Abstract
Background
Although locoregional recurrence is known to affect overall survival for operable breast cancer, the impact of receptor status on locoregional control is debated. Currently, hormone receptor (HR) and human epidermal growth factor receptor-2 (HER2) status are generally not considered relevant to surgical choice. This study examines recent population-level surgical trends with regard to receptor status.
Methods
We used the Surveillance, Epidemiology, and End Results (SEER) data to identify stage I–III female breast cancers diagnosed from 2010 to 2011. Patients were categorized by HR and HER2 receptor status. Univariate and multivariate logistic regressions were used to assess factors associated with undergoing mastectomy and the choice of contralateral prophylactic mastectomy (CPM).
Results
The overall mastectomy rate for the 87,504 women diagnosed in 2010–2011 was 43.4 %. On multivariate analysis, the odds of receiving mastectomy was greater for HER2-positive disease with either HR-negative or HR-positive status, than for women with HER2-negative/HR-positive disease (odds ratio 1.73 and 1. 31, respectively; all p values <0.001). Age, stage, marital status, race, and year of diagnosis also correlated with mastectomy. Triple-negative breast cancer (TNBC) was associated with CPM, while HER2 status was not. The mastectomy rate, which increased overall from 2006 to 2010, has continued to increase for stage III disease but has decreased for stage I disease. Mastectomy rates overall were lower in 2011 than 2010 (p = 0.012).
Conclusions
HER2-positive disease and TNBC were independent predictors of more extensive surgery in this large, recent, population-based cohort. Although mastectomy rates have continued to increase for stage III disease, mastectomy rates overall were lower in 2011 than in previous years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Numerous randomized clinical trials have demonstrated the efficacy of breast-conserving surgery (BCS) compared with mastectomy in early-stage breast cancer.1–6 The 1990 National Cancer Institute consensus statement for early-stage breast cancer states that, given the lower morbidity of BCS it should be considered the treatment of choice for eligible patients, and breast-conservation rate has since been added to the quality measures that cancer institutions report.7 The decision for BCS or mastectomy depends on a variety of factors, including anatomical and surgical considerations, availability of radiation treatment, and patient preference. However, hormone receptor (HR) and human epidermal growth factor receptor-2 (HER2) status are not considered pertinent to the decision by any guidelines.
Nevertheless, there is debate regarding the role of receptor status in local recurrence after breast-conserving therapy. A meta-analysis of 15 studies examining over 12,000 patients found that patients with HER2-positive or triple-negative breast cancer (TNBC) had a significantly higher risk of local recurrence after BCS than those who had HER2-negative/HR-positive disease.8 Although the initial large studies comparing mastectomy and BCS failed to show any survival difference related to in-breast tumor recurrence (IBTR), the Early Breast Cancer Trialists’ meta-analysis found differences in overall survival at 15 years of follow-up related to the prevention of recurrence by radiation therapy, suggesting that IBTR does play a role in long-term survival. Together, this may lead to the perception that patients with TNBC and HER2-positive disease have greater benefit from more extensive surgery.9 A single-institution study of 1194 patients treated in France found a higher mastectomy rate in these patients compared with those with luminal A and B disease, even though IBTR did not differ among the subtypes.10 This study seeks to evaluate surgical trends for stage I–III breast cancer, utilizing recent, population-based information from the Surveillance, Epidemiology, and End Results (SEER) program database.
Methods
Study Participants
Female invasive breast cancer and population data were obtained from SEER. This program includes 18 registries, representing 28 % of the population.11 Women diagnosed in 2010 or 2011 with stage I–III breast cancer who underwent surgery were included. Breast cancer was the first primary malignancy and was required to be pathologically confirmed. The University of Iowa Institutional Review Board approved this study.
Of 94,176 potentially eligible patients, the following were excluded: individuals diagnosed at autopsy or on death certificate (n = 7), men (n = 747), and patients who did not receive surgery (n = 5300) or whose type of surgery was unknown (n = 251). Squamous cell carcinomas, basal cell carcinomas, and sarcomas (n = 367) were also excluded.
