Abstract
Background
Locally recurrent rectal cancer remains a dreaded event because curative resection is unlikely to be performed in a large number of cases. Carbon ion radiotherapy offers physical and biologic advantages. A high precise local dose deposition and sparing of normal tissue is possible. This work summarizes our experience on feasibility and early toxicity of carbon ion radiotherapy in previously irradiated and operated patients.
Methods
Between 2010 and 2013, a total of 19 patients with a median age of 62 years (range 14–76 years) received carbon ion irradiation to treat locally recurrent rectal cancer at the Heidelberg Ion Beam Therapy Center (HIT). All patients had a history of surgery and pelvic radiotherapy of at least 50.4 Gy. Median dose was 36 Gy [relative biologic efficacy (RBE)] [range 36–51 Gy(RBE)], and median planning target volume was 456 ml (range 75–1,597 ml). Some patients were treated in the recruiting phase I/II of the PANDORA study (NCT01528683).
Results
Median follow-up was 7.8 months. Four patients were diagnosed with local relapse after carbon ion radiotherapy, and three patients developed distant metastases. Estimated mean local progression-free survival was 20.6 months by the Kaplan–Meier estimator. Two patients had preexisting rectovaginal fistula, and another patient had a preexisting presacral localized abscess formation in which the local relapse took place. No grade III or higher toxicities were observed.
Conclusions
Our first experiences in a pretreated patient group with a dismal prognosis are encouraging, and therapy-related side effects are mild. Longer follow-up is required to determine possible late effects and long-term disease control.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Rectal cancer is a widespread malignancy with one of the highest incidence rates in Western countries and is newly diagnosed in approximately 25,000 patients in Germany per year. Treatment of rectal cancer depends on initial staging. All curative treatment approaches include a complete tumor resection consisting of a transanal microscopic surgery for small T1 lesions and an anterior resection for most T2–4 tumors.1 Randomized clinical trials have shown that preoperative chemoradiation significantly reduces the risk of local failure and recurrence after 10 years, from 10.1 to 7.1 % in clinical stage II and III disease.2 A meta-analysis demonstrated that preoperative chemoradiotherapy (CRT) is more beneficial than single-modality radiotherapy (RT) in achieving a better pathologic response and a higher local control rate.3 Usually preoperative CRT is provided over 5–6 weeks with simultaneous 5-fluorouracil or an even shorter regimen of 5 × 5 Gy directly before surgery.4
Even when the rate of local recurrences is low after multimodal treatment including CRT, surgery, and adjuvant chemotherapy, 81 % of all recurrences develop in field or at the margins.5 A total of 78 % of the in-field relapses occur in the low pelvic and presacral region.5 Whenever surgical resection can be reasonably performed, it remains the mainstay of therapy, but a high percentage of locally recurrent rectal carcinoma (LRRC) show osseous or vessel infiltration in the pelvis, making surgery difficult. However, in some cases, resection is not possible or cannot be performed safely for medical reasons such as comorbidities. For these patients, RT represents an alternative local intensified treatment option in contrast to palliative systemic therapies. Different groups have reported their experiences with RT in case of relapse in patients with and without a history of RT.6,7 Using modern high-precision photon techniques such as image-guided or intensity-modulated RT, high doses can be delivered to the tumor area while sparing normal tissue, including organs at risk (e.g., large and small intestine, bladder, rectum). Fort treatment planning purposes, three-dimensional computed tomography (CT) and magnetic resonance imaging (MRI) may be used, and thus repeat irradiation can be provided for recurrent rectal cancer. Usually doses limited to 36–45 Gy are applied with small safety margins due to previous radiation exposure during initial therapy.
In contrast, particle beam therapy using protons (1H) or carbon ions (12C) offers advantageous physical and biologic properties, even compared to high-precision photon RT. Physical characteristics include a low dose deposition within the entry channel of every single beam, followed by a steep dose deposition in the spread-out Bragg peak, followed by a sharp dose falloff. Furthermore, 12C offers significant biologic advantages through an increased induction of clustered DNA double-strand breaks within the irradiated cells, which are difficult to repair. This results in an enhanced relative biologic efficacy (RBE) compared to reference irradiation with photons.
