Abstract
Background
A small differentiated gastric cancer with minute submucosal invasion after endoscopic resection is regarded as the curative resection criterion of an expanded indication. However, recent studies have shown a high incidence of lymph node metastasis in those meeting the expanded criteria. The aim of this study was to evaluate the validity of the 500 μm criterion and to determine an optimal cutoff value for the expanded indication.
Methods
We reviewed the clinicopathological data of 1,322 patients who underwent curative resection for submucosal gastric cancer between 2001 and 2013. The full thickness of the submucosa and the incidence of lymph node metastasis according to the depth of the submucosal invasion were evaluated. The sensitivity, specificity, and positive and negative predictive values were calculated with receiver operating characteristic (ROC) curve analysis.
Results
The mean full thickness of the submucosa was 2,605 ± 1,760 μm, and the incidence of lymph node metastasis in 103 tumors meeting the expanded indication was 3.9 % (4/103). In the ROC analysis, the area under the curve was 0.664 (95 % confidence interval 0.538–0.791; p = 0.017), and the highest negative predictive value of 98 % was observed when the cutoff value was 300 μm.
Conclusions
This study suggests that a range reduction in the depth of submucosal invasion is required to obtain a high negative predictive value. Further large-scale studies are required to validate the optimal cutoff value proposed in this study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Endoscopic resection is now widely performed as one of the treatment options for early gastric cancer. According to recent Japanese guidelines, endoscopic resection is indicated as a standard treatment for tumors meeting the absolute indication (intramucosal, differentiated type, no ulcer, ≤2 cm).1 As an investigational treatment, endoscopic submucosal dissection (ESD) has also been accepted for tumors meeting the expanded criteria as follows: (1) intramucosal, differentiated type, no ulcer, >2 cm; (2) intramucosal, differentiated type, ulcer present, ≤3 cm; and (3) intramucosal, undifferentiated type, no ulcer, ≤2 cm.
For submucosal cancer, endoscopic resection has not been suitable because of the high possibility of lymph node metastasis, which is approximately 10–20 %.2–4 However, Gotoda et al.3 revealed no incidence (0/145) of lymph node metastasis in minute submucosal cancer, and the following conditions have been included in the curative resection criteria of the expanded indications: SM1 invasion (<500 μm), size ≤3 cm, differentiated type, no lymphovascular invasion (LVI), en bloc resection, and a negative margin.
However, recent studies have shown higher incidences of lymph node metastasis in the expanded indication compared with those reported by Gotoda et al.3,5–7 Moreover, the depth of submucosal invasion can be different according to the measurement method, and this discrepancy has resulted in debate over the suitability of the 500 μm criterion. Because treatment can be entirely different according to the depth of the submucosal invasion, careful consideration is needed in deciding the criteria for the depth of submucosal invasion.
In this study, we aimed to determine whether the 500 μm criterion is appropriate as the curative resection criterion of the expanded indication, and what submucosal invasion depth cutoff value is optimal for endoscopic resection.
Patients and Methods
Study Cohort and Data
Between January 2001 and December 2013, a total of 1,919 patients underwent curative gastrectomy with lymph node dissection for submucosal gastric cancer at the National Cancer Center, Korea. Laparoscopy- or robot-assisted surgery was performed in 809 (61.2 %) patients, and the proportion of subtotal gastrectomy was 78.7 % (1,040/1,322). All patients underwent D1+ or D2 lymph node dissection as defined by Japanese treatment guidelines.1 Of these patients, we excluded 163 who had multiple lesions, 3 with unusual histology, such as hepatoid and sarcomatoid carcinoma, 1 who had previously undergone a subtotal gastrectomy for gastric cancer, and 1 who had received chemotherapy for gastric lymphoma. Moreover, 429 patients were excluded because they had no description of the depth of submucosal invasion (μm) in the pathological report. A total of 1,322 patients with submucosal invasion were included in this study
The clinicopathological characteristics were reviewed based on the medical charts and pathological reports. Tumor location was categorized as upper, middle, or lower one-third and overlapping based on the center of the main lesion, and the maximum diameter was recorded as the tumor size. The macroscopic tumor type was reported based on the pathological finding according to Japanese guidelines.8 A combined type, such as Type O-IIc + Iib, was classified as a predominant type (the former one, IIc). Histological type was classified according to the World Health Organization classification and was categorized according to recent Japanese guidelines. Papillary adenocarcinoma, and well and moderately differentiated tubular adenocarcinoma, were included in the differentiated type, while the undifferentiated type included poorly differentiated tubular adenocarcinoma, signet ring cell carcinoma, and mucinous adenocarcinoma.8,9 When a tumor consisted of components of both differentiated and undifferentiated types, a quantitatively predominant type was described.1 LVI was defined as tumor cells that were spread through the lymphatic or venous vessels and were categorized as ‘not identified’ or ‘present’. The 7th American Joint Committee on Cancer (AJCC) TNM classification was used to indicate the depth of invasion and lymph node metastasis.4
This study was performed with the approval of the Institutional Review Boards of the National Cancer Center, Korea (NCC2014-0019).
