. Mitotic count was analyzed as the single component of the 3-part Nottingham combined histological score and compared with clinical parameters. Mitotic count was graded and counted on Olympus BX50 microscopes (field diameter 0.55 mm, in 10 high-power [×400] fields) and assigned a mitotic score of 1 (up to 8 mitoses/10 hpf), 2 (9–16 mitoses/10 hpf) or 3 (17 or more mitoses/10 hpf).
Statistical Analysis
Descriptive statistics were used to summarize results by mitotic score category (1–3). Patient demographics, pathology, and treatment variables were compared between categories by analysis of variance (ANOVA) for continuous variables or Chi square tests for categorical variables. Time to local/regional recurrence was defined as the time from primary surgery date to the date of first local or regional recurrence. A patient was censored at last follow-up or death if the patient had not previously experienced a local or regional recurrence. Recurrence-free survival (RFS) included time from primary surgery date to the date of first recurrence (local, regional, or distant) or death from any cause. Overall survival (OS) was calculated as the time from primary surgery date to date of death from any cause. Patients without a recurrence or death event at last follow-up were considered censored for RFS and OS analyses. Event curves were estimated by the Kaplan–Meier method and compared between mitotic groups by the log-rank test. Cox proportional hazards analysis was used to generate hazard ratios (HR) and 95 % confidence intervals for mitotic categories after adjusting for grade and/or progesterone receptor status. A 2-sided p value < 0.05 was considered statistically significant.
Results
During the study period, 1292 ER+, HER2− unilateral primary breast cancers were identified: 1038 had a mitotic score of 1 (80 %), 188 a score of 2 (15 %), and 66 a score of 3 (5 %). Median follow-up for all patients was 2.6 years (range 0–14 years). Patient demographics are shown in Table 1. Patients whose tumors had a mitotic score of 3 were significantly younger compared with those with a mitotic score of 2 or 1 (p = 0.004). The proportion of premenopausal women similarly was highest in the group with a mitotic score of 3 versus 2 or 1 (p = 0.004). Race/ethnicity differed by mitotic score (p < 0.001) with 93.4 % of the group with a mitotic score of 1 being white versus 88.8 and 80.3 % of the groups with mitotic scores of 2 and 3 being white, respectively. There was no difference in mean BMI across the mitotic groups (p = 0.19).
Pathological Associations
Patients with mitotic scores of 2 or 3 were significantly more likely to have invasive ductal carcinoma (p < 0.001), whereas invasive lobular carcinoma and the invasive carcinoma subtypes were more likely to be associated with a low mitotic count. As expected, higher mitotic score was significantly associated with higher grade (p < 0.001), angiolymphatic invasion (p < 0.001), positive lymph nodes (p = 0.002), larger mean tumor size (p < .001), and higher final staging (p < 0.001). No association was seen with progesterone receptor status. Only 85 patients had Oncotype Dx recurrence scores available for evaluation. Mitotic scores of 2 and 3 were associated with intermediate- and high-risk recurrence scores (p = 0.009). Among the 85 patients with Oncotype Dx recurrence scores, no patients with a mitotic score of 1 had a high-risk score and only 1 patient with a mitotic score of 3 had a low-risk score (Table 2).
Presentation and Treatment Associations
Patients with higher mitotic scores were more likely to present on either clinical exam or on self-breast exam (p < 0.001) and were less likely to undergo breast conserving therapy (p = 0.004), which is in line with the finding of larger tumors in this subgroup (Table 3). Patients with higher mitotic scores were also more likely to receive chemotherapy (p < 0.001) and hormonal therapy (p = 0.04). There was no significant difference in use of radiation therapy (p = 0.26) in regard to mitotic score.
Survival Analysis
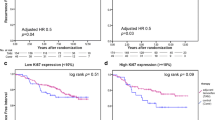
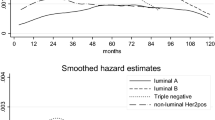
Local/regional recurrence was statistically different among mitotic score categories (Fig. 1a; log-rank p = 0.02; hazard ratio [HR] mitotic score 2 vs 1, 3.08 [95 % CI 1.05–9.01], HR mitotic score 3 vs 1, 4.63 [95 % CI 1.01–21.19]). Difference in local/regional recurrence by grade did not reach statistical significance (log-rank p = 0.07). Patients with higher mitotic scores also had significantly decreased RFS (p < 0.001), as patients with mitotic scores of 1 had a 5 year RFS of 88 %, compared with 76 % for mitotic scores of 2 and 68 % for mitotic scores of 3 (Fig. 1b). Mitotic score of 2 had a HR of 1.86 (95 % CI 1.14–3.03) and mitotic score of 3 had a HR of 2.19 (95 % CI 0.96–4.99) for RFS when compared with the group with a mitotic score of 1, after adjusting for grade and progesterone receptor status. Lower rates of overall survival were found when comparing mitotic scores of 2 or 3 against mitotic scores of 1 (Fig. 1c; p = 0.01). Mitotic score of 2 had a HR of 1.84 (95 % CI, 1.20–2.81) and mitotic score of 3 had a HR of 1.61 (95 % CI 0.71–3.69) for overall survival when compared with the group with a mitotic score of 1.
