Abstract
Introduction
Port-site metastases (PSMs) have been reported after laparoscopy in patients with peritoneal carcinomatosis (PC). We hypothesize that PSM is an independent negative predicting factor of survival in patients undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (CRS/HIPEC).
Methods
A retrospective review of a prospective database was conducted to search patients who underwent laparoscopy prior to CRS/HIPEC. Most of the tumors were of appendiceal origin. All previous laparoscopy port sites were excised regardless of macroscopic tumor involvement. Patients were divided into two groups: patients with PSM [PSM (+)] and patients without PSM [PSM (−)]. Overall survival (OS) was estimated by Kaplan–Meier curves and the log-rank test. Cox regression [hazard ratios (HRs) and 95 % confidence intervals (CIs)] was used to test for independent effects of the PSM (+) and the associated clinicopathological variables.
Results
Sixty-five patients had laparoscopy before CRS/HIPEC. One hundred and forty-four port-sites were resected; 41 (29 %) ports were positive for malignancy in a total of 22 (34 %) patients. Mean OS at 1, 3, and 5 years was 88, 66, and 63 %, respectively. Survival in patients with PSM was 73, 35, and 23 %, respectively, compared with 95, 82, and 82 %, respectively, in patients without PSM (p ≤ 0.001). Positive lymph nodes (LNs) were detected in 13/22 patients with PSM and 11/43 patients without PSM. Independent effects on survival shows an HR of 3.136, 95 % CI 1.150–8.549 (p = 0.026) for LN metastases, and an HR of 3.462, 95 % CI 1.198–10.006 (p = 0.022) in patients with positive PSM.
Conclusion
PSMs are common in patients with PC undergoing CRS/HIPEC and are independently associated with a worse prognosis. Resection of previous laparoscopy port sites is advocated in patients with PC to ensure complete cytoreduction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (CRS/HIPEC) offers an effective therapeutic alternative for selected patients with abdomino-pelvic malignancies (mesothelial, gastrointestinal, and gynecological origin) with peritoneal dissemination who otherwise would have a dismal prognosis.1 – 4 The feasibility and outcomes of CRS/HIPEC depends on the extent of disease and the completeness of macroscopic cytoreduction (CC).5 – 7 Many patients undergoing CRS/HIPEC have had previous open or laparoscopic surgeries. There has been a recent trend to utilize diagnostic laparoscopy in patients with peritoneal carcinomatosis (PC) as an assessment tool for possible CRS/HIPEC candidates.8,9 Therefore, abdominal wall recurrence and growth of port-site metastasis remains a serious practical concern.
Broadly defined, port-site metastasis (PSM) is the recurrence of tumor at the wound sites created by the placement of ports for passing instruments or retrieving specimens in laparoscopic surgery.10 The reported incidence of tumor seeding in laparoscopic surgery has changed notably compared with early publications. Recently, PSMs have declined from 21 % to less than 1 %, and, in most cases, the metastatic port-site spread occurs synchronously with disease at another anatomical site.10 – 13 PSM is not commonly considered a clinically relevant event, but rather a marker of advanced (metastatic) disease. Consequently, this type of recurrence is not believed to impact long-term prognosis.14 – 17
The purpose of this study was to document the incidence and evaluate the prognostic value and therapeutic implications of PSM in patients with PC undergoing CRS/HIPEC.
Methods
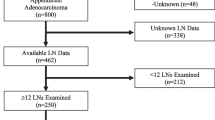
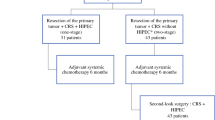
A review of a prospective database of 350 patients with PC who underwent CRS/HIPEC between April 2003 and July 2013 was conducted. Patients diagnosed with PC of abdomino-pelvic origin (gastrointestinal, mesothelial, and gynecological) with a history of a laparoscopic procedure prior to CRS/HIPEC, regardless of its indication, were included. CRS/HIPEC was conducted as previously described by our group.7,18 It is our practice to perform the abdominal wall resection of all identified previous port sites as a routine procedure during CRS/HIPEC, irrespective of pre- or intraoperative evidence of macroscopic tumor involvement. Midline port sites were included in the midline laparotomy incision when possible; however, additional port-site scars or tracts resulting from the abdominal wall components shift as the effect of insufflation during laparoscopy were also resected. All resected port-site specimens were submitted separately for routine pathological examination. PSM was defined as pathologic confirmation of malignancy in the specimen labeled as port site (scar/tract). Assessment of the extent of the disease was made at the beginning of and after CRS/HIPEC by calculating the peritoneal cancer index (PCI). Extensive disease was defined as PCI ≥20. Once the cytoreductive procedure was accomplished, the residual volume of disease was estimated according to the standardized complete CC score.6,19 Primary tumors included gastrointestinal origin (appendix, colon, small bowel, and gastric), mesothelioma, and gynecologic malignancies (primary peritoneal, ovarian, and fallopian tube). Based on pathological evaluation, the patients were divided into two groups—patients with malignant port-site involvement [PSM (+)] and patients without malignant port-site involvement [PSM (−)].