Women were categorized as receiving BCS (surgery of primary site variable values of 20–24) and mastectomy (surgery of primary site variable values of 30–80). Patients in the HR-positive subgroup were either estrogen receptor (ER)-positive, progesterone receptor (PR)-positive, or both. Those with borderline ER/PR status were considered ER/PR-positive and those with borderline HER2 were categorized as having missing HER2 status. Patients with TNBC were ER-negative, PR-negative, and HER2-negative. Thus, women were categorized into four, mutually exclusive subtypes: HER2-positive/HR-positive, HER2-positive/HR-negative, HER2-negative/HR-positive, and TNBC. HR status was unavailable for 2344 (2.7 %) women, 4653 (5.3 %) women had missing HER2 information, and 2103 women (2.4 %) had borderline HER2. Contralateral prophylactic mastectomy (CPM) and reconstruction were identified by the surgery of primary site variable. Stage was based on the SEER-adjusted American Joint Committee on Cancer (AJCC), 6th edition. We categorized women into six age groups: <40, 40–49, 50–59, 60–69, 70–79, and ≥80 years. Marital status at the time of diagnosis was categorized into three groups: married, single, and separated. Race was categorized as White, Black, and other, and women were also categorized as Hispanic or not. Finally, individuals were categorized by year of diagnosis.
Statistical Analysis
Univariate and multivariate logistic regressions were used to assess factors associated with undergoing mastectomy and with electing CPM. Receptor status, age, marital status, race and ethnicity, and year of diagnosis were included in the regressions. Reconstruction was included for the CPM analysis, and missing values were dropped from statistical analyses. All tests were two-tailed and p values <0.05 were considered statistically significant. Trend analysis of mastectomy and CPM rates included diagnoses from 2001 to 2011, with the same inclusion and exclusion criteria as above. All analyses used STATA version 12.0 (StataCorp LP, College Station, TX, USA).
Results
In 2010–2011, there were 87,504 women with a first breast cancer who were stage I, II, or III at presentation and who received either BCS or mastectomy (Table 1). The overall mastectomy rate was 43.4 %. Patients with HER2-positive disease and TNBC were more likely to be younger and present at a higher stage than HER2-negative/HR-positive patients.
Univariate Analysis
Univariate analysis by subtype revealed that women with HER2-positive disease, regardless of HR status, and TNBC were significantly more likely to undergo mastectomy than women with HER2-negative/HR-positive tumors (Table 2). Other significant predictors of mastectomy were stage, age, race, marital status, and year of diagnosis.
Multivariate Analysis
On multivariate analysis, subtype remained a significant predictor of mastectomy, although the odds ratios (ORs) were smaller in absolute values than in the univariate analysis (Table 3). ORs of mastectomy for HER2-positive/HR-positive and HER2-positive/HR-negative disease were 1.31 and 1.73, respectively (all p values <0.001). TNBC was no longer significant at the 5 % level (OR 1.05; p = 0.057), and the largest effect size was seen for stage at presentation. Higher-stage disease was associated with a greater likelihood of mastectomy (OR 2.31–8.17; all p values <0.001) compared with stage I breast cancer. Multivariate analysis which included tumor size and nodal involvement, instead of stage, showed similar results, with little or no change in effect size and significance for other covariates (results not shown).
Mastectomy Rates and Contralateral Prophylactic Mastectomy
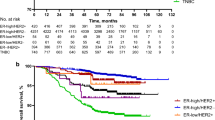
Historical trends for surgery by stage and use of CPM are show in Fig. 1. The overall mastectomy rate decreased from the years 2001–2005, and then increased from the years 2006–2010. In 2011 this rate decreased to 42.8 % compared with 44.0 % in 2010 (p < 0.001). For stage I disease, mastectomy rates have decreased since peaking in 2009 (30.2 % in 2009, 29.0 % in 2011; p = 0.005). There was no significant change in mastectomy rates between 2009 and 2011 for stage II disease (50.6 % in 2009, 49.8 % in 2011; p = 0.165). In contrast, mastectomy rates continue to increase for stage III disease (76.9 % in 2009, 78.8 % in 2011; p = 0.015).
