Abstract
The focus of the research was to overcome the limitations of metoclopramide (MTC) when administered intranasally. The aim was to improve its bioavailability, increase patient compliance, and prolong its residence time in the nasal cavity. MTC-loaded liposomes were prepared by applying the film hydration method. A study was conducted to determine how formulation variables affected encapsulation efficiency (EE %), mean particle size (MPS), and zeta potential (ZP). The MTC-liposomes were further loaded into the in situ gel (gellan gum) for longer residence times following intranasal administration. pH, gelling time, and in vitro release tests were conducted on the formulations produced. In vivo performance of the MTC-loaded in situ gels was appraised based on disparate parameters such as plasma peak concentration, plasma peak time, and elimination coefficient compared to intravenous administration. When the optimal liposome formulation contained 1.98% of SPC, 0.081% of cholesterol, 97.84% of chloroform, and 0.1% of MTC, the EE of MTC was 83.21%, PS was 107.3 nm. After 5 h, more than 80% of the drug was released from MTC-loaded liposome incorporated into gellan gum in situ gel formulation (Lip-GG), which exhibited improved absorption and higher bioavailability compared to MTC loaded into gellan gum in situ gel (MTC-GG). Acceptable cell viability was also achieved. It was found out that MTC-loaded liposomal in situ gel formulations administered through the nasal route could be a better choice than other options due to its ease of administration, accurate dosing, and higher bioavailability in comparison with MTC-GG.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over the past few decades, nanosized drug delivery systems have been extensively examined as a novel approach to overcome the low bioavailability of numerous pharmaceutical drugs [1]. Vesicular carriers offer additional advantages, such as protecting active compounds from chemical and enzymatic degradation and the potential to prolong the duration of medication in the bloodstream [2]. Among these carriers, liposomes have received the most research attention, thanks to their biocompatible and biodegradable nature [3]. Numerous studies have been conducted on liposomes to reduce drug toxicity and target specific areas [4].
In recent years, the intranasal drug delivery system has garnered attention as a potential method for both systemic and local therapy [5]. A wide range of medications are delivered through the nasal cavity due to its unique physiology and anatomy, including its large surface area, porous endothelial membrane, highly vascular epithelium, and lack of first-pass metabolism. Intranasal administration has the advantage of providing faster onset of pharmacological activity, reduced doses, fewer adverse side effects, and faster achievement of therapeutic blood levels [6]. To enhance intranasal drug absorption, mucoadhesive polymers are often added to drug carriers to extend the dosage form’s contact or residence time within the nasal mucosa [7]. Simple aqueous solutions with viscosity-increasing agents have been used as a straightforward formulation approach to prolong the time drugs spend in the nasal cavity area after administration. Recent research has shown that in situ gelling formulations are more effective than nasal liquid formulations, especially for medications that are regularly taken [7]. Additionally, the rapid absorption rate and quick onset of action of the intranasal route make it crucial for managing emergency situations, such as severe nausea and vomiting. This is particularly important for antiemetics taken orally, as vomiting can occur before systemic absorption, leading to low patient compliance [8,9,10].
One of these antiemetics is MTC, a white crystalline powder that is freely soluble in alcohol. It is a potent antiemetic with a well-studied pharmacological and toxicological profile. MTC is used to treat disorders associated with reduced gastrointestinal motility, such as gastroparesis, ileus, reflux, dyspepsia, and nausea and vomiting due to migraine, motion sickness, chemotherapy, and other conditions. The highly permeable and vascularized nasal mucosa ensures rapid onset of medication action, making it particularly effective in treating acute nausea and vomiting brought on by cancer treatment or migraines [11]. MTC can be administered in several ways. However, the parenteral route of MTC has limitations, including poor patient compliance, high cost, safety concerns, and the impracticality of self-administration [12]. When taken orally, MTC is immediately absorbed from the gastrointestinal tract. However, conditions like vomiting or impaired gastric motility can hinder its absorption. Consequently, MTC is characterized by variable bioavailability, ranging from 32 to 98%, due to its short half-life (3 to 4 h) and rapid first-pass metabolism, necessitating three or four daily administrations [12].
Nasal delivery appears to be a promising alternative for antiemetic drug administration. In situ gel systems are an efficient formulation technique for extending the residence time of MTC in the nasal medium, despite the limited permeability of MTC across the nasal mucosal membrane and the impact of mucociliary clearance. Mucociliary clearance is the physiological factor primarily responsible for reducing the duration of drug presence in the nasal environment [13]. In situ gel formulations work effectively to prevent rapid drug drainage when delivered as low-viscosity polymeric solutions, as they can be sprayed over a large surface area, ensuring optimal nasal deposition and transforming into gels upon contact with the mucosa. Various chemical or physical stimuli, including temperature, ionic strength, and pH, can influence the transition from solution to gel. The in vivo formation of a polymeric network prolongs the drug’s contact with the site of action and ensures a sustained release of its active components [14].
It is most common for biodegradable and biocompatible polymers to be used in the formulation of in situ gels to possess ionic and mucoadhesive properties to increase the effectiveness of the formulations. Sphingomonas elodea produces gellan gum as an exopolysaccharide by aerobic submerged fermentation. By complexing with cations and forming hydrogen bonds with water, double-helical segments are formed, followed by aggregation to form a 3-D network. In gellan gum solutions, the gelation mechanism is governed by the nature of the cations, and the divalent cation promotes gelation more effectively than the monovalent cation in gellan gum solutions [15].
As an alternative to in situ gelling systems, dual-functioning formulations comprising nanosystems (NSs), such as liposomes loaded into a mucoadhesive in situ gel vehicle, represent a recent innovative approach to extending drug permanence at the administration site and enhancing drug diffusion through the mucus. While NSs do not bind to mucus components, they should be capable of crossing the mucus barrier and reaching the mucosal surface, where they exert their action. Mucoadhesive in situ gels establish direct contact with the mucosal membrane, enhancing the retention of loaded nanosystems at the administration site.