The variables analyzed included age, sex, origin of the primary tumor, purpose/indication of laparoscopic procedures, interval between laparoscopy and CRS/HIPEC, PCI, CC score, and lymph node (LN) metastases. The data were collected prospectively at follow-up visits according to the standard postoperative schedule: 3 weeks, 3 months, and every 6 months thereafter. Demographics and other relevant variables of the sample were reported with descriptive statistics. Overall survival (OS) was calculated from the date of CRS/HIPEC to the date of last known follow-up or the date of death. Survival curves were estimated using the Kaplan–Meier method. Significant differences between groups were determined by the matched log-rank test. Univariate and multivariate Cox proportional regression analysis [reporting hazard ratios [HR] and 95 % confidence intervals (CIs)] was used to test for independent effect of the positive port-site involvement and the associated clinicopathological variables to determine their association with survival. Results were considered statistically significant if p < 0.05 was obtained. The statistical analyses were performed using SPSS 20 software (IBM Corporation, Armonk, NY, USA).
Results
A total of 65 patients undergoing CRS/HIPEC due to PC had a prior laparoscopic procedure. In 45 (69 %) of these patients, the laparoscopic procedure was performed for diagnosis of suspected malignancy, to stage a known tumor, or to assess the extent of disease for possible CRS/HIPEC. Twenty of 65 (31 %) were incidental findings during procedures unrelated to the oncological diagnosis (gastric bypass procedure, routine appendectomy, etc.). Mean time interval between laparoscopic procedure and CRS/HIPEC was 6 months (range 3 weeks–84 months). Mean age at the time of CRS/HIPEC was 54 years (range 27–80), 24 patients were male (37 %) and 41 were female (63 %). Primary tumor origin included appendix (39), colorectal (6), small bowel (1), mesothelioma (5), gastric (2), primary peritoneal (8), ovarian (3), and fallopian tube (1) cancer. Forty (62 %) patients had PCI ≥20, while 24 (37 %) patients had LN metastases. CC was achieved in 62 (95 %) patients.
One hundred and forty-four full-thickness abdominal wall port sites were resected—85 at midline (umbilical 58 and upper/lower midline 27) and 59 off-midline (right upper quadrant 13, right lower quadrant 17, left upper quadrant 9, left lower quadrant 20). Forty-one (29 %) ports were positive for malignancy in 22 (34 %) patients. Forty-two percent of patients who underwent diagnostic laparoscopy for staging of a known tumor developed PSM, whereas PSMs were found in 15 % of patients who underwent laparoscopy for non-oncological reasons (p = 0.046). PSMs were found in 45 % of patients with PCI ≥20 and in 16 % of patients with PCI <20 (p = 0.030), as well as in 54 % of patients with LN metastasis compared with 22 % without LN metastasis (p = 0.014). Neither age, sex, interval between laparoscopy and CRS/HIPEC nor CC score were found to be associated with the presence of PSM (see Table 1). A descriptive relationship between the variables associated with PSM and the origin of the primary tumor is detailed in Table 2.
At a mean follow-up of 31 months (range 1–98 months), 46 of 65 (71 %) patients were alive, 35 (54 %) of whom exhibited no evidence of disease and 11 (17 %) were alive with disease. Nineteen (29 %) patients were dead—18 (28 %) from disease and 1 from another cause. PSMs were reported in 12 (63 %) of these patients. The OS of the entire cohort at 1, 3, and 5 years was 88, 66, and 63 %, respectively. OS in patients with PSM was 73, 35, and 23 %, respectively, with median survival of 2.4 years, compared with 95, 82, and 82 %, respectively, in patients without port-site malignant involvement (p ≤ 0.001) (Fig. 1a). Patients with presence of LN metastases had a median survival of 2.6 years compared with patients without LN metastases, who did not reach the median survival. The OS was 75, 44, and 33 %, respectively, in the group with LN metastases, and 95, 80, and 80 %, respectively, in patients without LN (p = 0.001) (Fig. 1b). In positive LN patients, the 5-year OS related to PSM was 0 % compared with 80 % of patients without PSM (p = 0.006) (Fig. 1c). Table 3 compares percentages of survival according to PSM and LN involvement.
