Abstract
Background
The possibility of lymph node metastasis is critical to the assessment of the indication for endoscopic submucosal dissection. The differentiation of tumors is an important predicting factor for lymph node metastasis. Even though gastric cancers frequently show intratumoral heterogeneity, most studies have not considered the effects of the minor histologic components. The purpose of this study was to investigate the relationship between the presence of undifferentiated type histology (UD-min) within differentiated type tumors and lymph node metastases in early gastric cancer confined to the mucosal layer.
Methods
A retrospective study of 847 patients who underwent surgery for differentiated early gastric cancer, confined to mucosa, was conducted. We analyzed the proportion of the undifferentiated type components of the tumor and their relationship with lymph node metastasis.
Results
The overall rate of lymph node metastasis was 1.7 % (14/847 patients) and 215 differentiated tumors (25.4 %) have UD-min. UD-min was associated with female sex, younger age, larger tumor size, and the presence of ulcer. Lymph node metastasis rate with or without UD-min was 5.1 % (11/215) versus 0.5 % (3/632), respectively (p < 0.001). UD-min was found to be associated with lymph node metastasis in the multivariate analyses (odds ratio [OR] = 4.39, CI 1.08–17.89). When three risk factors (tumor size >2 cm, ulcer, and UD-min) were present concurrently, the rate of lymph node metastasis was high (10 %).
Conclusions
The presence of an UD-min component should be considered when assessing curative resection status of endoscopic submucosal dissection for differentiated type mucosal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastric cancer is the second most common form of cancer in Korea. The overall age-standardized incidence rates of gastric cancer in Korea were reported to be 62.3 per 100,000 males and 24.9 per 100,000 females in 2010.1 Recent progress in diagnostic techniques and an increasing demand for a better quality of life have increased the early diagnosis of gastric cancer in Korea and Japan.2,3 Surveillance conducted by the Korean Gastric Cancer Association showed that the proportion of early gastric cancers (EGC), among gastric cancers overall, detected in Koreans exceeded 57.6 % in 2009.4
Treatment options for EGC include endoscopic mucosal dissection (ESD), wedge resection, laparoscopy, or robot-assisted gastrectomy (LAG) and open gastrectomy.5,6 The possibility of lymph node metastasis is critical to the assessment of the type of resection to perform in patients with early gastric cancer; for example, the absence of lymph node metastasis is a prerequisite for ESD.5 Given that the accuracies of preoperative computed tomography (CT) and endoscopic ultrasonography (EUS) for the detection of lymph node metastases range from 50 to 70 %, clinical/pathological factors, including the presence of ulcers, tumor size, depth of tumor invasion, and tumor differentiation, are important features to consider in determining the risk of lymph node metastasis.7,8
Undifferentiated type histology has been reported to be a risk factor for lymph node metastasis in early gastric cancer.9 Unlike the presence of an ulcer or the depth of tumor invasion, the classification of tumors by their differentiation status is complex and can be difficult to determine. Differentiation of a tumor is determined by the histological type of the major portion of the tumor (more than 50 %) regardless of the minor histological type.10,11 Even though gastric cancers frequently show intratumoral heterogeneity, most studies have not considered the effects of the minor components.12–14
Thus, the purpose of the present study was to assess the meaning of minor undifferentiated type histology (UD-min) for lymph node metastasis in patients with differentiated type mucosal early gastric cancer.
Patients and Methods
Study Population
We conducted a retrospective study from January 2001 to April 2013; 847 patients who underwent surgery for differentiated early gastric cancer confined to mucosa at the National Cancer Center in Korea were included in the study. Recurrent cancers or cancers from remnant stomach were excluded in this study. The cases of which the number of dissected lymph nodes was less than 16 were excluded. When multiple synchronous cancers were present, the cancer having the deepest invasion depth and the largest size was selected for analysis. The preoperative evaluations included esophagogastroduodenoscopy with biopsy, abdominal CT, chest radiography, standard blood testing, and EUS if needed. Well-differentiated mucosal tumors less than 2 cm in size and without ulceration, which were curatively resected by endoscopic resection, were excluded in accordance with the treatment guidelines of our institution and the Japanese guidelines for gastric cancer treatment.15 This study was performed with the approval of the institutional review boards of National Cancer Center, Korea (NCC2014-0037).