Evaluation of the Depth of Submucosal Invasion and Lymph Node
As soon as a specimen was extracted, a surgeon opened the specimen according to the greater or lesser curvature depending on tumor location. Lymph node was also classified by a surgeon as nodal station according to the Japanese classification. The specimen was then sent to an experienced pathologist (MCK).8 The lesion was identified, and the mucosal folds around the lesion were unfolded evenly without any forced stretching. After gross examination, the specimen was pinned at the edges without stretching. After formalin fixation, the pathologist evaluated the depth of invasion and lymph node metastasis.
The depth of submucosal invasion was the length (in μm) from the lower border of the muscularis mucosae to the point of the deepest tumor penetration.1 When the continuity of muscularis mucosa was disrupted due to tumor infiltration or ulcer formation, or only a small fragment separately remained in the upper submucosa, the length was measured on the virtual line of the muscularis mucosae, based on the remaining adjacent layer, to the point of the deepest tumor penetration (Fig. 1).
Measurement of submucosal invasion. a Intact muscularis mucosa, from the lower border of the muscularis mucosa. b Absence of muscularis mucosa, from the virtual line extended from the remaining adjacent muscularis mucosae. c Split muscularis mucosa, from the major muscle bundles of which virtual extensions were in continuity with the adjacent muscularis mucosae. d Two methods to measure the submucosal depth: (i) from the lowest fragments of the muscularis mucosa, and (ii) from the imaginary line of the remaining adjacent muscularis mucosa
Statistical Analysis
All continuous values are presented as mean ± standard deviation; categorical variables are presented as portions. Differences in distributions were tested using the χ 2test for categorical variables and the t test for continuous variables.
The predictive performance of the depth of submucosal invasion for lymph node metastasis was evaluated using a receiver operating characteristic (ROC) curve; the area under the curve (AUC), sensitivity, specificity, and positive and negative predictive values were also calculated.
All p values were two-sided, and values of <0.05 were considered statistically significant. All data were analyzed using SAS version 9 (SAS Institute Inc., Cary, NC, USA) or R software (version 2.12.1).
Results
Full Thickness of Submucosa
The full thickness of the submucosa was measured in 559 of 1,322 patients from June 2005 to April 2010. In these patients, the mean full thickness of the submucosa (±standard variation) was 2,605 μm (±1,760) and the median thickness (range) was 2,100 μm (20–13,000).
Clinicopathological Characteristics and Incidence of Lymph Node Metastasis According to the Depth of Submucosal Invasion
The clinicopathological characteristics of 1,322 patients with submucosal invasion are shown in Table 1. The mean number of dissected lymph nodes was 39.1, and a positive lymph node was found in 18.8 % (248/1,322) of patients.
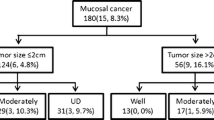
To evaluate the incidence of lymph node metastasis according to the depth of submucosal invasion, tumors meeting the following criteria were selected: (1) submucosal invasion; (2) differentiated histological type; (3) tumor size ≤3 cm; and (4) no LVI. Among a total of 272 patients with tumors meeting the above conditions, 103 had submucosal cancer with a depth of invasion of <500 μm. The incidences of lymph node metastasis were 2.9, 0, 7.7, 5.6, and 0 % in patients with 0–100, 100–200, 200–300, 300–400, and 400–500 μm submucosal cancers, respectively (Table 2). Overall, the incidence of lymph node metastasis was 3.9 % (4/103) for tumors meeting the curative resection criteria of the expanded indication.
Table 2 also shows the incidences of lymph node metastasis for all of the submucosal cancer patients. Approximately 5–35 % of the lymph node metastasis was found at each depth, and the overall incidence of lymph node metastasis in submucosal cancers within 500 μm of the depth of invasion was 9.6 % (35/366).