A univariate analysis of PSM showed an HR of 5.477, 95 % CI 2.062–14.545 (p = 0.001). Cox regression with the associated clinicopathological variables in the model to test for independent effects on survival found an HR of 3.136, 95 % CI 1.150–8.549 (p = 0.026) for LN metastases, and an HR of 3.462, 95 % CI 1.198–10.006 (p = 0.022) in patients with PSM (Table 4). This indicates that LN metastases and PSM makes an independent negative contribution to patient survival.
Discussion
While the incidence and clinical significance of PSM in patients who underwent laparoscopic surgery with curative intent have been well researched,20,21 metastatic tumor seeding in surgical scars in the setting of PC in candidates for CRS/HIPEC has not been studied. To our knowledge, this study is the first systematic attempt to describe the incidence of PSM in a large cohort of patients with PC and the role of PSM as an independent prognostic factor in OS in this patient population.
The true incidence of PSM is unclear; it has been reported at a range of 1–21 %.10 – 13 The incidence of PSM in our cohort was higher than in these reports. One-third of patients (34 %) had PSM at the time of CRS/HIPEC. This higher rate of PSM might be related to the fact that all port-site scars were resected at the time of CRS/HIPEC independently of its macroscopic appearance, and that each site underwent histopathologic evaluation to avoid overlooking microscopic disease. This finding highlights the importance of scar/tract removal since its macroscopic appearance does not guarantee absence of tumor involvement. Since the microscopic tumor growing along the trocar tracts is not exposed to intraperitoneal chemotherapy during HIPEC, and CC is the ultimate goal of CRS, we strongly recommend excising all laparoscopy port sites.
Our results differ from previous studies where PSMs were not found at trocar sites after staging/diagnostic laparoscopy in patients with PC.9,22 This difference could be attributed to the timeframe associated with the procedures. In the Valle and Garofalo series, the laparoscopic procedures were performed 10–40 days prior to CRS/HIPEC, while in our study, laparoscopy was performed at a mean time interval of 6 months.9,22 The period between laparoscopic surgery and the clinical finding of PSM varies but most lesions arise between 3 and 9 months later, which could play a role in PSM incidence.23 – 25 At our institution, diagnostic laparoscopies were performed and followed by CRS/HIPEC within a mean timeframe of 4 weeks. However, most of the laparoscopic procedures were performed at other institutions and for different indications (not only for assessment of disease prior to CRS/HIPEC). In these patients, the time interval was longer. Frequently, the laparoscopic procedure was followed by other treatments such as systemic chemotherapy before referral to our center for CRS/HIPEC.
PSM was associated with the clinical indications for laparoscopy in this study. Patients with PC undergo laparoscopic procedures for three main reasons—diagnosis or staging, curative or palliative surgery, and procedures unrelated to oncological pathology (incidental findings).9,26 Not surprisingly, we observe a significant difference among patients undergoing laparoscopic procedures for oncologic versus non-oncologic indications. Patients who underwent diagnostic laparoscopy for tumor staging purposes had a higher rate of PSM (42 %) compared with patients who underwent laparoscopy for non-oncologic reasons (15 %) (p = 0.046). This finding supports previous reports of PSM involvement even in the absence of excessive tumor manipulation, which has been associated with port-site tumor seeding.12,21 PSM is an important risk to keep in mind while planning on a laparoscopic procedure in a patient with known or suspected PC.
PSM was associated with a worse OS compared with patients without port-site malignant involvement (23 vs. 82 % at 5 years, respectively; p < 0.001). However, OS in patients with PC has been related to several other risk factors, such as PCI, CC score, and LN metastases.18,27,28 In our series, PSM patients had higher mean PCI scores and LN metastases, which suggests that PSMs are related to extensive and more aggressive disease.14,15,24 The few available studies neither found association between the presence of PSM and peritoneal disease progression nor addressed the potential benefit of routine resection of laparoscopic port sites.16,29 – 31 Our data showed that PSM affected OS on univariate (HR 5.477; 95 % CI 2.062–14.545; p = 0.001) and multivariate (HR 3.462; 95 % CI 1.198–10.006; p = 0.022) analysis even after adjusting for such a poor prognostic factor as the presence of LN metastasis.27 Therefore, the resection of PSM is essential to achieve CC and, consequently, improve long-term survival of patients undergoing CRS/HIPEC.