This new treatment modality seemed worth being tested in rectal cancer patients with isolated recurrences in the pelvic region in a controlled clinical trial. Whereas 12C showed good results in a wide variety of malignancies and in reirradiation settings, clinical data on 12C-reirradiation in rectal cancer patients are scarce.8–10 Additionally, there is a complete lack of 12C RT for this indication using the active raster-scanning technique, which permits higher-precision particle beams. Active beam delivery using the raster scanning method is highly focused by using a pencil beam that is moved by two magnetic dipoles, leading to a point-by-point scan of the target structure. At our institution, the beam is generated by a synchrotron, which allows the energy to be switched from one pulse to another to shape the particle range in the irradiated tissue. The target volume can be scanned in all three dimensions, and even irregular shapes can be scanned without requiring further hardware such as collimators or compensators. The main advantage of this method compared to passive beam shaping, as practiced in most particle therapy facilities, is the better precision of the delivered particle beams, especially at the proximal, distal, and lateral target borders. Moreover, fewer nuclear fragments are produced as a result of the avoidance of the hardware material in the beam line to shape the passive beam, which leads to a higher dose to the entrance channel and thus to adverse normal tissue contamination.11
Smaller patient groups are reported from Japanese institutions that examined the therapeutic efficacy of passive scattered 12C beams in primarily diagnosed rectal cancer patients.12–14 Overall local control rates were encouraging, and toxicity was comparable and mild. However, reirradiation protocols always carry the risk of increased toxicity rates. Therefore, we here present the first data, including feasibility, outcomes, and toxicity, in patients after 12C reirradiation in case of LRRC in the pelvic region.
Patients and Methods
Patient Selection
Patients were mainly selected according to the PANDORA clinical trial protocol (NCT01528683); inclusion criteria were LRRC represented by an inoperable lesion (macroscopic tumor up to 1,000 ml in volume), prior photon RT of 20 to 60 Gy, and absence of any distant metastasis.15 However, we also included in our analysis patients who did not fulfill the PANDORA study protocol inclusion criteria. All patients were seen and evaluated in an interdisciplinary setting including specialists from gastroenterology, medical oncology, visceral surgery, radiology, and radiation oncology.
Patient Characteristics
From 2010 to 2013, the disease of a total of 19 patients with LRRC was reirradiated with 12C at the Heidelberg Ion Therapy Center (HIT) (Table 1). Median age was 62 years (range 14–76 years), and there were nine female and ten male patients. All patients had been previously irradiated with at least 50.4 Gy (median 50.4 Gy, range 50.4–60.4 Gy) and had undergone at least one resection due to rectal carcinoma. One patient had a history of two RT series (50.4 Gy in the primary setting using conventional pelvic RT and CyberKnife-based radiosurgery with 19 Gy to treat an in-field relapse) (Table 2). A further patient previously underwent intraoperative radiotherapy with 15 Gy additionally delivered to the conventional pelvic RT. The applied 12C doses at our institution varied from 36 to 51 Gy(RBE) in single fractions of 3 Gy(RBE). Median duration between initial RT and 12C re-RT was 47.4 months (range 17–110 months). The median planning target volume (PTV) was 456 ml (range 75–1,597 ml).
Treatment Planning
Patients were immobilized in the supine position with an indexed positioning of the lower extremities using a ProSTEP (Elekta, Sweden) immobilization device to account for a precise repositioning of the pelvic area. For treatment planning, a contrast-enhanced CT was performed, and on an individual, case-by-case basis, further imaging was recommended, including MRI and 18F-fludeoxyglucose-positron emission tomography imaging, for optimal target definition.
Typical organs at risk were contoured including the small intestine, bladder, spinal cord, rectum, and vagina. Dose constraints of normal tissue were respected according to Emami et al.16 Target definition included the gross tumor volume (GTV) based on the area of contrast enhancement on T1-weighted MRI. A clinical target volume was defined as the GTV enlarged by an anatomically adopted safety margin of 5–10 mm depending on tumor location. Finally, the PTV was generated on individual factors, such as patient positioning and beam angles chosen, and was between 3 and 10 mm. Carbon ion RT planning was performed using the treatment planning software PT-Planning (Siemens Healthcare, Erlangen, Germany), including biologic plan optimization based on the local effect model developed by GSI (Gesellschaft für Schwerionenforschung, Darmstadt, Germany); it is designed for RBE calculation in different tissue types and for selected endpoints.17 Briefly, the dependency of RBE on the physical and biologic properties are stronger than in conventional RT. The local effect model therefore incorporates photon- and carbon ion-based cell-survival data as well as the knowledge on the different topographical or local pattern of dose deposition between photons and charged particles along the beam (e.g., DNA double strand breaks). Energy deposition patterns on a molecular level (DNA level) are considered and integrated in the local effect model. The resulting RBE values depend on dose and cell type.