Discussion
Breast cancer is a heterogeneous disease that requires multi-modality treatment. The clinical question remains how to select patients appropriately for each treatment. A number of factors contribute, but most clinicians rely on the AJCC seventh edition TNM staging and pathologic features to determine risk for recurrence and, thus, treatment recommendations. In order to calculate risk for recurrence, various tools are available, such as Adjuvant!, an online calculator based on population studies utilizing standard patient and pathologic characteristics. More sophisticated tools, such as molecular profiling of the tumor itself, have become more widespread and can provide valuable information, however, at a higher financial cost. In our study, we found that the Nottingham Grading System mitotic count was fairly consistent with the Oncotype DX scores. We had only one outlier, a high mitotic count and low-risk Oncotype DX score, but the number of cases is small and most patients were found to have intermediate- or low-risk Oncotype DX scores in each category. On the other hand, lower mitotic count was found to be significantly associated with improved recurrence-free survival and overall survival.
The initial development and use of the Scarf-Bloom-Richardson system improved clinicians’ insight into individual tumor biology; however, the system was hindered by poor interobserver agreement and score reproducibility.1 Despite these shortcomings, multiple studies still found prognostic significance of the system. The Elston–Ellis modification in 1991 standardized the histopathological methods, and definitions making up the components of the NGS improved reproducibility and interobserver agreement. Multiple studies subsequently have validated the NGS’s prognostic value and its acceptance among multiple health organizations.2,4,5,7–9 Its continued use has been a testament to its ease of use, satisfactory reproducibility, and known prognostic value.17–19 The mitotic score component of the NGS is an undervalued prognostic tool, despite strong evidence and low cost.
Our study has demonstrated that patients with a higher mitotic score present with more aggressive cancers, worse overall prognosis, and shorter recurrence-free survival. We found a significant association between high mitotic score and patients being younger, nonwhite, premenopausal, with angiolymphatic invasion, higher staging, larger mean tumor size, node-positive disease, adjuvant hormonal therapy, and adjuvant cytotoxic chemotherapy. The higher mitotic score was also associated with worse overall survival. Our findings are in agreement with prior studies showing greater prognostic significance of the mitotic score than other components of the NGS.17,20–28 Mirza et al. performed a retrospective literature review of studies of node-negative breast cancer with more than 200 participants and greater than 5-year follow-up and found that mitotic index had prognostic significance in regard to overall survival and disease-free survival.21 In our study, we did not exclude node-positive patients, but found an association between higher mitotic score and likelihood of positive lymph nodes, as expected in more aggressive tumors. A prospective study by Baak et al. of 516 women younger than 55 years with lymph node negative breast cancer found a strong prognostic association with observed mitotic activity index (MAI) less than <3 and greater than 10.27 In their study, the only other component of the NGS with prognostic significance was nuclear atypia, but only among patients with a mitotic activity index less than 10. Interestingly, Baak et al. compared a cutoff of MAI > 10 to a cohort of women from the Multicenter Mammary Carcinoma project with 1–3 positive nodes and found similar survival curves in node-negative women with MAI > 10. The studies looking at specific mitotic counts, however, are impractical as this is not routinely reported. In our study, we looked at mitotic count as reported by the NGS, as it is commonly reported and simple to use. As expected, the mitotic score, a representation of the proliferation of the tumor in question, was found to be independently significant.