The benefit of patient selection to undergo CRS/HIPEC remains a critical point. Thus, routine diagnostic laparoscopy has been recommended in an attempt to assess the extent of tumor dissemination, to predict the CC probability, and to avoid the chance of an aborted HIPEC procedure.8,22,32,33 However, the occurrence of PSM is a finding of real concern, demonstrated in our series. PSM may reflect the tumor biology or potential iatrogenic consequences of laparoscopy. Since tumor biology is not subject to change, we suggest the following surgical strategy. First, midline placement of ports, as suggested by Pomel et al.32 and Iversen et al.,34 will allow for easier and more complete excision of PSM, achieving a true CC, at the time of the CRS/HIPEC. Second, the procedure should be carried out by the same surgical team that is treating the peritoneal surface malignancy, when possible; thus, the extent of tumor involvement and CRS/HIPEC feasibility could be evaluated. Third, CRS/HIPEC should be performed in a timely manner to avoid the development of PSM which is associated with poor prognosis. We believe that appropriate planning of this surgical procedure will help to avoid the difficulties of trocar positioning in the presence of abdominal wall tumor masses or adhesions from previous surgeries, and the expected fear of neoplastic contamination of port sites in patients with PC.9,22,32
Undoubtedly, there are methodological issues that may not permit generalization of these findings. Limitations such as selection bias, due to the heterogeneity of primary tumor sites and underlying differences in the histopathologic grade of tumor, must be considered, as well as the variety of indications for the laparoscopic procedure. These variables, in addition to the fact that our study was a retrospective analysis, may make it difficult to extrapolate our results.
Conclusions
Our study is the first to describe PSM as a common clinicopathological entity present in patients with PC who undergo CRS/HIPEC and represent an independent poor prognostic factor for OS. This finding raises the concern that this type of recurrence could jeopardize long-term outcomes of a potentially life-extending surgical treatment option for the management of peritoneal surface malignancies, especially if PSMs are left behind. Therefore, we strongly advocate the resection of previous laparoscopy port sites in all patients with PC in order to ensure a true CC during CRS/HIPEC.
References
Elias D, Goere D, Dumont F, et al. Role of hyperthermic intraoperative peritoneal chemotherapy in the management of peritoneal metastases. Eur J Cancer. 2014;50(2):332–340.
Elias DM, Ouellet JF. Intraperitoneal chemohyperthermia: rationale, technique, indications, and results. Surg Oncol Clin N Am. 2001;10(4):915–933, xi.
Sommariva A, Pilati P, Rossi CR. Cyto-reductive surgery combined with hyperthermic intra-peritoneal chemotherapy for peritoneal surface malignancies: current treatment and results. Cancer Treat Rev. 2012;38(4):258–268.
Sugarbaker PH. New standard of care for appendiceal epithelial neoplasms and pseudomyxoma peritonei syndrome? Lancet Oncol. 2006;7(1):69–76.
Chua TC, Moran BJ, Sugarbaker PH, et al. Early- and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Clin Oncol. 2012;30(20):2449–2456.
Esquivel J, Elias D, Baratti D, Kusamura S, Deraco M. Consensus statement on the loco regional treatment of colorectal cancer with peritoneal dissemination. J Surg Oncol. 2008;98(4):263–267.
Omohwo C, Nieroda CA, Studeman KD, et al. Complete cytoreduction offers longterm survival in patients with peritoneal carcinomatosis from appendiceal tumors of unfavorable histology. J Am Coll Surg. 2009;209(3):308–312.
Laterza B, Kusamura S, Baratti D, Oliva GD, Deraco M. Role of explorative laparoscopy to evaluate optimal candidates for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) in patients with peritoneal mesothelioma. In Vivo. 2009;23(1):187–190.
Valle M, Federici O, Garofalo A. Patient selection for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy, and role of laparoscopy in diagnosis, staging, and treatment. Surg Oncol Clin N Am. 2012;21(4):515–531.
Ouellette JR, Ko AS, Lefor AT. The physiologic effects of laparoscopy: applications in oncology. Cancer J. 2005;11(1):2–9.
Curet MJ. Port site metastases. Am J Surg. 2004;187(6):705–712.
Ziprin P, Ridgway PF, Peck DH, Darzi AW. The theories and realities of port-site metastases: a critical appraisal. J Am Coll Surg. 2002;195(3):395–408.
Chua TC, Yan TD, Morris D, Sugarbaker PH. Port-site metastasis following laparoscopic surgery. Adv Laparosc. 2011.
Ramirez PT, Wolf JK, Levenback C. Laparoscopic port-site metastases: etiology and prevention. Gynecol Oncol. 2003;91(1):179–189.