In the current clinical setting, the Syngo RT treatment planning system was used, which works with an αβ-value of 2 Gy, which fits well to serious late adverse events (stricture; rectal or intestinal bleeding or ulceration). Publications on RBE values of rectal cancer are scarce, so we referred to our in-house in vitro data on HCT 116 rectal cancer cell lines. Experimental data revealed an RBE value of approximately 2.5 (unpublished data).18 In future versions of the treatment planning system, biologic planning will be more adaptive, thus integrating a higher amount of different tumor and normal tissue specific parameters. Daily patient positioning was controlled by comparison of digitally reconstructed radiographs with on-board kilovoltage imaging as described previously.10,19
Radiotherapy
Single fractions of 3 Gy(RBE) were applied in all patients. Patients treated in the phase I PANDORA study received doses according to the dose escalation protocol with fraction numbers from 12 to 18, leading to theoretical overall doses of 36–54 Gy(RBE).15 Doses were prescribed to the maximum of the calculated dose distribution for the PTV. Treatment planning aims in the coverage of the PTV by the 90 % isodose line. Dose specification is based on biologic equivalent dose because of the high relative biologic effectiveness (RBE) of carbon ions, which differs throughout the target volume due to its dependence on various factors. RBE will be calculated at each voxel throughout the target volumes and biologic optimization will be performed. Single doses of 3 Gy(RBE) carbon ions are established in our institution because the first patients were treated by this modality at the GSI in Darmstadt (Germany). The proposed regimen for the treatment of LRRC was set to 12 × 3 Gy(RBE) for the first step in the dose escalation PANDORA trial. Referring to a large experience in treating sacral chordoma with similar and also higher doses in nearly the same anatomical region, we consider this dose schedule to be safe and putatively effective.8,10,20
A total of 8 patients received RT via a single lateral 12C-beam and 11 patients with two lateral opposing beams on a horizontal beam treatment room (Fig. 1).
Follow-up
Patients are currently undergoing follow-up visits with physical examination, laboratory tests, and CT and MRI. Progression-free survival was determined as time period between the first day of RT and appearance of any local recurrence or progression. Observed toxicity was categorized according to the Common Toxicity Criteria of Adverse Events, version 4.03.
Results
Survival and Local Control
Median follow-up of all patients was 8 months. Three patients (16 %) died during the observation period. Four patients (21 %) experienced local progression after RT, and three patients (16 %) were diagnosed with distant metastases. During follow-up, three patients died after 3.3, 3.4, and 32.3 months. Calculated median overall survival for patients that were still alive was 9.1 months. Because of the short follow-up period, most patients were still alive and under observation at the time of this writing, so the median survival cannot yet be computed.
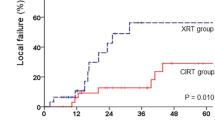
Local progression was seen in four patients after 2.1, 4.6, 16.5, and 20.6 months; systemic progression with distant metastasis was observed in three patients in whom no local progression was observed (Fig. 2). Estimated local progression according to the Kaplan–Meier estimator was 20.6 months, but most of the patients have not yet experienced disease progression. One patient developed a distant lymphatic relapse of rectal cancer. PTV (less than 600 ml or greater than 600 ml, 24.8 vs. 15.2 months, respectively) and applied dose (36 Gy(RBE) vs. ≥36 Gy(RBE), 20.2 vs. 15.2 months, respectively) were not predictive of local failure.
Toxicity
Two patients had preexisting rectovaginal fistulas without signs of acute inflammation at the initiation of RT. One did not develop any complication during and after RT. The other showed an increase of the fistula and slight signs of mild inflammation, but neither surgery nor further drainage were necessary.
One patient had a preexisting (pre-)sacral abscess formation with tumor manifestations that were treated with antibiotics. After RT, the abscess formation showed a premature enlargement and a further progression of the tumor content. A further patient had a lymphatic fistula as a consequence of surgery with no signs of inflammation during RT and after follow-up.
In general, gastrointestinal toxicities occurred in two patients with grade II side effects and five patients with grade I side effects (Table 3). Skin erythema was seen in one patient (grade II). Hematologic side effects were also observed and were classified as grade I in two patients (erythrocyte count). There were no cases of nausea or pain aggravation during RT and at first follow-up.