The aim of present study is to develop MTC nasal in situ gel formulation. Moreover, to enhance drug delivery by developing an innovative composite mixture that combines liposome and in situ gel delivery systems, suitable for intranasal administration was produced. This approach aims to improve absorption and maintain stable plasma concentrations. The optimized MTC-loaded liposome with favorable MPZ, PDI, ZP, and EE was selected to produce Lip-GG formulation. In order to evaluate the Lip-GG, a wide range of parameters were involved including, viscosity, mechanical properties, viscosity, pH, in vitro, in vivo rabbit studies. Furthermore, Fourier transform infrared spectroscopy (FTIR-ATR) analysis and differential scanning calorimetry (DSC) were also adopted for Lip-GG assessment.
Material and Methods
Materials
Metoclopramide (MTC) was kindly provided by the Ministry of National Defense Pharmaceutical Company (Ankara, Turkey). Phytagel® (gellan gum) and soybean phosphatidylcholine (SPC) were obtained from Sigma-Aldrich in Munich, Germany. Cholesterol was purchased from Sigma-Aldrich Chemie GmbH in Japan. Chloroform was acquired from Avantor Performance Materials in Poland S.A. Sodium chloride, potassium chloride, and calcium chloride were sourced from Sigma-Aldrich in Munich, Germany. Purified water used in HPLC and for sample preparation was produced using a Millipore Super Purity Water System (Millipore, USA). Krebs buffer was purchased from Caisson Lab in Smithfield, USA.
Methods
Preparation of Liposomes
A thin-film hydration method was used to prepare MTC-loaded liposomes [16]. In a flask, 10 mL of chloroform was used to dissolve SPC, cholesterol, and MTC. Following this, a thin film was formed by placing the flask in a rotary evaporator (Heidolph, Germany). Following the evaporation of the organic phase, nitrogen gas was passed through the formulation to prevent phospholipids from oxidizing. Distilled water was subsequently added and sonicated for 2–3 min, followed by probe sonication (10 min, 70% amplitude, x7 cycles). The final formulation solution was allowed to cool to room temperature (23 ± 0.5°C) and then stored in the refrigerator.
Experimental Design
D-optimal design was employed to assess the effects of four independent variables on four response variables, which included zeta potential (ZP), mean particle size (MPS), polydispersity index (PDI), and encapsulation efficiency (EE). The independent variables were the amounts of SPC (A), cholesterol (B), chloroform (C), and MTC (D). Previous studies were referenced to determine the parameter range for this investigation. To select the best-fitting model and enhance the process, Design-Expert® (version 13, Stat-Ease Inc., Minneapolis, MN, USA) was utilized.
Table I displays the variables and their respective levels used in the design. In order to determine the effects and regression coefficients of the various linear models, as well as the correlations between the variables, the analysis of variance tables was generated. A total of 16 combinations were generated by the experimental design. The best-fitting mathematical model was selected after evaluating several statistical parameters, including the coefficient of variation, the multiple correlation coefficient (R2), and the adjusted multiple correlation coefficient (adjusted R2). In order to assess the statistical significance of all terms in the polynomial, the F value was calculated at a probability of p < 0.05. In order to optimize the polynomials, numerical optimization was used. Experiments were conducted under the conditions listed in Table I in order to verify the ideal conditions.
Preparation of In Situ Gels
Gellan gum was prepared in four different concentrations (0.4%, 0.5%, 0.6%, and 0.7% w/v) to determine the best concentration. The required amount of gellan gum powder was dissolved in 20 mL of distilled water in a beaker with continuous stirring using a magnetic stirrer machine at 500 rpm for 30 min. Simulated nasal fluid (SNF), with a composition of 0.59 mg/mL CaCl2, 2.98 mg/mL KCl, and 8.77 mg/mL NaCl, was prepared [17]. The formulation was placed on a magnetic stirrer with a speed of 500 rpm until a clear solution was obtained. To select the best concentration of gellan gum, drops of the prepared SNF and gellan gum (0.4%, 0.5%, 0.6%, and 0.7%), in which the ratio was used of the solutions 1:1, were added to four small glass plates using a dropper, and the gelling capacity was assessed. Based on the results obtained, gellan gum with a concentration of 0.6% was chosen for further studies.
A pre-calculated amount of distilled water was added slowly to obtain a gellan gum solution. After stirring at 400 rpm and 35°C for 4 h, solutions containing 25 mg/mL (w/v) of the same amount of, or an appropriate amount of these solutions, were added to the liposomes. The mixture was further diluted with water to achieve the desired weight fraction. Until used, all formulations were kept in the refrigerator (4°C) [18].
Quantification of MTC
The amount of MTC was measured using an HPLC system, which included a gradient pump, an Agilent 1100 UV detector (Thermo Scientific, Germany), and a C18 column (Fisher Scientific, Pittsburgh, PA) (5 µm, 150 × 4.6 mm). The samples were examined at a temperature of 25°C and a wavelength of 280 nm. Acetonitrile and potassium phosphate buffer (pH 3.5) were combined in an 80:20 v/v ratio as the mobile phase. The flow rate was 1.5 mL/min, and the injection volume was 10 µL.
In order to validate the HPLC method, international guidelines on analytical techniques for pharmaceutical quality control were followed [19]. In order to validate the method, linearity, limits of detection (LOD) and quantitation (LOQ), accuracy, precision, specificity, selectivity, and stability were evaluated. Using standard solutions of MTC (5 mg/mL), a calibration curve was constructed to determine the linear relationship between peak area and concentration.
Characterization Studies of Liposome Formulation
Particle Size Distribution and Zeta Potential
In order to measure MPS and PDI, the method of differential light scattering (DLS) was used (Nano ZS 3600 from Malvern Instruments, Chester County, PA, USA). PDI values below 0.25 indicate homogeneous particle size distributions, while values higher than 0.5 indicate heterogeneous particle size distributions. By operating the DLS in zeta mode, zeta potential was also measured. Zeta potential measurements were conducted using electrocuvettes [20].
Determination of Encapsulation Efficiency
In order to determine the encapsulation efficiency of MTC in liposomal dispersion, an indirect method was employed. The amount of MTC trapped in the liposomes must be calculated by subtracting the quantity of non-entrapped MTC that remains in the supernatant from the total amount added to the loading solution. Liposome suspension was centrifuged (10,000 rpm, 20 min) and supernatant was separated. The amount of MTC in supernatant was determined by HPLC method. Encapsulation efficiency was calculated using the following formula: [21]
where qu is the amount of unloaded MTC (mg/mL) and qt is the total MTC quantity of taken (mg/mL).