We attempted to determine whether mitotic score would correlate with Oncotype DX Recurrence Score. Oncotype DX is a 21-gene RT-PCR assay of ER positive breast cancer that is used to quantify the risk of distance recurrence. Of the genes in question, 16 are grouped into 5 groups: the proliferation group, the HER2 group, the invasion group, the estrogen receptor (including ER and PR) group, and other.29 The other 5 genes are the reference group against which RNA levels are normalized. Recurrence scores classify patients into 3 groups according to 10-year risk of recurrence: low risk (score 0–17, 6.8 % risk of recurrence), intermediate (score 18–31, 14.3 % risk of recurrence), or high risk (score greater than 31, 30.5 % risk of recurrence).29 Most of the information obtained from the Oncotype DX is already detailed in a standard pathology report. The estrogen and progesterone receptor status, the tumor invasion, and the HER2 status can already be obtained by light microscopy and immunohistochemistry. The mitotic score describes the proliferation group, though in a qualitative manner and not quantitative, as the Oncotype DX reports. In our study, we found a statistical association between low mitotic score and Oncotype DX Recurrence Score. Of patients with a known Oncotype DX recurrence score and a mitotic score of 1, no patients had a high recurrence score, though our cohort is limited by the retrospective nature of our study and the selection bias of our institution’s medical oncologists who decide for which patients to order the Oncotype DX Recurrence Score. Several other studies have found similar correlations of low recurrence score based on Nottingham Grade, Ki-67, progesterone receptor positivity, histomorphological components, and the mitotic score of the NGS.30–34 Our results are somewhat limited, due to a small sample size and selection bias, but are suggestive that mitotic score may help guide our decisions as to who may warrant further evaluation with the molecular profiling that is available.
The Nottingham Grading System, particularly the mitotic score component, has valuable prognostic information for providers regarding the tumor characteristics and potential responses to treatment. The individual components of the combined score, detailing each component (tubules, nuclear pleomorphism, and mitotic rate), should always be reported. In an era of genetic testing, where attempts to properly risk-stratify and determine the benefits of adjuvant therapies are made against the risks, the mitotic count is a zero-cost cost marker of cell proliferation. The mitotic count can be used in situations where advanced molecular testing is not available or cost prohibitive, or as another factor that is used to determine which patients may benefit from further molecular testing. The benefit of the mitotic count is that it is data we already have in our hands as we are seeing breast cancer patients, which can help individualize their treatment plans.
References
Bloom HJ, Richardson WW. Histological grading and prognosis in breast cancer; a study of 1409 cases of which 359 have been followed for 15 years. Br J Cancer. 1957;11:359–77.
Elston CW, Ellis IO. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology. 1991;19:403–10.
Elston CW. The assessment of histological differentiation in breast cancer. Aust N Z J Surg. 1984;54:11–5.
Pereira H, Pinder SE, Sibbering DM, et al. Pathological prognostic factors in breast cancer. IV: should you be a typer or a grader? A comparative study of two histological prognostic features in operable breast carcinoma. Histopathology. 1995;27:219–26.
Sundquist M, Thorstenson S, Brudin L, Nordenskjold B. Applying the Nottingham prognostic index to a Swedish breast cancer population. South East Swedish Breast Cancer Study Group. Breast Cancer Res Treat. 1999;53:1–8.
Henson DE, Ries L, Freedman LS, Carriaga M. Relationship among outcome, stage of disease, and histologic grade for 22,616 cases of breast cancer. The basis for a prognostic index. Cancer. 1991;68:2142–9.
Rakha EA, El-Sayed ME, Lee AH, et al. Prognostic significance of Nottingham histologic grade in invasive breast carcinoma. J Clin Oncol. 2008;26:3153–8.
Lundin J, Lundin M, Holli K, et al. Omission of histologic grading from clinical decision making may result in overuse of adjuvant therapies in breast cancer: results from a nationwide study. J Clin Oncol. 2001;19:28–36.
Simpson JF, Gray R, Dressler LG, et al. Prognostic value of histologic grade and proliferative activity in axillary node-positive breast cancer: results from the Eastern Cooperative Oncology Group Companion Study, EST 4189. J Clin Oncol. 2000;18:2059–69.
World Health Organization Classification of Tumors. Pathology and genetics of tumours of the breast and female genital organs. Lyon: IARC Press; 2003.
Fitzgibbons PL, Page DL, Weaver D, et al. Prognostic factors in breast cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med. 2000;124:966–78.
Ellis I, Pinder S, Bobrow L, et al. Pathology reporting of breast disease. Sheffield, London: NHS Cancer Screening Programmes and The Royal College of Pathologists; 2005.
Paik S, Tang G, Shak S, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24:3726–34.
van de Vijver MJ, He YD, van’t Veer LJ, et al. A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med. 2002;347:1999–2009.
Habel LA, Shak S, Jacobs MK, et al. A population-based study of tumor gene expression and risk of breast cancer death among lymph node-negative patients. Breast Cancer Res. 2006;8:R25.
van’t Veer LJ, Dai H, van de Vijver MJ, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415:530–6.