Discussion
Reirradiation with 12C for LRRC seems to provide moderate local control with acceptable toxicity, considering the difficult clinical situation with previous radiotherapy and surgeries. Further dose escalation and longer follow-up may improve the preliminary data; however, the need for careful patient selection limits application of the protocol in a larger patient population. The introduction of preoperative chemoradiation and radiation protocols led to a significant reduction of local recurrence rates in rectal cancer patients.2,4 Nevertheless, local relapse is still a serious event in preirradiated patients, depending on localization and infiltration of anatomic structures. In many patients, surgical repeat resection cannot be performed safely; therefore, multimodal treatment approaches, including modern RT techniques and systemic agents, are necessary. The presented patient group was treated with carbon ion beams, with therapy performed as reirradiation in case of LRRC. Progression-free survival was encouraging, and toxicity rates were low.
Reports on reirradiation in LRRC patients are rare and heterogeneous considering RT dose and concurrent systemic treatment. In the recent study of Das et al., a hyperfractionated accelerated RT protocol was examined in previously irradiated patients with LRRC.21 The median dose of pretreatment RT was 47 Gy (range 25–70 Gy). Patients irradiated more than 1 year before received a dose of 39 Gy in two 1.5 Gy fractions per day, and those patients who had pelvic RT less than 1 year before were treated with 30 Gy using the same fractionation schedule. Freedom from local progression was achieved in 33 % after 3 years, with a borderline significant difference between the patient group that underwent additional surgical resection after repeated RT and those that did not (47 and 21 %, respectively). Furthermore, a secondary surgical resection led to a significant survival advantage, leading to a 3-year overall survival of 66 % in the resection group compared to 27 % in RT-only patients. Overall acute toxicity was relatively mild, with only two patients (4 %) experiencing grade III events, with nausea and vomiting. Late toxicity rates were higher, with 13 patients (26 %) developing grade III and IV toxicity events, mainly due to small bowel and bladder side effects.
There also exist re-RT protocols including concurrent chemotherapy application. Valentini et al. performed an Italian multicenter phase II study examining a preoperative hyperfractionated chemoradiation for LRRC patients.22 Fifty-nine patients were treated with twice-daily 1.2 Gy up to a total dose of 30 Gy to a target volume encompassing the GTV with a 4 cm margin. Subsequently a boost was applied to the GTV plus a 2 cm margin with further 10.8 Gy in the same fractionation scheme. Chemotherapy with 5-fluorouracil was applied simultaneously with 225 mg/m2 per day, 7 days a week. Tolerance of study treatment was good, and no patient developed grade IV toxicity. Acute grade III gastrointestinal side effects were observed in only 5.1 % of all patients. Late toxicity was seen in one patient with small bowel obstruction requiring surgery. Actuarial survival rates were 87.5, 58.9, and 39.3 % after 1, 3, and 5 years. Median local control was 20 months, and median disease-free survival was 15.5 months. Forty-four percent of all patients experienced at least a partial response of their tumor to chemoradiation. A total of 66.1 % of all patients underwent surgery, and a majority had a complete tumor resection without evidence of residual disease.
Sun et al. recently published a comparable treatment regime including re-RT using hyperfractionation of 2 × 1.2 Gy per day for 3 weeks up to a dose of 36 Gy with concurrent capecitabine in 72 patients.23 Afterward resectability was evaluated, and a total of 18 patients underwent surgery. Patients with disease not suitable for resection continued combined-modality RT up to 51.6–56.4 Gy. A total of 59.7 % showed at least a partial response to the treatment. Acute toxicities included grade III to IV diarrhea and hematologic side effects in 9.7 and 8.3 %, respectively. Higher late toxicity consisted of small bowel obstruction with an incidence rate of 1.4 %.
The accordance of our data on 12C re-RT toxicity levels of conventional pelvic re-RT plus concurrent chemotherapy is almost comparable to that of the above-mentioned studies. However, in contrast to our results on acute toxicities, a small percentage of patients experienced grade III toxicities due to re-RT and systemic agents. Obvious advantages of our strategy on toxicity prevention is the superiority in precision of particle beams compared to photons (especially to non-intensity modulated radiotherapy techniques as applied in the mentioned studies) and the omission of any systemic agent during and shortly after RT. Therefore, no extra toxicity will occur due to an additional use of systemic treatments.