Scanning Electron Microscopy (SEM) Analysis
Liposomes were characterized morphologically using a scanning electron microscope (SEM) (Quattro S, Thermo Scientific, Iowa, IL, USA). In the SEM, samples were accelerated to 15.00 kV and sputtered with gold and palladium (LEICA EM ACE200, Leica Microsystems, Germany) at 3 kV for 60 s. Images were captured under conditions of high vacuum using a scanning electron microscope at various magnifications [20].
Stability Studies
The stability of MTC-loaded liposomes and Lip-GG formulation and Lip-GG formulation after passage through a device that stimulates nasal administration was monitored was monitored for 5 weeks. The samples were stored at 4 ± 0.5°C in amber-colored glass containers. Triplicate samples were withdrawn at 0, 1, 2, 4, and 5 weeks for the analysis of MPS, PDI, ZP, and EE [22].
Characterization Studies of In Situ Gels
Mechanical Properties
In order to analyze texture, a TA-XT Plus Texture Analyser (Stable Micro Systems, Edinburgh, UK) fitted with a 2-kg load cell set to the texture profile analysis mode with a range of 0–100 N was used [23]. As a sample holder, a 15-mm-diameter cylindrical probe was used. A 3-cm-diameter petri dish was used for the initial transfer of the formulations. There was a delay period of 15 s between the end of the first compression and the beginning of the second compression in each formulation, where an analytical probe was inserted twice at a defined depth (50 mm) and at a defined rate (1 mm/s). The force-time curve led to the derivation of mechanical parameters (hardness, compressibility, adhesiveness, and cohesiveness) [23, 24] (n = 3).
Determination of pH and Viscosity
A calibrated pH meter (SevenExcellence S400 Benchtop, Mettler Toledo Greifensee, Switzerland) was used to measure the pH of the in situ gel formulations. An average pH value for the formulations was calculated by repeating the pH measurement (n = 3).
The viscosities of the formulations were determined using a Brookfield DV2 viscometer (Lazar Scientific, Inc. South Bend, Indiana, USA), accompanied by a 0.7 numbered probe from Brookfield. The measurements were taken at 25°C temperature, at a speed of 100 rpm and with a torque of 0.5%. It is important to note that each measurement was repeated five times to ensure accuracy [25].
Spreadability
The spreadability of the gel was determined by placing the formulations between the slides and exposing them to 1 kg of tension for 5 min. The spreadability of the gel has been expressed as the time elapsed (g.cm/s), after applying the 1-kg tension [26].
Fourier Transform Infrared Spectroscopy (FTIR-ATR) Analysis
Attenuated total reflectance (ATR) spectroscopy (Nicolet iS50 ATR, Thermo Fischer, Bremen, Germany) was employed for compatibility studies of the materials used in the preparation of in situ gel formulations. Spectra of the formulations were collected in the wavenumber range of 650–4000 cm−1. The formulations were directly placed on the equipment’s crystal. Multiple scans were conducted for each sample, and the force on the specimen was adjusted to achieve satisfactory transmittance results [20].
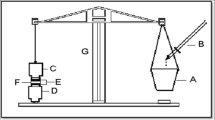
Differential Scanning Calorimetry
A small piece of each sample was divided into five-milligram pieces and placed in an aluminum pan that was sealed. A differential scanning calorimeter (DSC131, Setaram Inc., Caluire-et-Cuire, France) was used to raise the temperature to 300°C under a covering of nitrogen gas (50 µL/s) at a heating rate of 10°C/min [20].
In Vitro Drug Release
A Franz diffusion cell (Permegear, USA) with a diffusion area of 5.29 cm2 and a receiver volume of 20 mL was used to assess the release of MTC from the formulation. The membrane used was an artificial membrane, cellulose acetate membrane (Spectra/Por Regenerated Cellulose, molecular weight cutoff: 8–10 kDa). A Krebs buffer solution (pH, 6.6) was placed in a receiving compartment that was maintained at 37°C + 0.5°C [27]. After adding 2 g of formulations to 2 mL of ISF, the top of the Franz cell was sealed with parafilm. For up to 6 h, a 1-mL sample was collected every 30 min, taking care to prevent air bubbles in the receiver compartment, and was then replaced with equal amounts of fresh medium [28]. The concentrations of drugs in the samples were determined using HPLC analysis.
XTT Cytotoxicity Assay
Incubated in Advanced Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% (v/v) heat-inactivated fetal bovine serum, 10 mM l-glutamine, 10 mM HEPES, 100 ng/mL Noggin, FGF-10, 10 mM Nicotinamide, 1 mM N-acetyl cysteine, 10% (v/v) B-27 supplement, 50 ng/mL EGF, 10M SB202190, 20% R-spondin1 CM, and 100 IU/mL penicillin. In a CO2 atmosphere of 5%, the cells were incubated overnight. Incubation of the cells for an additional 24 h followed the treatment with drugs (Reference number: 20-300-1000, Sartorius, USA) [29, 30].
In Vivo Studies
An in vivo study was performed on six adult New Zealand rabbits weighing nearly 2.8 kilograms each to assess the bioavailability of MTC following nasal administration (approved by Yeditepe University Ethics Committee, Protocol number: 2021-062). It was determined the number of rabbits using a “Power Analysis” (experimental group 90%, control group 1%, alpha 0.05, beta 0.2, and power 80%). Using the power analysis, the total number of animals was determined to be six for significance. As a positive control group formulation, a parenteral (i.v.) marketed product of MTC was used. 3.6 mg/kg (10 mg/400 L total) of MTC was administered intravenously to each rabbit, with 200 µL applied to each nostril [31]. After the formulations were applied to the experimental animals, blood samples were collected at specific intervals from the marginal ear vein. The blood was collected in heparinized tubes at regular intervals, vortexed for 2 min, and centrifuged for 10 min at 3000 rpm. We used the Agilent 1100 UV detector (Thermo Scientific, Germany), a C18 column (Fisher Scientific Pittsburgh, PA) (5 µL, 150 × 4.6 mm) for our analysis. At 280 nm and 25°C, the analysis was conducted. An 80:20 v/v mixture of acetonitrile and potassium phosphate buffer (pH 3.5) was used as the mobile phase. Injection volume was 10 µL, flow rate was 1.5 mL/min, and flow rate was 1.5 mL/min [32].