Operations
All patients enrolled in the present study underwent a gastrectomy with D1 + β, or more, lymph node dissection. All patients who underwent gastrectomy were reviewed before and after surgery by all surgeons, all gastroenterologists, a radiologist, and a pathologist. The same surgical procedures and reconstruction methods were used by all of the surgeons. A distal subtotal gastrectomy was performed if there was a tumor-free margin of 5 cm in cases with advanced gastric carcinoma or 2 cm in cases with early gastric carcinoma. The extent of the lymph node dissection was determined by the recommendations of the Japanese Research Society for Gastric Carcinoma.15 Cancers were staged according to the tumor node metastasis (TNM) classification system as reported by the Union International Contra la Cancrum (UICC). A potentially curative resection was defined as an R0 resection in accordance with the UICC residual tumor classification.16
Pathologic Examination
All pathology specimens were examined immediately after resection. All lymph nodes were retrieved by palpation under gross inspection. No size limitation was specified for lymph node harvesting. All pathological examinations were performed in a standard manner. The entire tumor was sectioned into 4-mm-thick sections (2 mm for ESD specimens), embedded in paraffin blocks and stained with hematoxylin and eosin. All HE slides were reviewed by the expert gastric pathologists (MC Kook) to validate UD-min, lymphovascular invasion (LVI), ulcer, invasion depth, and lymph node metastasis. The presence of UD-min was confirmed by the consensus of two expert gastric pathologists (MC Kook and HS Han). The cases were classified according to the presence of UD-min (supplemental Fig. 1). The proportion of UD-min was measured with a semiquantitative three-tiered system: no more than 10 %, no more than 30 %, or no more than 50 % of total tumor volume.
Evaluation of Ulcer
The presence of ulcer was determined based on the full-layer disruption of muscularis mucosa, including both the active and the healing stage. Some of the ulcers showed sharply demarcated margins surrounded by almost normal mucosa and their widths of the disrupted area were small (supplemental Fig. 2A). These cases could be considered as the possibility of iatrogenic ulcer caused by an endoscopic biopsy. There was no reasonable criterion to distinguish an iatrogenic ulcer from a true ulcer. We put the cases into the “ulcer presence” group when the width of the disruption of muscularis mucosa was large enough (more than 4 mm) to be hardly generated by endoscopic biopsy (supplemental Fig. 2B).
Statistical Analysis
The continuous variables measured in this study were expressed as the mean and the standard deviation (SD). Between-group comparisons of continuous variables were made using Student’s t test, and between-group comparisons of categorical variables were made using the χ 2 test. For the risk of lymph node metastasis, univariate and multivariate analyses were performed using the Poisson regression model. A two-sided p value <0.05 was considered statistically significant. All statistical analyses were carried out using STATA ver. 11 (College Station, TX).
Results
Clinical and Pathologic Patient Characteristics
The median age of the 847 patients was 62 years (range 28–88 years), and there were 615 (72.6 %) males and 232 (37.4 %) females. Sixty-two (7.3 %) of the gastric cancers were located in the upper third of the stomach, and the other 785 were located in the middle or lower third (Table 1).
Characteristics of Tumors with UD-min
UD-min was observed in 25.4 % of total cases. The presence of UD-min associated with female, younger age, larger tumor size, and the presence of ulcer. The location of the tumor and the presence of lymphovascular invasion were not related with the UD-min (Table 1). The incidence of both ulcer and UD-min presence increased as tumor size increased: ≤2 cm, 8/314 (2.5 %); 2< to ≤3 cm, 20/200 (10 %); >3 cm, 58/333 (17.4 %) (p < 0.001).
Risk of Lymph Node Metastasis
Pathologic examinations showed that 14 patients (1.7 %) had metastatic lymph nodes. Younger age, larger tumor size, the presence of ulcer, and lymphovascular invasion were related to lymph node metastasis. The rate of lymph node metastasis was 5.1 % (11/215 patients) in tumors with UD-min. As the proportion of the UD-min increased, the rate of lymph node metastasis increased. The increase of lymph node metastasis was statistically significant when the proportion of UD-min was more than 10 % (Table 2). UD-min also was significantly associated with lymph node metastasis in multivariate analyses like other known risk factors for lymph node metastasis, including tumor size, the presence of lymphovascular invasion, and ulcer (Table 3).
Stratification of the Rate of Lymph Node Metastasis with ESD Indications and Risk Factors
No lymph node metastasis was shown in absolute ESD indication cases (0/245). In the tumors of expanded indications for ESD, a few tumors (3/430, 0.7 %) metastasized to lymph nodes (Table 4).