Meyer JS, Alvarez C, Milikowski C, et al. Breast carcinoma malignancy grading by Bloom-Richardson system vs proliferation index: reproducibility of grade and advantages of proliferation index. Mod Pathol. 2005;18:1067–78.
Dalton LW, Page DL, Dupont WD. Histologic grading of breast carcinoma. A reproducibility study. Cancer. 1994;73:2765–70.
Lakhani SR, Jacquemier J, Sloane JP, et al. Multifactorial analysis of differences between sporadic breast cancers and cancers involving BRCA1 and BRCA2 mutations. J Natl Cancer Inst. 1998;90:1138–45.
van Diest PJ, van der Wall E, Baak JP. Prognostic value of proliferation in invasive breast cancer: a review. J Clin Pathol. 2004;57:675–81.
Mirza AN, Mirza NQ, Vlastos G, Singletary SE. Prognostic factors in node-negative breast cancer: a review of studies with sample size more than 200 and follow-up more than 5 years. Ann Surg. 2002;235:10–26.
Mandard AM, Denoux Y, Herlin P, et al. Prognostic value of DNA cytometry in 281 premenopausal patients with lymph node negative breast carcinoma randomized in a control trial: multivariate analysis with Ki-67 index, mitotic count, and microvessel density. Cancer. 2000;89:1748–57.
Volpi A, Bacci F, Paradiso A, et al. Prognostic relevance of histological grade and its components in node-negative breast cancer patients. Mod Pathol. 2004;17:1038–44.
Thor AD, Liu S, Moore DH, 2nd, Edgerton SM. Comparison of mitotic index, in vitro bromodeoxyuridine labeling, and MIB-1 assays to quantitate proliferation in breast cancer. J Clin Oncol. 1999;17:470–7.
Lynch J, Pattekar R, Barnes DM, Hanby AM, Camplejohn RS, Ryder K, Gillett CE. Mitotic counts provide additional prognostic information in grade II mammary carcinoma. J Pathol. 2002;196:275–9.
Medri L, Volpi A, Nanni O, et al. Prognostic relevance of mitotic activity in patients with node-negative breast cancer. Mod Pathol. 2003;16:1067–75.
Baak JP, van Diest PJ, Voorhorst FJ, van der Wall E, Beex LV, Vermorken JB, Janssen EA. Prospective multicenter validation of the independent prognostic value of the mitotic activity index in lymph node-negative breast cancer patients younger than 55 years. J Clin Oncol. 2005;23:5993–6001.
Lende TH, Janssen EA, Gudlaugsson E, et al. In patients younger than age 55 years with lymph node-negative breast cancer, proliferation by mitotic activity index is prognostically superior to adjuvant! J Clin Oncol. 2011;29:852–8.
Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351:2817–26.
Allison KH, Kandalaft PL, Sitlani CM, Dintzis SM, Gown AM. Routine pathologic parameters can predict Oncotype Dx recurrence scores in subsets of ER positive patients: who does not always need testing? Breast Cancer Res Treat. 2012;131:413–24.
Mattes MD, Mann JM, Ashamalla H, Tejwani A. Routine histopathologic characteristics can predict Oncotype DX(TM) recurrence score in subsets of breast cancer patients. Cancer Invest. 2013;31:604–6.
Klein ME, Dabbs DJ, Shuai Y, Brufsky AM, Jankowitz R, Puhalla SL, Bhargava R. Prediction of the Oncotype Dx recurrence score: use of pathology-generated equations derived by linear regression analysis. Mod Pathol. 2013;26:658–64.
Auerbach J, Kim M, Fineberg S. Can features evaluated in the routine pathologic assessment of lymph node-negative estrogen receptor-positive stage I or II invasive breast cancer be used to predict the Oncotype Dx recurrence score? Arch Pathol Lab Med. 2010;134:1697–701.
Zbytek B, Cohen C, Wang J, Page A, Williams DJ, Adams AL. Nottingham-defined mitotic score: comparison with visual and image cytometric phosphohistone H3 labeling indices and correlation with Oncotype Dx recurrence score. Appl Immunohistochem Mol Morphol. 2013;21:48–53.
Conflict of interest
None.
Funding
No discrete funding source.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chang, J.M., McCullough, A.E., Dueck, A.C. et al. Back to Basics: Traditional Nottingham Grade Mitotic Counts Alone are Significant in Predicting Survival in Invasive Breast Carcinoma. Ann Surg Oncol 22 (Suppl 3), 509–515 (2015). https://doi.org/10.1245/s10434-015-4616-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4616-y