Statistical Analysis
In this study, GraphPad Prism v. 5.04 software (Prism Inc., La Jolla, CA, USA) was used to conduct a one-way analysis of variance (ANOVA) followed by a Tukey’s multiple comparison test. It was decided to present the results in the form of either mean values with standard deviation (SD) or mean values with standard error of the mean (SEM). In the course of statistical comparisons and analysis, Student’s t-test was used, and statistical significance was defined as a p value of less than 0.05.
Results and Discussion
Preparation and Characterization of MTC-Contained Liposomes
To determine the compositions of four different ingredients, we employed a D-optimal experimental design using Design-Expert® (version 13.0.4.01, Stat-Ease Inc., Minneapolis, MN, USA). The effects of four independent variables, namely the amounts of SPC, cholesterol, chloroform, on four response variables (ZP, MPS, EE, and PI) were evaluated as presented in Table I and Fig. 1. We utilized the thin film hydration approach to create API-loaded liposomes (API-Lip), which were subsequently characterized.
A list of the fitting models, equations, and statistical parameters is provided in Table II. We used a significance level of p < 0.05 for our analysis. A three-dimensional response surface graph was generated using Design Expert® software based on equations. Based on the desirability approach, optimal parameters were determined for the formulations [33]. There were 16 combinations in the design, including five replications at the central point. The effect and regression coefficients of each linear model, as well as the relationships between the variables, were calculated using ANOVA table. The significance of all terms in the polynomial was assessed statistically by computing the F value at the probability p < 0.001. The PDI values ranged between 0.186 and 0.506, indicating broad size distributions [34]. A PDI value around 0.1 represents monodispersity and values near to 1 indicate polydispersity [35]. Additionally, the particle size of the MTC-loaded liposomes was small, with a MPS of all formulations ranging between 92.16 and 127.5 nm, consistently smaller than 128 nm. Encapsulation efficiency of MTC in liposomes ranged from 71 to 94%. The best results were achieved when 1.97% of SPC, 0.08% of cholesterol, 97.84% of chloroform, and 0.1% of MTC were used for the preparation of liposomes. Furthermore, ZP values were consistently negative for all formulations, ranging from −30.5 to −55.3. As is well-known, nanocarriers with negative surface charges may impact the processes involved in their transport from the nasal cavity [36]. Negatively charged nanocarriers can penetrate mucus more effectively without any interaction [37].
The procedure was optimized individually for each of the three responses by creating simplified model polynomial equations that establish the connections between the dependent and independent variables (Table III). The best formulation was selected based on the criteria of achieving the smallest particle size and PDI value and with significant encapsulation efficiency and ZP. The final ideal experimental parameters were determined by utilizing the extensive grid search and feasibility search features provided by the Design Expert program. Numerical optimization of the amounts of wall materials was performed using the desirability function. The optimization parameters are presented in Table III.
Experimental and predicted values did not differ significantly (p > 0.05). A total of 1.98% SPC, 0.081% cholesterol, 97.84% chloroform, and 0.1% MTC were found to be the optimal composition of MTC-loaded liposomes.
Liposomal Morphology
SEM is the most convenient visual technique for investigating the mean size and surface morphology of prepared nano-formulations [38]. The surface morphology of the optimal liposome formulation was assessed through SEM analysis. SEM images were captured to gather more information about the morphology of the prepared API-Lip (Fig. 2). In Fig. 2, it can be observed that the particles were nearly spherical, uniform in size, with smooth surfaces. The SEM images obtained support the results of the nano-sized measurements.
In Situ Gel with Gellan Gum Preparation
As mentioned in the method section, the determination of gellan gum concentration primarily depended on the thickness of the gel formed by mixing different concentrations of gellan gum (0.4%, 0.5%, 0.6%, and 0.7%) with a simulated nasal fluid solution. Samples containing gellan gum up to 0.5% w/w did not exhibit any signs of the sol-gel transition upon contact with the simulated nasal fluid solution. This could be attributed to the low concentration of gellan gum and insufficient ionic interactions with the simulated nasal fluid solution. Consequently, these formulations were not used for further study. However, formulations containing 0.6% and 0.7% w/w gellan gum displayed immediate gelation after the addition of simulated nasal fluid solution, attributed to the aggregation of double-helical segments via complexation with cations. The most favorable gel appearance was achieved with a concentration of 0.6% gellan gum. These results align well with findings from other researchers [39].
MTC-ISG Preparation and Characterization
Liposomal and non-liposomal MTC-loaded in situ gel formulations, as well as blank liposomal formulations, were prepared according to the ratios specified in Table IV. Three formulations were created. For the non-liposomal in situ gel formulations, the gelling agent was first prepared, and then the specified amount of MTC (0.1% v/w) was dissolved in the appropriate amount of destil water and added to the formulation. Regarding the liposomal in situ gel formulations, liposomes were initially prepared using SPC and MTC at the specified ratios, employing the thin-film hydration method. Subsequently, the in situ gel (gellan gum) was prepared. The liposomes were then incorporated into the gels, and the mixture was stirred at 500 rpm at room temperature (25± 0.5°C) for 30 min using the direct incorporation method.
Mechanical Properties
In general, nasal in situ gel compositions should possess appropriate mechanical properties for easy administration and high mucosal spreadability [40]. To gain a better understanding of the gel structure and evaluate how well the formulations resist compressive loads and subsequent relaxation, texture profile analyses (TPA) were conducted. Hardness, compressibility, adhesiveness, and cohesiveness were used to characterize the mechanical properties of the formulations (Table V).