The rate of CPM (for those with unilateral disease who received a mastectomy) has increased markedly since 2001 (7.8 % in 2001, 26.6 % in 2011; p < 0.001). A greater proportion of TNBC and HER2-positive/HR-positive patients elected CPM than HER2-negative/HR-positive patients (28.1 and 27.3 % vs. 24.9 %; p < 0.001). HER2-positive/HR-negative women were no more likely to elect CPM than HER2-negative/HR-positive women. However, on multivariate analysis, HER2 status, regardless of HR status, was not associated with CPM (Table 4). Only women with TNBC remained more likely to elect CPM than HER2-negative/HR-positive patients (OR 1.26; p < 0.001). Women who chose reconstruction were more likely to elect CPM (OR 2.62; p < 0.001).
Discussion
This is the most recent population-based analysis demonstrating a difference in surgical management of breast cancer based on HR status and, to our knowledge, is the first large, population-based study to examine HER2 status as a factor. A review of SEER registry data from the years 2000–2008 found both negative ER and PR status to be predictors of mastectomy, and smaller, single-institution studies have found that mastectomy is performed more often for both HR-negative and HER2-positive patients.10,12
The interaction between receptor status and IBTR has been the subject of a number of studies, and the findings have been inconsistent. A study of 753 patients found no difference in 5-year locoregional recurrence rates by receptor status in women treated with BCS.13 Similar findings were reported in a review of 482 patients.14 Conversely, a study of nearly 3000 patients with over 10-year follow-up found increased IBTR in patients with HER2-positive disease and TNBC.15 A 2011 report involving 1434 patients treated with breast conservation found a significantly higher rate of IBTR in patients who had HER2-positive disease and TNBC;16 however, these patients did not receive targeted anti-HER2 therapy. Other studies, in which contemporary therapy was used, have failed to show differences in recurrence.17,18
Increasingly, local failure is felt to be a function of more aggressive biology, with multiple retrospective analyses showing no difference in locoregional recurrence after mastectomy or BCS in patients with TNBC.19,20 In 2014, the Consensus Guideline on Margins for Breast Conserving Surgery addressed this issue, stating “although there is evidence that the risk of IBTR varies by subtype based on the results of many studies, patients with aggressive tumors remain at equally increased risk for local failure irrespective of treatment with mastectomy or BCS, indicating there is no justification for more widely clear margins over no ink on tumor for any BC subtype”.21
The perception of increased risk for local recurrence is only one of a complex interplay of factors surrounding the surgical decision. Patients with HER2-positive breast cancers are more likely to be younger and present at a higher stage. These clinical characteristics were independently associated with mastectomy in our multivariate analysis, as well as other population-based and single-institution studies.14,17,22 The effect of stage on mastectomy rate is intuitive as tumor size can have obvious implications on surgical options.
SEER registry data cannot account for variables such as patient choice, adjuvant therapy, genetic testing, family history, breast size, multicentricity, and use of magnetic resonance imaging (MRI). In multiple studies, breast MRI has been shown to be associated with a higher mastectomy rate.23–25 In one study of 6072 tumors, HER2-positive breast cancer was found to have a 1.6-fold greater incidence of multifocality than luminal A subtypes, although this has not always been replicated in other series.26,27 TNBC should prompt genetic counseling per National Comprehensive Cancer Network (NCCN) guidelines in patients ≤60 years of age, and genetic testing has also been shown to influence the decision for mastectomy.28,29
In this study, CPM was more likely to be performed in women with TNBC. Although the BRCA status of this population was not available, it is likely that more patients with TNBC had a predisposing mutation as there is a known propensity for BRCA1 carriers to develop basal-type breast cancer.30 A review of SEER registry data from the years 2000–2006 noted that the rates of CPM rose, while the rates of unilateral mastectomy fell, suggesting that in some patients the decision to perform therapeutic mastectomy rather that breast conservation is driven by the desire for CPM.31 This may enlighten our multivariate results, which found that HER2-positive patients disproportionately elect mastectomy (but not CPM) and that TNBC patients disproportionately elect CPM (but not mastectomy).