Nevertheless, a total of four patients experienced a further local relapse after 12C-RT, two of them premature, during the first 6 months after RT start. Carbon-ion RT still remains an experimental radiation modality, and therefore it is highly important to continue patient treatment in controlled clinical studies. Implemented biologic optimization algorithms at HIT have to be evaluated continuously and constantly correlated with clinical findings to ensure patient safety and therapeutical benefit.24–26 Particle therapy, including 12C and 1H, seems to be promising in multimodal oncologic concepts. There are two main advantages of 12C beams over proton beams. At first, 12C undoubtedly exerts a higher RBE, leading to a higher amount of clonogenic cell death, even in almost radioresistant tumors (e.g., adenoid cell carcinoma, chordoma, chondrosarcoma, hepatocellular carcinoma).19,27–29 RBE values vary from at least 2 to more than 5, implicating a high tumoricidal potential. On the other hand, 1H beams account for only a mean RBE of approximately 1.1.11 In addition, as a result of the physical properties of 12C, the dose distribution is more conformal than that of 1H. The ratio of dose in the spread-out Bragg peak compared to the entrance channel is larger for carbon ions. Furthermore, 12C atoms have a larger mass and are therefore less prone to nuclear interactions, which allows a higher dose conformality and a higher sharpness in the lateral dose gradient (penumbra).11 Finally, these arguments represent theoretical biologic and dosimetric benefits of 12C over 1H. Nevertheless, these advantages require more costly facilities, and biologic dose computation still remains a matter of debate. At our institution, we set up several clinical trials (including the PANDORA trial) to evaluate which is the better of the two particle modalities in terms of benefit to our patients.
Results of this treatment concept seem promising, and overall toxicity was low. However, longer follow-up is needed before we can draw definitive conclusions on therapeutic effect. Furthermore, longer follow-up is required to determine possible late effects and long-term control of disease of patients treated in the phase I/II clinical trial protocol PANDORA.
References
National Comprehensive Cancer Network. Rectal cancer, version 3.2014. Available at: http://nccn.org.
Sauer R, Liersch T, Merkel S, et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol. 2012;30:1926–33.
De Caluwe L, Van Nieuwenhove Y, Ceelen WP. Preoperative chemoradiation versus radiation alone for stage II and III resectable rectal cancer. Cochrane Database Syst Rev. 2013;2:CD006041.
Ngan SY, Burmeister B, Fisher RJ, et al. Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group trial 01.04. J Clin Oncol. 2012;30:3827–33.
Yu TK, Bhosale PR, Crane CH, et al. Patterns of locoregional recurrence after surgery and radiotherapy or chemoradiation for rectal cancer. Int J Radiat Oncol Biol Phys. 2008;71:1175–80.
Calvo FA, Sole CV, Alvarez de Sierra P, et al. Prognostic impact of external beam radiation therapy in patients treated with and without extended surgery and intraoperative electrons for locally recurrent rectal cancer: 16-year experience in a single institution. Int J Radiat Oncol Biol Phys. 2013;86:892–900.
Alberda WJ, Verhoef C, Nuyttens JJ, et al. Outcome in patients with resectable locally recurrent rectal cancer after total mesorectal excision with and without previous neoadjuvant radiotherapy for the primary rectal tumor. Ann Surg Oncol. 2014;21(2):520–6.
Combs SE, Kalbe A, Nikoghosyan A, et al. Carbon ion radiotherapy performed as re-irradiation using active beam delivery in patients with tumors of the brain, skull base and sacral region. Radiother Oncol. 2011;98:63–7.
Rieken S, Habermehl D, Haberer T, Jaekel O, Debus J, Combs SE. Proton and carbon ion radiotherapy for primary brain tumors delivered with active raster scanning at the Heidelberg Ion Therapy Center (HIT): early treatment results and study concepts. Radiat Oncol. 2012;7:41.
Combs SE, Ellerbrock M, Haberer T, et al. Heidelberg Ion Therapy Center (HIT): initial clinical experience in the first 80 patients. Acta Oncol. 2010;49:1132–40.
Schulz-Ertner D, Jakel O, Schlegel W. Radiation therapy with charged particles. Semin Radiat Oncol. 2006;16:249–59.
Tsujii H, Mizoe JE, Kamada T, et al. Overview of clinical experiences on carbon ion radiotherapy at NIRS. Radiother Oncol. 2004;73(Suppl 2):S41–9.
Yamada S, Shinoto M, Shigeo Y, et al. [Current status and perspective of heavy ion beam therapy for patients with pelvic recurrence after primarily resected rectal cancer]. Gan To Kagaku Ryoho. 2009;36:1263–6.
Koizumi M, Saga T, Yoshikawa K, et al. 11C-methionine-PET for evaluation of carbon ion radiotherapy in patients with pelvic recurrence of rectal cancer. Mol Imaging Biol. 2008;10:374–80.
Combs SE, Kieser M, Habermehl D, et al. Phase I/II trial evaluating carbon ion radiotherapy for the treatment of recurrent rectal cancer: the PANDORA-01 trial. BMC Cancer. 2012;12:137.
Emami B, Lyman J, Brown A, et al. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys. 1991;21:109–22.
Scholz M, Kellerer AM, Kraft-Weyrather W, Kraft G. Computation of cell survival in heavy ion beams for therapy. The model and its approximation. Radiat Environ Biophys. 1997;36:59–66.
Adeberg S, Baris D, Habermehl D, et al. Evaluation of radiochemotherapy with carbon ions and the influence of p53 mutational status in the colorectal carcinoma cell line HCT 116. In: Strahlentherapie und Onkologie. Munich, Germany: Urban & Vogel; 2012. pp. 136–7.
Habermehl D, Debus J, Ganten T, et al. Hypofractionated carbon ion therapy delivered with scanned ion beams for patients with hepatocellular carcinoma—feasibility and clinical response. Radiat Oncol. 2013;8:59.
Schulz-Ertner D, Nikoghosyan A, Thilmann C, et al. Results of carbon ion radiotherapy in 152 patients. Int J Radiat Oncol Biol Phys. 2004;58:631–40.
Das P, Delclos ME, Skibber JM, et al. Hyperfractionated accelerated radiotherapy for rectal cancer in patients with prior pelvic irradiation. Int J Radiat Oncol Biol Phys. 2010;77:60–5.
Valentini V, Morganti AG, Gambacorta MA, et al. Preoperative hyperfractionated chemoradiation for locally recurrent rectal cancer in patients previously irradiated to the pelvis: a multicentric phase II study. Int J Radiat Oncol Biol Phys. 2006;64:1129–39.
Sun DS, Zhang JD, Li L, Dai Y, Yu JM, Shao ZY. Accelerated hyperfractionation field-involved re-irradiation combined with concurrent capecitabine chemotherapy for locally recurrent and irresectable rectal cancer. Br J Radiol. 2012;85:259–64.
Gillmann C, Jakel O, Schlampp I, Karger CP. Temporal lobe reactions after carbon ion radiation therapy: comparison of relative biological effectiveness-weighted tolerance doses predicted by local effect models I and IV. Int J Radiat Oncol Biol Phys. 2014;88:1136–41.
Friedrich T, Grun R, Scholz U, Elsasser T, Durante M, Scholz M. Sensitivity analysis of the relative biological effectiveness predicted by the local effect model. Phys Med Biol. 2013;58:6827–49.
Grun R, Friedrich T, Elsasser T, et al. Impact of enhancements in the local effect model (LEM) on the predicted RBE-weighted target dose distribution in carbon ion therapy. Phys Med Biol. 2012;57:7261–74.
Jensen AD, Nikoghosyan AV, Ecker S, et al. Raster-scanned carbon ion therapy for malignant salivary gland tumors: acute toxicity and initial treatment response. Radiat Oncol. 2011;6:149.
Uhl M, Mattke M, Welzel T, et al. High control rate in patients with chondrosarcoma of the skull base after carbon ion therapy: first report of long-term results. Cancer. 2014;120:1579–85.
Uhl M, Mattke M, Welzel T, et al. Highly effective treatment of skull base chordoma with carbon ion irradiation using a raster scan technique in 155 patients: first long-term results. Cancer. 2014;120(21):3410–7.
Disclosure
Daniel Habermehl, Martin Wagner, Malte Ellerbrock, Markus W. Büchler, Oliver Jäkel, Jürgen Debus and Stephanie E. Combs declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Habermehl, D., Wagner, M., Ellerbrock, M. et al. Reirradiation Using Carbon Ions in Patients with Locally Recurrent Rectal Cancer at HIT: First Results. Ann Surg Oncol 22, 2068–2074 (2015). https://doi.org/10.1245/s10434-014-4219-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4219-z