A formulation’s hardness and compressibility determine how much force is required to remove it from the container. This attribute measures the amount of deformation that occurs when the sample is compressed. It is desirable to have a gel with a low hardness and compressibility in order to make it easier to remove it from the container [41]. There are numerous challenges to be overcome when developing intranasal formulations, including improved spreadability, mucoadhesion, and acceptable viscosity, all of which contribute to the ease of administration and compliance of patients. The TPA is a method of assessing the mechanical properties of semi-solid formulations by examining the physical structure of the gel [24]. Table V presents the mechanical parameters derived from the force-time curves obtained from TPA diagrams, including density exponent, adhesiveness, cohesiveness, and viscosity. The sample hardness varied between 0.481 ± 0.020 and 0.581 ± 0.033 N. According to the results, the statistically increased hardness was conducted in the GG formulation and lowest in Lip-GG formulations. Taking into account the textural profile analysis, an increase in adhesiveness could be attributed to an increase in viscosity of liposomal in situ gels over Blip-GG and MTC-GG gels. These results can be explained by the disruption of hydrogen bonds formed between the hydrophilic polymer chains and the solvent. Consequently, this mechanism leads to an increase in the hydrophobic polymer chains, promoting micellar aggregation and, as a result, facilitating polymer gelation [42].
It is important that the compressibility, which determines the easy removal of the gel from the container, should be low, just like the hardness value. Moreover, after phase transition at body temperature, it is desirable for in situ gel to form a homogeneous layer on the nasal respiratory mucosa surface to avoid patient discomfort and leak of the drug while facilitating drug diffusion. The compressibility of the samples varied between 1.999 ± 0.174 and 2.286 ± 0.193 N.mm. According to the results, it was no significant differences between the samples, the highest compressibility was found out in GG formulation and the lowest in Lip-GG formulation.
A greater adhesiveness value may result in increased adhesion to mucosal surfaces and a longer retention time, thereby ensuring better clinical effectiveness. A lower cohesiveness value indicates better spreadability [23]. The samples adhesiveness varied between 1.003 ± 0.095 and 4.498 ± 0.429 N.mm. Taking into account the textural profile analysis, an increase in adhesiveness could be attributed to an increase in viscosity of liposomal in situ gels over Blip-GG and MTC-GG gels. These results can be explained by the disruption of hydrogen bonds formed between the hydrophilic polymer chains and the solvent. Consequently, this mechanism leads to an increase in the hydrophobic polymer chains, promoting micellar aggregation and, as a result, facilitating polymer gelation [43].
Spreadability
The spreadability test is very important for production of in situ gel systems because it shows the quality of the formulation. The MTC gelling system should have suitable spreadability so that it can be spread on nasal mucosal membrane easily without loss of the formulation after the administration [44]. The results of spreadability were shown in Table VI. The spreadability results ranged between 71.27 ± 0.39 to 86.39 ± 0.25 g/s. The results showed that spreadability results did not correlated with the viscosity values, because it was no significant differences between the formulations in terms of viscosity results (p > 0.05).
pH and Viscosity
The pH of the prepared in situ gel formulation is between 5.9 and 6.4 and this result proves that the application can be made without causing any nasal mucosal damage (Table VI) [45].
In situ gels should have an optimal viscosity that allows for easy application of the formulations. Initially, they should be easy to spray as a liquid and then undergo a rapid gelation process due to ionic interactions. The viscosity of the formulations ranged between 17.01 ± 0.02 and 17.83 ± 0.01 cP (Table VIII). The highest viscosity range is achieved when MTC is loaded into the liposomal formulation and incorporated into the gellan gum in situ gel (Lip-GG). The obtained results could be explained by gellan gum and liposomal formulations having a tendency to form hydrogen bonds and, accordingly, forming interpolymer connections [46]. It was found that the MTC containing formulations showed increased viscosity values (p > 0.05). Also incorporation of liposomal dispersion into the in situ gel formulations (Blip-GG) did not cause any significant change in viscosity measurements.
FTIR-ATR Analysis
Figure 3 shows the FTIR analysis of MTC and the formulations. In the FTIR spectra of pure MTC, the following peaks were observed: 3394.39 cm−1 (OH stretching mode of hydrate), 3302.81 cm−1 (symmetric NH2 stretching vibration), 3192 and 2942.51 cm−1 (NH stretching mode of amide), 1661.41 cm−1 (OH bending mode of hydrate), 1629.09 cm−1 (NH2 scissoring and/or C=O stretching bands), and 1537.61 cm−1 (amide N–H band) (Fig. 3). These findings were found to be in agreement with the reference article [47]. The major OH group signal at 3394 cm−1 and 3192 cm−1 is prominent, which belongs to gellan gum. In addition, stretching vibrations belonging to the aromatic C-O group are seen in the spectrum at 2943.57 and 2635.90 cm−1. The signal at 1628.54 cm−1 is due to the glycosidic link in gellan gum, which is also prominent. Again, these results appear to be in agreement with the reference study [48].
In the spectrum of MTC-GG, it is observed that the stretching vibrations of the -OH group shift to 3327.61 cm−1 due to the -NH2 group of MTC. Additionally, the stretching vibrations originating from the glycosidic bonds of gellan gum and the C=O vibrations of MTC combine to produce a single peak at 1636.19 cm−1. The spectrum resulting from the -OH stretching vibrations of gellan gum in the placebo formulation, arising from the -CH2 group of SPC, appears as a single spectrum at 3331.82 cm−1. Furthermore, the C=O band of the cholesterol content in the liposome gives a signal at 1636.09 cm−1 [49]. This confirms the incorporation of liposomes into gellan gum. In the MTC-loaded liposome formulation, the peaks of MTC were not clearly observed, which indicates that most of the MTC is entrapped within the liposomal formulation. Additionally, vibrations of glycosidic bonds originating from gellan gum are observed at 1636.06 cm−1, and stretching vibrations of -PO2 originating from soy lecithin are seen at 637.09 cm−1.