The findings reported here occur in the context of rising mastectomy rates for all breast cancer in recent years. Both the Moffit Cancer Center and the Mayo Clinic have reported on robust databases of over 5000 patients each, noting increases in mastectomy rates after an initial decrease seen prior to 2004.32,33 A recent review reported an increase in mastectomy rates from 35.6 % in 2005 to 38.4 % in 2008 for SEER patients with T1-2 N0-3 M0 disease.12 This trend is not seen in Europe. A recent report of 15,369 breast cancer patients from the European Society of Breast Cancer Specialists database demonstrated a decline in mastectomies from 38.1 % in 2005 to 13.1 % in 2010.34 Our study noted an increase in mastectomy rates overall from 2006 until 2010, with a slight decrease in 2011, suggesting that the mastectomy rate may have plateaued.
Conclusions
This large, recent, population-based series elucidates the relative role of HR receptor and HER2 status on the current surgical choices for operable breast cancer. Some women may be receiving more extensive surgery based on the perception of increased risk of future disease, locoregional or distant, without clear evidence of survival benefit. As systemic therapies improve, any benefit to more aggressive surgery may become even less apparent. Further study of the complex interactions involved in surgical decision making, as well as better understanding of the benefits and risks of surgical options, would advance care for women with breast cancer.
References
Lichter AS, Lippman ME, Danforth DN Jr, et al. Mastectomy versus breast-conserving therapy in the treatment of stage I and II carcinoma of the breast: a randomized trial at the National Cancer Institute. J Clin Oncol. 1992;10:976–83.
Jacobson JA, Danforth DN, Cowan KH, et al. Ten-year results of a comparison of conservation with mastectomy in the treatment of stage I and II breast cancer. N Engl J Med. 1995;332:907–11.
Poggi MM, Danforth DN, Sciuto LC, et al. Eighteen-year results in the treatment of early breast carcinoma with mastectomy versus breast conservation therapy: the National Cancer Institute Randomized Trial. Cancer. 2003;98:697–702.
Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–41.
van Dongen JA, Voogd AC, Fentiman IS, et al. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst. 2000;92:1143–50.
Arriagada R, Le MG, Rochard F, Contesso G. Conservative treatment versus mastectomy in early breast cancer: patterns of failure with 15 years of follow-up data. Institut Gustave-Roussy Breast Cancer Group. J Clin Oncol. 1996;14:1558–64.
NIH consensus conference. Treatment of early-stage breast cancer. JAMA. 1991;265:391–5.
Lowery AJ, Kell MR, Glynn RW, Kerin MJ, Sweeney KJ. Locoregional recurrence after breast cancer surgery: a systematic review by receptor phenotype. Breast Cancer Res Treat. 2012;133:831–41.
Early Breast Cancer Trialists’ Collaborative Group, Darby S, McGale P, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378:1707–16.
Mazouni C, Rimareix F, Mathieu MC, et al. Outcome in breast molecular subtypes according to nodal status and surgical procedures. Am J Surg. 2013;205:662–7.
Howlader N, Noone AM, Krapcho M, et al. SEER cancer statistics review, 1975-2011. Available at: http://seer.cancer.gov/csr/1975_2011/. Accessed April 2014.
Mahmood U, Hanlon AL, Koshy M, et al. Increasing national mastectomy rates for the treatment of early stage breast cancer. Ann Surg Oncol. 2013;20:1436–43.
Freedman GM, Anderson PR, Li T, Nicolaou N. Locoregional recurrence of triple-negative breast cancer after breast-conserving surgery and radiation. Cancer. 2009;115:946–51.
Haffty BG, Yang Q, Reiss M, et al. Locoregional relapse and distant metastasis in conservatively managed triple negative early-stage breast cancer. J Clin Oncol. 2006;24:5652–7.
Voduc KD, Cheang MC, Tyldesley S, Gelmon K, Nielsen TO, Kennecke H. Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol. 2010;28:1684–91.
Arvold ND, Taghian AG, Niemierko A, et al. Age, breast cancer subtype approximation, and local recurrence after breast-conserving therapy. J Clin Oncol. 2011;29:3885–91.