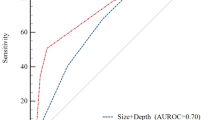
We stratified the rate of lymph node metastasis according to the combinations of four risk factors, including tumor size and the presence of lymphovascular invasion, ulcer, and UD-min (Table 5). When lymphovascular invasion was present or all of three other risk factors (tumor size >2 cm, ulcer and UD-min) were present concurrently, the rate of lymph node metastasis was high (10–25 %). Lymph node metastasis was absent or present in a very low frequency in other cases (0–1.2 %).
Discussion
The main findings of this study are as follows: (1) 215 differentiated tumors (25.4 %) had UD-min histology, (2) the rate of lymph node metastasis in mucosal cancers with differentiated histology mixed with UD-min was higher than that of mucosal cancer with differentiated histology only (5.1 vs. 0.5 %, p < 0.001), (3) UD-min was an independent risk factor for lymph node metastasis in early gastric cancer confined to mucosa, especially the proportion of UD-min was more than 10 % of total tumor volume, (4) several tumors (3/430, 0.7 %) among expanded indications metastasized to lymph node, and (5) the rate of lymph node metastasis was high (10–25 %) when lymphovascular invasion was present or all of three other risk factors (tumor size >2 cm, ulcer, and UD-min) were present.
A gastrectomy is associated with considerable postoperative discomfort, e.g., abdominal pain, nausea, vomiting, and dumping syndrome.17 Although pylorus and vagus nerve-preserving gastrectomies have been attempted to prevent postgastrectomy syndrome, the results have not been encouraging.18,19 Therefore, preservation of the stomach provides the best means of preventing this syndrome. Lymph node metastasis is the most important consideration when determining whether the stomach can be preserved.5
We found that the rate of lymph node metastasis of mucosal cancers with differentiated type histology was 1.7 %, similar to those of previous studies for mucosal cancers (0.4–1.8 %). However, when limited to UD-min present cases, the rate of lymph node metastasis was much higher than that of UD-min–negative cases. In Takizawa’s study, about the rate of lymph node metastasis in mucosal cancers, cancers with differentiated type histology mixed with undifferentiated component showed a higher rate of lymph node metastasis than cancers with pure differentiated type histology, but the difference was not great enough to be statistically significant.20 In the present study, the number of cases was higher and thus showed statistically significant difference and independent predictive power.
Furthermore, we demonstrated the stratification including UD-min factor could be more helpful to consider the curative resection status for ESD, because the rate of lymph node metastasis was much higher in the cases of both UD-min and ulcer present. Recently, Min et al. reported the impact of UD-min on the long-term outcome after ESD.21 Recurrence was absent in UD-min cases meeting the expanded curative resection criteria (0/40), including sm1 invasion cases. Their cases consisted of ESD-treated cases only and it is difficult to compare to our cases directly. However, the incidence of ulcer or co-presence of ulcer and UD-min was not described in their data. In our study, the rate of lymph node metastasis in UD-min cases of expanded curative resection criteria was 2.3 % (2/87). The rate was significantly increased to 7.1 % (2/28) for cases with both risk factors present: UD-min and ulcer. Based on our data, we suggest that a stratification using risk factors for lymph node metastasis should be applied to survival analysis of ESD cases, and a further large-scale study is needed for such an analysis.
Several studies reported the clinical significance of heterogenous components. Mita reported that the differentiated type submucosal invasive cancers containing undifferentiated component showed higher rate of lymph node metastasis than pure differentiated type cancers.22 Hanaoka reported that undifferentiated type submucosal invasive cancers mixed with differentiated component showed more frequent lymph node metastasis even than the pure undifferentiated type cancers.23 Similar result was reported in Zheng’s study; based on Lauren classification mixed-type carcinomas have higher rates of lymph node metastasis and a worse prognosis than diffuse-type carcinomas.24 Carneiro suggested a classification system modified from Lauren classification and emphasized the poor prognosis of the “mixed-type” showing heterogeneity consisting of the isolated component and other components.25 All of these studies were for submucosal cancers, the populations of which the majority were advanced cases. The results of present study suggest the significance of heterogeneity can be still valid in mucosal cancers.