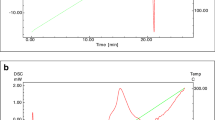
DSC Analysis
Figure 4 displays the DSC thermograms of MTC and formulations using a heating rate of 10°C/min from 25 to 300°C. It clearly indicates a single endothermic peak at 112.5°C in the DSC curve of MTC [47, 50]. In addition to observing a single endothermic peak in the thermogram of gellan gum (GG), the onset temperature is noted at 94.5°C, while the peak melting temperature is observed at 142.3°C. This is believed to occur because the bonds between glyceryl and acetyl groups located outside the molecule begin to break [51]. In the thermograms of gellan gum-blank liposome (Blip-GG) and gellan gum-MTC-loaded liposomes (Lip-GG) formulations, the onset temperatures of the endothermic peaks are 93.8°C and 94.1°C, respectively, and melting temperatures were observed as 128.3°C and 131.8°C. The increase in the melting point in the Blip-GG formulation is thought to be due to the increased cross-linking of gellan gum, requiring more energy [18]. The temperature increase in the Lip-GG formulation is attributed to the endothermic energy requirement resulting from both GG and MTC content. In the MTC-GG formulation, the melting point of MTC is characterized by a single endothermic peak at 135.3°C due to gellan gum [52].
Storage Stability Studies of Liposomal Formulations
The stability of MTC-loaded liposomes and Lip-GG formulation and Lip-GG formulation after passage through a device that stimulates nasal administration was monitored over a period of 5 weeks. The samples were stored in sealed containers at 4 ± 0.5°C and 65% relative humidity (Table VII). At predetermined intervals, aliquots were taken and measured for MPS, PDI, ZP, and EE. ZP values ranged from −47.3 ± 0.07 to −51.6 ± 0.08, while MPS showed variations between 107.3 ± 0.17 nm and 111.1 ± 0.28 for MPS, the values ranged from 0.181 ± 0.02 to 0.193 ± 0.03. The last response, which is the EE of MTC, varied between 78.61 ± 0.14% and 84.75 ± 0.81%, showing no significant difference in the resulting ratios (p ≥ 0.05) [53]. Furthermore, the slight loss in EE of MTC could be attributed to MTC’s high water-solubility, as continuous partitioning of MTC into the aqueous core might have led to hydrolytic degradation. A similar trend has been reported for allicin-loaded liposomes, where encapsulation efficiency decreased over the course of 50 days of storage at 4°C [54].
HPLC Method
Several validation studies have been conducted for MTC in order to develop the analytical method. Based on the guidelines contained in ICH Q2 (R1), the HPLC method was validated [55]. The LOD and LOQ were determined as 0.004 µg/mL and 0.009 µg/mL, respectively, indicating the method’s sensitivity. The method exhibited good linearity over the tested concentration range (0.011–30 µg/mL) with an R2 value exceeding 0.99 for the MTC standard. Based on the observed data, it can be concluded that the method is reliable for identifying and quantifying MTC in formulations, in accordance with ICH guidelines.
In Vitro Release Study
A Franz diffusion cell was used to investigate the in vitro release behavior of MTC-GG and Lip-GG formulations. A cellulose dialysis membrane served as the diffusional barrier, and Krebs buffer solution (pH, 6.6) served as the receptor medium. Based on the formulations, Fig. 5 displays the release profiles. Lip-GG formulations produced cumulative drug release exceeding 95% after 5 h. Additionally, Lip-GG displayed a significantly improved in vitro release profile as compared to MTC-GG control samples. It is thought that the controlled release effect and increased permeation of the drug-facilitated by the liposome accounts for the enhanced permeation and sustained release effect of MTC from the Lip-GG formulation [56]. Drug release from liposomes depends on the lipophilicity of drug molecule and lipid composition other than the type of liposomes. It was reported that multilamellar vesicles have shown barrier property for the release of encapsulated water soluble drug (Betageri, G.V. and Parsons, D.L., 1992. Drug encapsulation and release from multilamellar and unilamellar liposomes. International journal of pharmaceutics, 81(2-3), pp.235-241.). Drug release from multilamellar vesicles have two main points of interests. First, phospholipid bilayers may simulate some fundamental properties of biological membranes and constitute a model system to investigate passive drug transport. Second, there is a possibility of application of these systems for sustained or controlled drug delivery application, mainly for non-parenteral route of administration [57]. Furthermore, cholesterol’s amphiphilic properties promote hydrogen bonding, further increasing MTC solubility within the liposomal core, which might enhance drug absorption [56]. Additionally, it was observed that the MTC-GG formulation released less active ingredient than the MTC-GG formulation. There might be an inflection point in the release profiles, indicating the formation of gel in the donor compartment of the diffusion cell, which could explain these results. Due to polymer cross-linking and increased viscosity, which hinder molecule movement, a portion of the drug may become entrapped within the gel matrix during gel formation [58].
A regression coefficient value comparison of different kinetic models determined that the R2 value of Lip-GG formulation and release data correlated most closely with the Korsmeyer-Peppas model (R2, 0.973; n, 0.93), while the Higuchi kinetics model was used to determine the release of the active substance in GG-MTC gel formulation. Korsmeyer-Peppas is a comprehensive model for depicting drug release from polymeric systems, because the model identifies the main transport phenomena, either diffusion or swelling, involved in the release [59]. A release exponent (n) greater than 1 indicates a non-Fickian diffusion release pattern from liposomal in situ gel, in which matrix diffusion, erosion, and polymer chain loosening play a significant role in drug release [60, 61]. The release of drugs may be affected by a variety of processes, such as diffusion, erosion, and loosening of polymer chains. As a result of swelling and erosion, the polymer exhibits the characteristic hydrophilic characteristics of the polysaccharide gelling agent (gellan gum), leading to Case II transport. This is an unusual release model that results from the expansion of forces (van der Waals and dipole-dipole interactions) caused by the swollen gel within the vitreous nucleus [62].
XTT Cytotoxicity Assay
After 24 h, the viability of cells treated with 0.5 mM Lip-GG, MTC-GG, and the control was 97.1% ± 1.8%, 83.1% ± 2.4%, and 78.7% ± 1.9%, respectively. Additionally, when 2 mM MTC formulations were applied to the cells, the viability was determined as 95.5% ± 1.5%, 69.7% ± 2.23%, and 61.3% ± 2.2% for Lip-GG, MTC-GG, and control groups (Figs. 6 and 7).
The Lip-GG group showed the highest rate of cell viability, and there was no significant difference observed between the untreated and Lip-GG group even 24 h later (p > 0.05). Subsequently, at 48 h, the viability of cells treated with 0.5 mM Lip-GG, MTC-GG, and the control was determined to be 96.3% ± 1.3%, 79.4% ± 2.2%, and 62.1% ± 0.5%. For the 2 mM concentration, it was 93.6% ± 3.2%, 61.1% ± 1.7%, and 55.6% ± 1.5%, respectively (Figs. 6 and 7).