Lymph Node-Positive Cases Among Those Meeting the Expanded Criteria
Table 3 summarizes the clinicopathological characteristics of patients with lymph node metastasis. The tumors in cases 1–4 met the curative resection criteria of the expanded indication for ESD; however, lymph node metastasis was identified.
Predictive Performance of Depth of Submucosal Invasion for Lymph Node Metastasis
We performed an ROC analysis to evaluate the predictive performance of the depth of submucosal invasion for lymph node metastasis in 272 patients meeting the following conditions: (1) submucosal cancer; (2) differentiated type; (3) tumor size ≤3 cm; and (4) no LVI. The AUC of the depth of submucosal invasion was 0.664 (95 % confidence interval 0.538–0.791; p = 0.017); Table 4 shows the sensitivity, specificity, positive predictive value, and negative predictive value at each cutoff point. The negative predictive values ranged from 95.7 to 98.1 % at each depth of submucosal invasion, and the highest negative predictive value was observed when the cutoff point was 300 μm.
Discussion
Since Gotoda et al.3 reported no lymph node metastasis in minute submucosal cancer, a ‘depth of submucosal invasion of 500 μm’ has become a key criterion for the curability of ESD. However, higher incidences of lymph node metastasis were reported in several Korean studies, and the 500 μm criterion has been debated. The present study also shows 3.9 % of lymph node metastasis in minute submucosal cancer, and evaluated the validity of the 500 μm criterion using ROC curve analysis. As a result, the highest negative predictive value was observed at a cutoff value of 300 μm.
The incidence of lymph node metastasis has been evaluated in several previous studies with reference to the feasibility of ESD for submucosal cancer. In the study by Jee et al.5 the incidence of lymph node metastasis in submucosal cancers meeting the expanded indication was 3.8 % (2/52); a similar result (4.1 %, 2/49) was shown in the study by Kim et al.6 In the study by Kang et al.7 the incidence of lymph node metastasis was found to be 15.0 % (3/20) for patients with the same conditions. These high incidences of lymph node metastasis have given rise to debate of the suitability of the 500 μm criterion; however, no study has yet evaluated the optimal depth of the submucosal invasion cutoff value.
This study evaluated the incidences of lymph node metastasis at each 100 μm of depth of the invasion subgroup, and considerable variation in each subgroup was observed, most likely due to the small number in each subgroup population. Moreover, the accumulated incidences seem to be almost similar between ‘<300’ and ‘<1,500 μm’ without a sharp increase in lymph node metastasis. However, the negative predictive value was highest at the 300 μm cutoff value, which indicates that we can reduce the false negative cases to <2 % with a cutoff value of 300 μm. Therefore, a range reduction in the depth of submucosal invasion criterion may be proposed for the expanded indication if an ESD could be performed on the assumption there was little change in lymph node metastasis.
The higher incidence of lymph node metastasis in recent studies compared with the study by Gotoda et al.3 could be associated with the submucosal invasion measurement method. According to Japanese guidelines, the depth of submucosal invasion is defined as the length from the lower border of the muscularis mucosa to the point of deepest tumor penetration.8 However, when the muscularis mucosa is obscure due to tumor infiltration or ulcer formation, the measurement of submucosal invasion is difficult, and can result in a discrepancy between pathologists. Kim et al.10 compared two methods: one was to measure from the lowest point of the muscularis mucosa to deepest tumor, and the other was to measure from the lowest point of the imaginary line of the remaining adjacent muscularis mucosa to the deepest tumor (Fig. 1d). The significance of correlation between lymph node metastasis and the depth of submucosal invasion was different according to the two measurement methods. Therefore, standardization in measuring submucosal invasion is needed for an objective application of the expanded indication for ESD.
The depth of submucosal invasion can also be influenced by the stretching of resected tissue.11–13 An ESD specimen is generally stretched and pinned on a cork board in the endoscopy unit. According to the study by Park et al.11 evaluating the effects of stretching on different layers and sites of porcine gastric tissue, the gastric wall and submucosal layers showed gradual thinning with stretching, and the submucosal layer was thinner in body tissue than in cardia or antrum tissue. Cho et al.12 also demonstrated a decrease in the depth of the submucosa in fully stretched porcine gastric tissue compared with non-stretched tissue. A lesion with 500 μm of submucosal invasion in an ESD specimen could correspond to a deeper lesion in a surgical specimen, and the incidence of lymph node metastasis may also be higher than the expected incidence. Therefore, the handling method for ESD specimens should be standardized to ensure proper estimation of the submucosal invasion, and it is recommended the ESD specimen be put on a cork board evenly and pinned without any forced stretching.