Gangi A, Chung A, Mirocha J, Liou DZ, Leong T, Giuliano AE. Breast-conserving therapy for triple-negative breast cancer. JAMA Surg. 2014;149:252–8.
Romond EH, Perez EA, Bryant J, et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005;353:1673–84.
Zumsteg ZS, Morrow M, Arnold B, et al. Breast-conserving therapy achieves locoregional outcomes comparable to mastectomy in women with T1-2N0 triple-negative breast cancer. Ann Surg Oncol. 2013;20:3469–76.
Adkins FC, Gonzalez-Angulo AM, Lei X, et al. Triple-negative breast cancer is not a contraindication for breast conservation. Ann Surg Oncol. 2011;18:3164–73.
Moran MS, Schnitt SJ, Giuliano AE, et al. Society of Surgical Oncology–American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. J Clin Oncol. 2014;32:1507-1515.
Jones T, Neboori H, Wu H, et al. Are breast cancer subtypes prognostic for nodal involvement and associated with clinicopathologic features at presentation in early-stage breast cancer? Ann Surg Oncol. 2013;20:2866–72.
Houssami N, Turner R, Morrow M. Preoperative magnetic resonance imaging in breast cancer: meta-analysis of surgical outcomes. Ann Surg. 2013;257:249–55.
Bleicher RJ, Ciocca RM, Egleston BL, et al. Association of routine pretreatment magnetic resonance imaging with time to surgery, mastectomy rate, and margin status. J Am Coll Surg. 2009;209:180–7; quiz 294-185.
Xia C, Schroeder MC, Weigel RJ, Sugg SL, Thomas A. Rate of contralateral prophylactic mastectomy is influenced by preoperative MRI recommendations. Ann Surg Oncol. 2014;21:4133–8.
Wiechmann L, Sampson M, Stempel M, et al. Presenting features of breast cancer differ by molecular subtype. Ann Surg Oncol. 2009;16:2705–10.
Ustaalioglu BO, Bilici A, Kefeli U, et al. The importance of multifocal/multicentric tumor on the disease-free survival of breast cancer patients: single center experience. Am J Clin Oncol. 2012;35:580–6.
Lokich E, Stuckey A, Raker C, Wilbur JS, Laprise J, Gass J. Preoperative genetic testing affects surgical decision making in breast cancer patients. Gynecol Oncol. 2014;134:326–30.
National Comprehensive Cancer Network. Genetic/familial high-risk assessment: breast and ovarian. Available at: http://www.nccn.org/professionals/physician_gls/pdf/genetics_screening.pdf, 2014. Accessed January 2015.
Foulkes WD, Stefansson IM, Chappuis PO, et al. Germline BRCA1 mutations and a basal epithelial phenotype in breast cancer. J Natl Cancer Inst. 2003;95:1482–5.
Habermann EB, Abbott A, Parsons HM, Virnig BA, Al-Refaie WB, Tuttle TM. Are mastectomy rates really increasing in the United States? J Clin Oncol. 2010;28:3437–41.
McGuire KP, Santillan AA, Kaur P, et al. Are mastectomies on the rise? A 13-year trend analysis of the selection of mastectomy versus breast conservation therapy in 5865 patients. Ann Surg Oncol. 2009;16:2682–90.
Katipamula R, Degnim AC, Hoskin T, et al. Trends in mastectomy rates at the Mayo Clinic Rochester: effect of surgical year and preoperative magnetic resonance imaging. J Clin Oncol. 2009;27:4082–8.
Garcia-Etienne CA, Tomatis M, Heil J, et al. Mastectomy trends for early-stage breast cancer: a report from the EUSOMA multi-institutional European database. Eur J Cancer. 2012;48:1947–56.
Disclosures
All authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lizarraga, I., Schroeder, M.C., Weigel, R.J. et al. Surgical Management of Breast Cancer in 2010–2011 SEER Registries by Hormone and HER2 Receptor Status. Ann Surg Oncol 22 (Suppl 3), 566–572 (2015). https://doi.org/10.1245/s10434-015-4591-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4591-3