It was found that the Lip-GG formulation resulted in significantly higher cell rejuvenation compared to the MTC-GG and control groups, for both treatment intervals of 24 h and 48 h (p < 0.005). The study by Radhakrishnan et al. mentioned that MTC is a natural D2 receptor antagonist, a 5-HT3 and 5-HT4 receptor agonist known for its cancer chemopreventive activity, and it induces apoptosis in breast cancer cells as well [63]. In the same study, Mogharbel et al. reported that MT, another apoptosis regulatory protein, p53, induced the expression of one of the apoptosis-stimulating protein families (ASPP) [64].
In Vivo Study
Humans and rabbits are both dealkylated to monodiethylclopramide after nasal administration of MTC [65]. The Cmax values obtained from the gellan gum-prepared solution formulations (Fig. 8 and Table VIII) differed significantly (p < 0.05; p < 0.001). It is statistically significant that the tmax value of the formulation achieved with the liposomal system differs from that of the IV and MTC-GG formulations (p < 0.05). The liposomal system is thought to play a significant role in this as it retains the active substance for a longer period of time and releases it at a controlled rate [66]. Again, the same reason, the fact that the elimination constant (kel), is statistically higher than in the IV and MTC-GG formulations (p < 0.05), is thought to depend on the effect of the liposomal transporter system on controlled drug release [67]. In light of the findings obtained, it was determined that the Lip-GG formulation exhibited a faster and better absorption profile, leading to higher bioavailability compared to MTC-GG (Fabs) (p < 0.05) (Table 9). It was also observed that the Lip-GG formulation showed a sustained absorption profile, which can be explained by the vesicular structure of liposomes releasing the active substance slowly and continuously, providing plasma concentration for a long time, and therefore showed higher bioavailability. This finding is supported by the calculated AUC value. It was also found that Lip-GG and IV MTC formulation had a statistically higher AUC value compared to MTC-GG. The enhanced drug permeation across nasal mucosa could be explained based on the liposomes’ lipophilic nature and nanosize, which facilitate the passage of MTC across the nasal mucosal epithelium, resulting in efficient delivery into the bloodstream [68, 69] (Table 9).
Conclusion
We aimed to evaluate the efficacy of a novel intranasal composite formulation that incorporates liposomes into in situ gels in an attempt to uncover its numerous benefits. The formulation was designed to enhance the delivery of drugs to the nasal cavity and provide ease of administration, precise dosing, prolonged retention in the nasal cavity, and enhanced absorption of the drug by improving the delivery of drugs to the nasal cavity. Researchers need to determine whether this formulation can improve the effectiveness and efficiency of drug delivery for various intranasal applications by enhancing the effectiveness and efficiency of drug delivery. In light of the available evidence, it seems as if delivering hydrophilic antiemetic molecules through the nasal passage would be a viable and advantageous option compared to the traditional routes of delivering them orally or via parenteral routes. In addition to making patients more comfortable and providing them with more effective relief from nausea and vomiting, this type of approach may prove to be more convenient for the patients as well. There is a great deal of potential benefit for the pharmaceutical industry if this approach is implemented in the future; therefore, it is of paramount importance that the industry explore this option.
Data Availability
The data will be present according to request.
References
Sharma M, Sharma R, Jain DK. Nanotechnology based approaches for enhancing oral bioavailability of poorly water soluble antihypertensive drugs. Scientifica. 2016;2016:1–11.
Bozzuto G, Molinari A. Liposomes as nanomedical devices. Int J nanimed. 2015;10:975–99.
Akbarzadeh A, Rezaei-Sadabady R, Davaran S, Joo SW, Zarghami N, Hanifehpour Y, et al. Liposome: classification, preparation, and applications. Nanoscale Res Lett. 2013;8:1–9.
Hofheinz R-D, Gnad-Vogt SU, Beyer U, Hochhaus A. Liposomal encapsulated anti-cancer drugs. 2005;16(7):691-707.
Gavini E, Hegge AB, Rassu G, Sanna V, Testa C, Pirisino G, et al. Nasal administration of carbamazepine using chitosan microspheres: in vitro/in vivo studies. 2006;307(1):9-15.
Mara MR, Cristina CUM, Oliveira CP, Vinicius CM, Cesar ER, Palmira D, Gremiao M. Liposomes and micro/nanoparticles as colloidal carriers for nasal drug delivery. Curr Drug Deliv. 2006;3(3):275–85.
Lansley AB. Mucociliary clearance and drug delivery via the respiratory tract. Adv Drug Del Rev. 1993;11(3):299–327.
Rossi S, Vigani B, Sandri G, Bonferoni MC, Caramella CM, Ferrari F. Recent advances in the mucus-interacting approach for vaginal drug delivery: from mucoadhesive to mucus-penetrating nanoparticles. 2019;16(8):777-81.
Vigani B, Rossi S, Sandri G, Bonferoni MC, Caramella CM, Ferrari FJP. Recent advances in the development of in situ gelling drug delivery systems for non-parenteral administration routes. Pharmaceutics. 2020;12(9):859.
Esim O, Savaser A, Ozkan CK, Oztuna A, Goksel BA, Ozler M, et al. Nose to brain delivery of eletriptan hydrobromide nanoparticles: preparation, in vitro/in vivo evaluation and effect on trigeminal activation. J Drug Del Sci Technol. 2020;59:101919.
Pires A, Fortuna A, Alves G, Falcão A, Sciences P. Intranasal drug delivery: how, why and what for? J Pharm Pharm Sci. 2009;12(3):288–311.
Fortuna A, Alves G, Serralheiro A, Sousa J, Falcão A. Intranasal delivery of systemic-acting drugs: small-molecules and biomacromolecules. Eur J Pharm Biopharm. 2014;88(1):8–27.
Karavasili C, Fatouros DGJDdt. Smart materials: in situ gel-forming systems for nasal delivery. 2016;21(1):157-66.