This study has several limitations. First, the total number of cases is insufficient because this study was performed using a single-center database. Submucosal cancers meeting the curative resection criteria of the expanded indication accounted for a minor portion only, and only 10–30 patients were included in each 100 μm of depth of the submucosal invasion subgroup. Thus, the incidence of lymph node metastasis was considerably different, with even one or two positive cases suggesting that the incidence of lymph node metastasis can differ in other databases. Second, in our ROC curve analysis, the AUC was 0.664, which is a statistically poor performance in predicting lymph node metastasis. However, this result is comparable with a previous study (AUC 0.645), and it seems that the exact prediction of lymph node metastasis using one factor (depth of submucosa invasion) is difficult.10 For this inaccuracy, the previous study suggested a predictive scoring system and developed a new nodal predicting index using four factors—lymphovascular emboli, submucosal invasion width, submucosal invasion depth, and infiltrative growth pattern. These four factors yielded higher predictive performance with an AUC of 0.809.10 Although, insufficient prediction performance was observed compared with the predicting index, this study derived a cutoff value minimizing false negative cases by statistical analysis.
Conclusions
The incidence of lymph node metastasis in submucosal cancers meeting the expanded indication was 3.9 %, and the highest negative predictive value was demonstrated at a cutoff value of 300 μm. Further large-scale studies are required to validate the optimal cutoff value of the depth of submucosal invasion for the expanded indication.
References
Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011;14:113–23.
An JY, Baik YH, Choi MG, Noh JH, Sohn TS, Kim S. Predictive factors for lymph node metastasis in early gastric cancer with submucosal invasion: analysis of a single institutional experience. Ann Surg. 2007;246:749–53.
Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–25.
Warneke VS, Behrens HM, Hartmann JT, et al. Cohort study based on the seventh edition of the TNM classification for gastric cancer: proposal of a new staging system. J Clin Oncol. 2011;29:2364–71.
Jee YS, Hwang SH, Rao J, et al. Safety of extended endoscopic mucosal resection and endoscopic submucosal dissection following the Japanese Gastric Cancer Association treatment guidelines. Br J Surg. 2009;96:1157–61.
Kim JH, Lee YC, Kim H, et al. Additive lymph node dissection may be necessary in minute submucosal cancer of the stomach after endoscopic resection. Ann Surg Oncol. 2012;19:779–85.
Kang HJ, Kim DH, Jeon TY, et al. Lymph node metastasis from intestinal-type early gastric cancer: experience in a single institution and reassessment of the extended criteria for endoscopic submucosal dissection. Gastrointest Endosc. 2010;72:508–15.
Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–12.
Hamilton SR LL. World Health Organization classification of tumours. Lyon: IARC; 2000.
Kim JY, Kim WG, Jeon TY, et al. Lymph node metastasis in early gastric cancer: evaluation of a novel method for measuring submucosal invasion and development of a nodal predicting index. Hum Pathol. 2013;44:2829–36.
Park S, Chun HJ, Kwon YD, et al. Stretching causes extensive changes of gastric submucosa: is it acceptable to define 500 microm as the safe margin? Gut Liver. 2008;2:199–204.
Cho JY, Kim YS, Jung IS, et al. Controversy concerning the cutoff value for depth of submucosal invasion after endoscopic mucosal resection of early gastric cancer. Endoscopy. 2006;38:429–30; author reply 430.
Min YW LJ. Endoscopic resection for early gastric cancer beyond absolute indication with emphasis on controversial issues. J Gastric Cancer. 2014;14:7–14.
Acknowledgment
This work was supported by a Grant from the National Cancer Center (No. NCC-1210552-3).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Keun Won Ryu and Myeong-Cherl Kook have contributed equally to this study and both serve as co-corresponding authors.
Rights and permissions
About this article
Cite this article
Eom, B.W., Yu, J.S., Ryu, K.W. et al. Optimal Submucosal Invasion of Early Gastric Cancer for Endoscopic Resection. Ann Surg Oncol 22, 1806–1812 (2015). https://doi.org/10.1245/s10434-014-4308-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4308-z