In the Japanese Gastric Cancer Treatment Guidelines 2011, the criteria for a curative resection in ESD consist of histologic type, tumor size, invasion depth, ulcer, lymphovascular invasion, and status of resection margin.26 In these guidelines, it is tentatively recommended to regard as a noncurative resection if there is some component of undifferentiated type histology in case of an expanded indication because the evidence is still insufficient. The data of present study can provide useful information on this point. According to the data of the present study, the presence of UD-min was significantly associated with lymph node metastasis in ulcer-positive mucosal cancers, and it can be considered an indicator of a noncurative resection.
In the present study, we designated the cases with the full-layer disruption of muscularis mucosa wider than 4 mm as ulcer-present regardless healing status. The rate of ulcer presence was 33.4 %, similar to that of previous data in Japan (42.6 %).27 There were several reports in which the rate of ulcer was much lower (7.2–9.9 %).28,29 We suppose that only active ulcer were included in these studies. With regard to the interpretation error of biopsy-induced ulcers, we investigated their size and depth. We found that the ulcer was more than 4 mm in width or deep into proper muscle layer in all cases of lymph node metastasis associated with ulcer presence (data not shown). Therefore, we think the iatrogenic findings caused by endoscopic biopsy had no effect on our conclusions.
In the tumors of expanded curative resection criteria for ESD, several cases metastasized to lymph nodes. This result is different from previous results of large-volume data in Japan showing no lymph node metastasis in those expanded criteria cases.27,30 Some reports from Korea also showed lymph node metastasis in the expanded criteria cases.31 It is difficult to find a reason for this difference.
Although present study revealed the risk of UD-min for lymph node metastasis with high statistical power, several limitations can be considered. First, in stratification analysis with risk factors the number of cases was small in several subgroups. Second, we did not classify the undifferentiated components into further subcategories. If the undifferentiated components are grouped into poorly tubular, signet ring cell, or mucinous histology, the possibility cannot be excluded that significant odd ratio for lymph node metastasis between the histologic subgroups is observed. However, the number of cases was not enough to do such a subgroup analysis. Third, it can be ideally applied to the curative resection status but may be difficult to ESD indication, because the detection of UD-min or ulcer is limited in endoscopy.
Conclusions
Minor undifferentiated type histology was associated with a number of characteristic findings and the presence of minor undifferentiated type histology in differentiated type mucosal cancer is an independent risk factor for lymph node metastasis. Our findings suggest that minor undifferentiated type histology should be considered when assessing curative resection status for endoscopic submucosal dissection.
References
Jung K-W, Won Y-J, Kong H-J, Oh C-M, Seo HG, Lee J-S. Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat. 2013;45(1):1–14.
Kunisaki C, Ishino J, Nakajima S, et al. Outcomes of mass screening for gastric carcinoma. Ann Surg Oncol. 2006;13(2):221–8.
Kim JP. Surgical results in gastric cancer. Paper presented at: Seminars in Surgical Oncology; 1999.
Jeong O, Park Y-K. Clinicopathological features and surgical treatment of gastric cancer in South Korea: the results of 2009 nationwide survey on surgically treated gastric cancer patients. J Gastric Cancer. 2011;11(2):69–77.
Soetikno R, Kaltenbach T, Yeh R, Gotoda T. Endoscopic mucosal resection for early cancers of the upper gastrointestinal tract. J Clin Oncol. 2005;23(20):4490–8.
Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N, Group JLSS. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007;245(1):68.
Habermann CR, Weiss F, Riecken R, et al. Preoperative staging of gastric adenocarcinoma: comparison of helical CT and endoscopic US 1. Radiology. 2004;230(2):465–71.
Isomoto H, Shikuwa S, Yamaguchi N, et al. Endoscopic submucosal dissection for early gastric cancer: a large-scale feasibility study. Gut. 2009;58(3):331–6.
Goto O, Fujishiro M, Kodashima S, Ono S, Omata M. Outcomes of endoscopic submucosal dissection for early gastric cancer with special reference to validation for curability criteria. Endoscopy. 2009;41(02):118–22.
Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. World Health Organization; 2010.
Association JGC. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14(2):101–12.
Saito A, Shimoda T, Nakanishi Y, Ochiai A, Toda G. Histologic heterogeneity and mucin phenotypic expression in early gastric cancer. Pathol Int. 2001;51(3):165–71.
Dinis-Ribeiro M, Pimentel-Nunes P, Afonso M, Costa N, Lopes C, Moreira-Dias L. A European case series of endoscopic submucosal dissection for gastric superficial lesions. Gastrointest Endosc. 2009;69(2):350–5.