Cao S-l, Ren X-W, Zhang Q-Z, Chen E, Xu F, Chen J, et al. In situ gel based on gellan gum as new carrier for nasal administration of mometasone furoate. Int J Pharm. 2009;365(1–2):109–15.
Coviello T, Matricardi P, Marianecci C, Alhaique F. Polysaccharide hydrogels for modified release formulations. J Contr Rel. 2007;119(1):5–24.
Hibberd CJ, Chassaing E, Liu W, Mitzi DB, Lincot D, Tiwari AN, et al. Non‐vacuum methods for formation of Cu (In, Ga)(Se, S) 2 thin film photovoltaic absorbers. 2010;18(6):434-52.
Adnet T, Groo A-C, Picard C, Davis A, Corvaisier S, Since M, et al. Pharmacotechnical development of a nasal drug delivery composite nanosystem intended for Alzheimer’s disease treatment. Pharmaceutics. 2020;12(3):251.
Yu S, Wang Q-M, Wang X, Liu D, Zhang W, Ye T, et al. Liposome incorporated ion sensitive in situ gels for opthalmic delivery of timolol maleate. Int J Pharm. 2015;480(1–2):128–36.
Rana K, Sharma PJ, Technology. Analytical method development and validation for the simultaneous estimation of metformin hydrochloride and alogliptin by RP-HPLC in bulk and tablet dosage forms. 2021;13(2):111-8.
Ockun MA, Baranauskaite J, Uner B, Kan Y, Kırmızıbekmez H. Preparation, characterization and evaluation of liposomal-freeze dried anthocyanin-enriched Vaccinium arctostaphylos L. fruit extract incorporated into fast dissolving oral films. J Drug Del Sci Technol. 2022;72:103428. https://doi.org/10.1016/j.jddst.2022.103428.
Sebaaly C, Jraij A, Fessi H, Charcosset C, Greige-Gerges H. Preparation and characterization of clove essential oil-loaded liposomes. Food Chem. 2015;178:52–62.
Baranauskaite J, Duman G, Corapcıoğlu G, Baranauskas A, Taralp A, Ivanauskas L, et al. Liposomal incorporation to improve dissolution and stability of rosmarinic acid and carvacrol extracted from oregano (O. onites L.). Biomed Res. 2018;2018:1–10.
Baloglu E, Karavana SY, Senyigit ZA, Hilmioglu-Polat S, Metin DY, Zekioglu O, et al. In-situ gel formulations of econazole nitrate: preparation and in-vitro and in-vivo evaluation. J Pharm Pharmacol. 2011;63(10):1274–82.
Jones DS, Bruschi ML, de Freitas O, Gremião MPD, Lara EHG, Andrews GP. Rheological, mechanical and mucoadhesive properties of thermoresponsive, bioadhesive binary mixtures composed of poloxamer 407 and carbopol 974P designed as platforms for implantable drug delivery systems for use in the oral cavity. Int J Pharm. 2009;372(1–2):49–58.
Okur NÜ, Yozgatli V, Okur ME. In vitro–in vivo evaluation of tetrahydrozoline-loaded ocular in situ gels on rabbits for allergic conjunctivitis management. Drug Dev. 2020;81(6):716–27.
Sherafudeen SP, Vasantha P. Development and evaluation of in situ nasal gel formulations of loratadine. Res Pharm Sci. 2015;10(6):466.
Sakeena MHF, Muthanna FA, Ghassan ZA, Kanakal MM. Formulation and in vitro evaluation of ketoprofen in palm oil esters nanoemulsion for topical delivery. J Oleo Sci. 2010;59(4):223–8.
Ng S-F, Rouse J, Sanderson D, Eccleston GJP. A comparative study of transmembrane diffusion and permeation of ibuprofen across synthetic membranes using Franz diffusion cells. Pharmaceutics. 2010;2(2):209–23.
Gunes Ozunal Z, Donmez Y, Tekin S, Saglam E, Aktas RG. Metoclopramide increased cell proliferation in HepG2 cell line and sorafenib attenuated the effect. Ann Med Res. 2020;27(4):1188–92.
Jost L, Kirkwood J, Whiteside T. Improved short-and long-term XTT-based colorimetric cellular cytotoxicity assay for melanoma and other tumor cells. Comp Stud. 1992;147(2):153–65.
Bayrak Z, Kurbanoglu S, Savaser A, Ozkan SA, Altunay H, Tas C, et al. LC–MS method for the sensitive determination of metoclopramide: application to rabbit plasma, gel formulations and pharmaceuticals. Chromatographia. 2014;77:99–107.
Ullah F, Iqbal Z, Raza A, Khan I, Ullah Khan F, Hassan M, et al. Simultaneous determination of methotrexate and metoclopramide in physiological fluids using RP-HPLC with ultra-violet detection; application in evaluation of polymeric nanoparticles. J Liq Chromatogr Relat Technol. 2017;40(20):1020–30.
Sebaaly C, Charcosset C, Stainmesse S, Fessi H, Greige-Gerges H. Clove essential oil-in-cyclodextrin-in-liposomes in the aqueous and lyophilized states: from laboratory to large scale using a membrane contactor. Carbohydr Poly. 2016;138:75–85.
Mahajan HS, Tatiya BV, Nerkar PP. Retracted: ondansetron loaded pectin based microspheres for nasal administration: in vitro and in vivo studies. Elsevier; 2012.
Vergara D, Shene C. Encapsulation of lactoferrin into rapeseed phospholipids based liposomes: optimization and physicochemical characterization. J Food Eng. 2019;262:29–38. https://doi.org/10.1016/j.jfoodeng.2019.05.012.
Bonaccorso A, Musumeci T, Serapide M, Pellitteri R, Uchegbu I, Puglisi GJC, et al. Nose to brain delivery in rats: effect of surface charge of rhodamine B labeled nanocarriers on brain subregion localization. Colloids Surf B Biointerfaces. 2017;154:297–306.
Pangua C, Reboredo C, Campión R, Gracia JM, Martínez-López AL, Irache JM. Mucus-penetrating nanocarriers. Theory and Applications of Nonparenteral Nanomedicines: Elsevier; 2021. p. 137–52.
Ekelund K, Östh K, Påhlstorp C, