Abstract
Background
The purpose of this study was to evaluate the diagnostic accuracy of [18F] fluorodeoxyglucose (FDG) positron emission tomography–computed tomography (PET–CT) for lymph node (LN) staging of bladder cancer patients undergoing radical cystectomy (RC) with extended pelvic lymphadenectomy compared to conventional CT.
Methods
A total of 61 patients underwent FDG PET–CT before RC and extended pelvic lymphadenectomy. A template for extended pelvic lymphadenectomy to the level of the inferior mesenteric artery was divided into 11 anatomic nodal packets. Definitive pathologic findings of resected LNs were correlated with the results of FDG PET–CT and CT alone in a patient- and nodal packet-based manner.
Results
Among the 61 patients, pathological staging confirmed LN metastasis in 17 patients (27.9 %). In total, 627 LN packets (2580 LNs) were resected and histologically evaluated. The mean number of LNs removed was 42 (median 40; range 22–118). Of the 627 LN packets removed, 27 packets (4.3 %) were positive for LN metastasis based on pathologic analysis. On a patient-based analysis, FDG PET–CT and conventional CT showed a sensitivity of 47.1 and 29.4 %, respectively, specificity of 93.2 and 97.7 %, respectively, positive predictive value (PPV) of 72.7 and 78.2 %, respectively, and negative predictive value (NPV) of 82.0 and 78.2 %, respectively. On a nodal packet-based analysis, sensitivity, specificity, PPV, and NPV were 14.8, 97.8, 23.5, and 96.2 %, respectively, for PET-CT and 11.1, 98.7, 27.3, and 96.1 %, respectively, for conventional CT.
Conclusions
Combined FDG PET–CT did not improve the diagnostic accuracy of conventional CT for the detection of LN metastasis in bladder cancer patients scheduled for RC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Urothelial carcinoma of the urinary bladder is the fifth most common malignancy in the United States, with an estimated 72,570 new cases and 15,210 deaths in 2013.1 Accurate pretreatment staging of bladder cancer is essential for improving patient care because it allows better selection of patients for systemic treatment or curative surgery. The standard treatment of muscle-invasive bladder cancer with no evidence of distant metastasis is radical cystectomy (RC) with pelvic lymph node (LN) dissection. However, the management of bladder cancer is dependent on LN staging, with more advanced tumors requiring aggressive therapy, such as neoadjuvant chemotherapy.2,3
Current standard staging modalities such as computed tomography (CT) or magnetic resonance imaging (MRI), which depend solely on morphologic characteristics and lesion size, have not proven to be highly accurate in LN staging.4 The diagnostic accuracy of CT and MRI in terms of LN staging is equally low, with reported rates of 55 and 60 %, respectively.5,6
Positron emission tomography (PET) performed with radiopharmaceutical [18F] fluorodeoxyglucose (FDG) is a molecular imaging technique that assesses regional glucose metabolism.7 It is widely used because most cancers exhibit increased glucose utilization compared to normal tissue. Currently available data indicates that combined PET–CT is more sensitive and specific than either of its constituent imaging methods alone and probably more so than images obtained separately from PET and CT and viewed side by side for many different tumor types.8
To date, there are limited and conflicting data regarding the utility of FDG PET–CT in patients scheduled to undergo RC for muscle-invasive bladder cancer. In addition, there are no previous studies with strict “node-to-node” comparison between FDG PET–CT results and pathology data for LN staging because limited LN tissue is removed during pelvic lymphadenectomy.9 – 17 Therefore, there is no firm consensus regarding the role of FDG PET–CT in nonmetastatic muscle-invasive bladder cancer. Here, we performed a prospective study of FDG PET–CT in patients scheduled to undergo RC and extended pelvic lymphadenectomy for bladder cancer with no evidence of metastatic disease on conventional staging modality.
Patients and Methods
Study Design
The study population consisted of 61 consecutive patients with bladder cancer who were scheduled to undergo RC and extended pelvic LN dissection with curative intent. Inclusion criteria were histologically proven high-grade T1 cancer (n = 9) or muscle-invasive (n = 52) bladder cancer. All patients underwent preoperative chest X-ray, conventional CT of the abdomen and pelvis, and bone scan for disease staging, and had no evidence of distant metastasis. Patients with concomitant malignancy as well as those who underwent neoadjuvant chemotherapy were excluded from the study. Patients were also excluded from the data analysis if they did not undergo extended pelvic LN dissection or did not have proven urothelial carcinoma after RC. This prospective study was performed in accordance with the regulations of the local institutional review board and ethics committee, and written informed consent was obtained from all patients before enrollment.
Abdominal CT Protocol and Interpretation
All CT data were obtained using a 64-channel CT scanner (Somatom Plus-S, Siemens Medical System, Erlangen, Germany). Initially, an unenhanced scan was performed from the dome of the diaphragm to the bladder with a section thickness of 5 mm. After obtaining unenhanced CT images, intravenous contrast medium was delivered and corticomedullary phase enhanced images were obtained when the Hounsfield unit of the descending aorta reached 100 with a scan delay of 10 s to allow the kidneys to be covered. A delayed pelvic phase scan was conducted 80 s after the injection to cover the bladder, followed by an excretory phase scan from the liver to the symphysis pubis. The technical parameters of CT imaging at our institute have been previously reported.18 Before surgery, all CT images were prospectively interpreted by a specialist in genitourinary imaging who was blinded to patient clinical characteristics, and the findings were kept on an electronic medical record. LNs were interpreted as positive for metastatic spread on CT scan if their short-axis diameter exceeded 10 mm or if necrosis, independent of size, was noted.
FDG PET–CT Imaging Protocol and Image Processing
FDG PET–CT scanning was performed using a multislice PET-CT camera system with a Biograph Sensation 16, TruePoint 40 (Siemens Medical Systems, Malvern, PA) or Discovery STE, D690 (GE Healthcare, Waukesha, WI). All patients fasted for ≥6 h prior to scanning, and their serum glucose concentration before [18F] FDG administration was below 150 mg/dl (mean 108 mg/dl; range 68–148 mg/dl). Whole body image acquisition was initiated approximately 1 h after intravenous injection of approximately 555 MBq of [18F] FDG. CT without contrast enhancement was performed in a spiral mode from the base of the skull to the proximal thigh for attenuation correction and image fusion, followed by a three-dimensional caudocranial PET emission scan. The emission scan time per bed position was 2–3 min, and 5–6 bed positions were employed. CT results were used for PET attenuation correction and fusion. PET results were reconstructed iteratively without and with attenuation correction based on CT results, and then reoriented in axial, sagittal, and coronal slices. FDG PET–CT images were reviewed on a viewing platform (TureD; Siemens Medical Systems) and AW (GE Healthcare) and interpreted by an experienced nuclear medicine physician blinded to the clinical information. LNs were graded as malignant or benign based on functional criteria (increased metabolism relative to the surrounding LNs and blood pool activity) using a maximal standardized uptake value (SUVmax) of 2.5 as the cutoff value.
Surgery and Histopathologic Evaluation
All operations were performed by a single qualified experienced surgeon (C.S.K.). The standard surgical procedure was RC with extended pelvic LN dissection. Extended pelvic lymphadenectomy was routinely performed, which included bilateral standard pelvic lymphadenectomy template (the distal common iliac, external iliac, hypogastric, obturator, and presacral), as well as LN regions at the level of the proximal common iliac, distal aorta, and vena cava to the level of the inferior mesenteric artery. All nodal tissue removed from each anatomic location was divided into 11 anatomic nodal packets and submitted as a separate packet.
Statistical Analysis
Continuous variables are expressed as the median (and range) or the mean ± SD. Categorical variables are expressed as numbers and percentages. Definitive pathologic findings of resected LN were correlated with the results of FDG PET–CT and CT alone in a patient- and nodal packet-based manner. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of FDG PET–CT and CT were evaluated. All statistical analyses were performed using the SPSS software version 21.0 (IBM, Armonk, NY).
Results
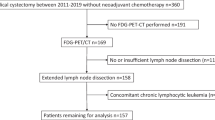
Between June 2009 and April 2012, 69 patients were consecutively enrolled in this study. Patients were prospectively included in the study if histological diagnosis indicated muscle-invasive bladder cancer or high-grade T1 disease on previous transurethral resection. Of the 69 patients, 61 had RC with extended pelvic LN dissection after FDG PET–CT, and these patients were included in the final data analysis (Fig. 1).
Demographic and pathologic characteristics of the patients are shown in Table 1. Most of the patients underwent surgery within a range of 1–25 days (median 6 days) after undergoing FDG PET–CT. Among the 61 patients, pathological staging confirmed LN metastasis in 17 patients (27.9 %). In total, 627 LN packets (2580 LNs) were resected and histologically evaluated. The 11 anatomical LN packets during extended pelvic LN dissection are shown in Fig. 2a. The mean number of LNs removed was 42 with a median of 40 (range 22–118). Of the 627 LN packets removed, 27 packets (4.3 %) showed LN metastasis by pathological analysis. The mean (range) number of LNs removed from each nodal packet and the location of the 27 positive nodal packets are shown in Fig. 2b and c.
The predictive accuracy of FDG PET–CT and that of conventional CT alone are shown in Table 2. On a patient-based analysis, FDG PET–CT and conventional CT showed a sensitivity of 47.1 and 29.4 %, respectively, specificity of 93.2 and 97.7 %, respectively, PPV of 72.7 and 83.3%, respectively, and NPV of 82 and 78.2 %, respectively. On a nodal packet-based analysis, sensitivity, specificity, PPV, and NPV were 14.8, 97.8, 23.5, and 96.2 %, respectively, for FDG PET–CT and 11.1, 98.7, 27.3, and 96.1 %, respectively, for conventional CT.
Based on a patient-based analysis, nodal staging was correctly determined by both FDG PET–CT and CT alone in 44 (72.1 %) of the 61 patients. The remaining 2 (3.3 %) and 16 (26.2 %) of the 61 patients were overstaged or understaged, respectively, on FDG PET–CT. When patients were analyzed by conventional CT alone, 4 (6.6 %) and 13 (21.3 %) of the 61 patients were overstaged or understaged, respectively. The detailed clinical, radiographic, and pathologic characteristics of the 17 LN-positive patients are shown in Table 3.
Discussion
In this study, we found that combined FDG PET–CT did not improve the diagnostic accuracy of conventional CT alone for the detection of LN metastasis in bladder cancer patients scheduled for RC. Although our study included only 61 patients with bladder cancer, to the best of our knowledge, it represents the largest study published on extended pelvic LN dissection and preoperative FDG PET–CT imaging directly comparing to surgically removed LNs (Table 4).
Accurate clinical LN staging can identify patients most likely to benefit from systemic treatment before definitive surgery. Great effort has been made to improve the accuracy of preoperative LN staging before RC using various imaging modalities.4,19 PET–CT is one of these imaging modalities and has undergone explosive growth because of recent technical improvement in PET–CT scanners and the development of better PET tracers.14 However, conflicting data currently exists on the utility of preoperative FDG PET–CT in patients with muscle-invasive bladder cancer. Some studies advocate the use of FDG PET–CT, which has higher sensitivity and equal specificity compared to conventional CT alone.9,12,16 However, other studies do not support the incremental benefit of this imaging modality over conventional CT scan or MRI.10,17 Various factors including patient population, extent of LN dissection, and the staging sequence as well as the interpretation of FDG PET–CT imaging data, such as different cutoff values of standardized uptake value (SUV) to distinguish benign from malignant FDG uptake, may underlie the institutional discrepancies in the diagnostic performance of FDG PET–CT imaging for the detection of LN metastasis.
Removal of regional LNs during RC is important to optimize disease-specific outcomes.20 The extent of LN dissection is one of the most important determinants of the accuracy of imaging for the detection of LN metastasis for several reasons. First, LN dissection according to an extended template with subsequent pathologic evaluation is the gold standard for accurate LN staging. For example, presacral or common iliac LN metastasis cannot be identified using a limited LN dissection template. Second, pelvic LN dissection performed with a limited template or LN sampling for positive findings on preoperative imaging increases the accuracy of FDG PET–CT for LN staging. However, none of the studies that advocate the use of FDG PET–CT for LN staging included patients who had undergone extended pelvic LN dissection during RC.9,12,16
FDG PET–CT for bladder cancer patients who are scheduled to undergo RC can also be used to identify metastatic disease undetectable by conventional imaging, such as CT scan or chest X-ray. In patients planned to undergo curative treatment with RC, surgery can be replaced with systemic chemotherapy based on FDG PET–CT findings. In a study by Apolo et al. 21 % of patients scheduled to receive organ-confined treatment or local radiotherapy for bladder cancer had a change in treatment to metastatic treatment or systemic chemotherapy as a result of FDG PET–CT data.11 However, in this study, we did not detect new metastatic lesions on FDG PET–CT in any patient with no evidence of metastasis on conventional imaging.
In addition to FDG, new PET tracers, such as radio labeled choline and acetate, have been used as tracers in LN staging of patients with bladder cancer prior to undergoing RC and have the advantage of minimal urinary excretion. However, studies showed inconsistent results, likely attributable to small patient populations, nonstandardized LN dissection, and differing patient population with diverse spectrum of disease.21,22 Although a recent study using combined ultrasmall super paramagnetic particles of iron oxide MRI showed an improved detection of metastasis in normal-sized pelvic LNs of bladder cancer in 19 patients with bladder cancer, external validation on a large cohort of bladder cancer patients is needed.19 Further development of more reliable methods for preoperative LN staging in bladder cancer is needed.
Our study results were strengthened by the standardization of patients. All bladder cancer patients undergoing RC with extended pelvic LN dissection at our institute underwent FDG PET–CT before surgery, which eliminates any potential selection bias. Also, because this study was conducted prospectively, all FDG PET–CT imaging findings were interpreted by specialists in genitourinary FDG PET–CT imaging who were blinded to conventional imaging as well as final pathology results.
However, this study has several limitations. First, our study includes a relatively small number of patients and includes patients with LN metastasis. However, to the best of our knowledge, this is the largest study on the use of FDG PET–CT in patients with bladder cancer who underwent extended pelvic LN dissection. Additionally, because there is no specific SUV number that distinguishes between benign and malignant lesions, we choose an SUV of ≥2.5 as the cutoff point according to a previous study on FDG PET–CT.23
In conclusion, our study demonstrates that FDG PET–CT has a low sensitivity for LN staging in muscle-invasive bladder cancer. Combined FDG PET–CT did not improve the diagnostic accuracy of conventional CT alone for the detection of LN metastasis in bladder cancer patients scheduled for RC. Considering the cost, routine use of FDG PET–CT for LN staging of bladder cancer is not recommended. Further studies are needed on the use of other PET tracers and/or the resolution of PET scanners for the LN staging of bladder cancer.
References
American Cancer Society. Cancer facts & figures 2013. Atlanta: American Cancer Society; 2013.
Stein JP, Lieskovsky G, Cote R, et al. Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol. 2001;19:666–75.
Niegisch G, Lorch A, Droller MJ, Lavery HJ, Stensland KD, Albers P. Neoadjuvant chemotherapy in patients with muscle-invasive bladder cancer: which patients benefit? Eur Urol. 2013;64:355–7.
Moses KA, Zhang J, Hricak H, Bochner BH. Bladder cancer imaging: an update. Curr Opin Urol. 2011;21:393–7.
Paik ML, Scolieri MJ, Brown SL, Spirnak JP, Resnick MI. Limitations of computerized tomography in staging invasive bladder cancer before radical cystectomy. J Urol. 2000;163:1693–6.
Kundra V, Silverman PM. Imaging in oncology from the University of Texas M. D. Anderson Cancer Center. Imaging in the diagnosis, staging, and follow-up of cancer of the urinary bladder. AJR Am J Roentgenol. 2003;180:1045–54.
Kelloff GJ, Hoffman JM, Johnson B, et al. Progress and promise of FDG-PET imaging for cancer patient management and oncologic drug development. Clin Cancer Res. 2005;11:2785–808.
von Schulthess GK, Steinert HC, Hany TF. Integrated PET/CT: current applications and future directions. Radiology. 2006;238:405–22.
Kibel AS, Dehdashti F, Katz MD, et al. Prospective study of [18F]fluorodeoxyglucose positron emission tomography/computed tomography for staging of muscle-invasive bladder carcinoma. J Clin Oncol. 2009;27:4314–20.
Swinnen G, Maes A, Pottel H, Vanneste A, Billiet I, Lesage K, Werbrouck P. FDG-PET/CT for the preoperative lymph node staging of invasive bladder cancer. Eur Urol. 2010;57:641–7.
Apolo AB, Riches J, Schoder H, et al. Clinical value of fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography in bladder cancer. J Clin Oncol. 2010;28:3973–8.
Lodde M, Lacombe L, Friede J, Morin F, Saourine A, Fradet Y. Evaluation of fluorodeoxyglucose positron-emission tomography with computed tomography for staging of urothelial carcinoma. BJU Int. 2010;106:658–63.
Drieskens O, Oyen R, Van Poppel H, Vankan Y, Flamen P, Mortelmans L. FDG-PET for preoperative staging of bladder cancer. Eur J Nucl Med Mol Imaging. 2005;32:1412–7.
Bouchelouche K, Oehr P. Positron emission tomography and positron emission tomography/computerized tomography of urological malignancies: an update review. J Urol. 2008; 179:34–45.
Goodfellow H, Viney Z, Hughes P, et al. Role of fluorodeoxyglucose positron emission tomography (FDG PET)-computed tomography (CT) in the staging of bladder cancer. BJU Int. 2014;114:389–9.
Hitier-Berthault M, Ansquer C, Branchereau J, Renaudin K, Bodere F, Bouchot O, Rigaud J. 18 F-fluorodeoxyglucose positron emission tomography-computed tomography for preoperative lymph node staging in patients undergoing radical cystectomy for bladder cancer: a prospective study. Int J Urol. 2013;20:788–96.
Jensen TK, Holt P, Gerke O, Riehmann M, Svolgaard B, Marcussen N, Bouchelouche K. Preoperative lymph-node staging of invasive urothelial bladder cancer with 18F-fluorodeoxyglucose positron emission tomography/computed axial tomography and magnetic resonance imaging: correlation with histopathology. Scand J Urol Nephrol. 2011;45:122–8.
Kim B, Choi HJ, Kim MH, Cho KS. Recurrence patterns of bladder transitional cell carcinoma after radical cystectomy. Acta Radiol. 2012;53:943–9.
Birkhauser FD, Studer UE, Froehlich JM, et al. Combined ultrasmall superparamagnetic particles of iron oxide-enhanced and diffusion-weighted magnetic resonance imaging facilitates detection of metastases in normal-sized pelvic lymph nodes of patients with bladder and prostate cancer. Eur Urol. 2013;64:953–60.
Tilki D, Brausi M, Colombo R, et al. Lymphadenectomy for bladder cancer at the time of radical cystectomy. Eur Urol. 2013;64:266–76.
Powles T, Murray I, Brock C, Oliver T, Avril N. Molecular positron emission tomography and PET/CT imaging in urological malignancies. Eur Urol. 2007;51:1511–21.
Maurer T, Souvatzoglou M, Kubler H, et al. Diagnostic efficacy of [11C] choline positron emission tomography/computed tomography compared with conventional computed tomography in lymph node staging of patients with bladder cancer prior to radical cystectomy. Eur Urol. 2012;61:1031–8.
Beggs AD, Hain SF, Curran KM, O’Doherty MJ. FDG-PET as a “metabolic biopsy” tool in non-lung lesions with indeterminate biopsy. Eur J Nucl Med Mol Imaging. 2002;29:542–6.
Acknowledgment
We thank Drs. Hyuk Jae Choi, Jeong Kon Kim, Kyung Sik Cho, and Jong Jin Lee for their dedicated review of the conventional CT and FDG-PET CT analysis and critical revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jeong, I.G., Hong, S., You, D. et al. FDG PET–CT for Lymph Node Staging of Bladder Cancer: A Prospective Study of Patients with Extended Pelvic Lymphadenectomy. Ann Surg Oncol 22, 3150–3156 (2015). https://doi.org/10.1245/s10434-015-4369-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4369-7