An JY, Baik YH, Choi MG, Noh JH, Sohn TS, Kim S. Predictive factors for lymph node metastasis in early gastric cancer with submucosal invasion: analysis of a single institutional experience. Ann Surg. 2007;246(5):749–53.
Nakajima T. Gastric cancer treatment guidelines in Japan. Gastric Cancer. 2002;5(1):1–5.
Sobin LH, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. Hoboken: Wiley; 2011.
Kim Y-W, Baik YH, Yun YH, et al. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg. 2008;248(5):721–7.
Morii Y, Arita T, Shimoda K, et al. Jejunal interposition to prevent postgastrectomy syndromes. Br J Surg. 2000;87(11):1576–79.
Morita S, Katai H, Saka M, Fukagawa T, Sano T, Sasako M. Outcome of pylorus‐preserving gastrectomy for early gastric cancer. Br J Surg. 2008;95(9):1131–5.
Takizawa K, Ono H, Kakushima N, et al. Risk of lymph node metastases from intramucosal gastric cancer in relation to histological types: how to manage the mixed histological type for endoscopic submucosal dissection. Gastric Cancer. 2012; 16:531–536.
Min B-H, Kim K-M, Park CK, et al. Outcomes of endoscopic submucosal dissection for differentiated-type early gastric cancer with histological heterogeneity. Gastric Cancer. 2014; 1–9. doi:10.1007/s10120-014-0378-7.
Mita T, Shimoda T. Risk factors for lymph node metastasis of submucosal invasive differentiated type gastric carcinoma: clinical significance of histological heterogeneity. J Gastroenterol. 2001;36(10):661–8.
Hanaoka N, Tanabe S, Mikami T, Okayasu I, Saigenji K. Mixed-histologic-type submucosal invasive gastric cancer as a risk factor for lymph node metastasis: feasibility of endoscopic submucosal dissection. Endoscopy. 2009;41(05):427–32.
Zheng H-c, Li X-h, Hara T, et al. Mixed-type gastric carcinomas exhibit more aggressive features and indicate the histogenesis of carcinomas. Virchows Arch. 2008;452(5):525–34.
Carneiro F. Classification of gastric carcinomas. Curr Diagn Pathol. 1997;4(1):51–9.
Association JGC. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011;14(2):113–23.
Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3(4):219–25.
Choi J, Kim S, Im J, Kim J, Jung H, Song I. Comparison of endoscopic ultrasonography and conventional endoscopy for prediction of depth of tumor invasion in early gastric cancer. Endoscopy. 2010;42(09):705–13.
Higashimaya M, Oka S, Tanaka S, et al. Outcome of endoscopic submucosal dissection for gastric neoplasm in relationship to endoscopic classification of submucosal fibrosis. Gastric Cancer. 2012:1–7.
Haruta H, Hosoya Y, Sakuma K, et al. Clinicopathological study of lymph‐node metastasis in 1389 patients with early gastric cancer: assessment of indications for endoscopic resection. J Digest Dis. 2008;9(4):213–8.
Kang HJ, Kim DH, Jeon T-Y, et al. Lymph node metastasis from intestinal-type early gastric cancer: experience in a single institution and reassessment of the extended criteria for endoscopic submucosal dissection. Gastrointest Endosc. 2010;72(3):508–15.
Acknowledgment
This work was supported by a grant from the National Cancer Center (NCC-1110240).
Disclosure
The authors declare no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jun Ho Lee and Il Ju Choi have contributed equally to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10434_2014_4167_MOESM1_ESM.tif
Supplemental Fig. 1 Pathologic classification. A Differentiated type adenocarcinoma without undifferentiated component. B Differentiated type adenocarcinoma mixed with undifferentiated component
10434_2014_4167_MOESM2_ESM.tif
Supplemental Fig. 2 Representative cases of ulcer. The whole thickness of muscularis mucosa was disrupted and replaced by fibrosis or irregular muscle bundles. A Disruption was focal and well demarcated. B Large-sized disruption was present
Rights and permissions
About this article
Cite this article
Lee, J.H., Choi, I.J., Han, H.S. et al. Risk of Lymph Node Metastasis in Differentiated Type Mucosal Early Gastric Cancer Mixed with Minor Undifferentiated Type Histology. Ann Surg Oncol 22, 1813–1819 (2015). https://doi.org/10.1245/s10434-014-4167-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4167-7