Shoup M, Brennan MF, Karpeh MS, Gillern SM, McMahon RL, Conlon KC. Port site metastasis after diagnostic laparoscopy for upper gastrointestinal tract malignancies: an uncommon entity. Ann Surg Oncol. 2002;9(7):632–636.
Velanovich V. The effects of staging laparoscopy on trocar site and peritoneal recurrence of pancreatic cancer. Surg Endosc. 2004;18(2):310–313.
Dijkum V, Nieveen EJ, de Wit LT, Obertop H, Gouma DJ. Port-site metastases following diagnostic laparoscopy. Br J Surg. 1996;83(12):1793–1794.
El Halabi H, Gushchin V, Francis J, et al. The role of cytoreductive surgery and heated intraperitoneal chemotherapy (CRS/HIPEC) in patients with high-grade appendiceal carcinoma and extensive peritoneal carcinomatosis. Ann Surg Oncol. 2012;19(1):110–114.
Sugarbaker PH. Peritonectomy procedures. Surg Oncol Clin N Am. 2003;12(3):703–727, xiii.
Zivanovic O, Sonoda Y, Diaz JP, et al. The rate of port-site metastases after 2251 laparoscopic procedures in women with underlying malignant disease. Gynecol Oncol. 2008;111(3):431–437.
Zmora O, Weiss EG. Trocar site recurrence in laparoscopic surgery for colorectal cancer. Myth or real concern? Surg Oncol Clin N Am. 2001;10(3):625–638.
Garofalo A, Valle M. Laparoscopy in the management of peritoneal carcinomatosis. Cancer J. 2009;15(3):190–195.
Neuhaus SJ, Texler M, Hewett PJ, Watson DI. Port-site metastases following laparoscopic surgery. Br J Surg. 1998;85(6):735–741.
Schaeff B, Paolucci V, Thomopoulos J. Port site recurrences after laparoscopic surgery: a review. Dig Surg. 1998;15(2):124–134.
Rao S, Rathod A, Kamble AT, Gupta D. Delayed presentation of port-site metastasis from an unknown gastrointestinal malignancy following laparoscopic cholecystectomy. Singapore Med J. 2014;55(5):e73–76.
Sommariva A, Zagonel V, Rossi CR. The role of laparoscopy in peritoneal surface malignancies selected for hyperthermic intraperitoneal chemotherapy (HIPEC). Ann Surg Oncol. 2012;19(12):3737–3744.
Halabi HE, Gushchin V, Francis J, et al. Prognostic significance of lymph node metastases in patients with high-grade appendiceal cancer. Ann Surg Oncol. 2012;19(1):122–125.
Van Sweringen HL, Hanseman DJ, Ahmad SA, Edwards MJ, Sussman JJ. Predictors of survival in patients with high-grade peritoneal metastases undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Surgery. 2012;152(4):617–624.
Maker AV, Butte JM, Oxenberg J, et al. Is port site resection necessary in the surgical management of gallbladder cancer? Ann Surg Oncol. 2012;19(2):409–417.
Wu JS, Guo LW, Ruiz MB, Pfister SM, Connett JM, Fleshman JW. Excision of trocar sites reduces tumor implantation in an animal model. Dis Colon Rectum. 1998;41(9):1107–1111.
Muntean V, Oniu T, Lungoci C, et al. Staging laparoscopy in digestive cancers. J Gastrointestin Liver Dis. 2009;18(4):461–467.
Pomel C, Appleyard TL, Gouy S, Rouzier R, Elias D. The role of laparoscopy to evaluate candidates for complete cytoreduction of peritoneal carcinomatosis and hyperthermic intraperitoneal chemotherapy. Eur J Surg Oncol. 2005;31(5):540–543.
Valle M, Garofalo A. Laparoscopic staging of peritoneal surface malignancies. Eur J Surg Oncol. 2006;32(6):625–627.
Iversen LH, Rasmussen PC, Laurberg S. Value of laparoscopy before cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis. Br J Surg. 2013;100(2):285–292.
Disclosures
Maria F. Nunez, Armando Sardi, William Jimenez, Carol Nieroda, Michelle Sittig, Ryan MacDonald, Nail Aydin, Vladimir Milovanov, and Vadim Gushchin declare that there are no financial or commercial interests in the present study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nunez, M.F., Sardi, A., Jimenez, W. et al. Port-Site Metastases is an Independent Prognostic Factor in Patients with Peritoneal Carcinomatosis. Ann Surg Oncol 22, 1267–1273 (2015). https://doi.org/10.1245/s10434-014-4136-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4136-1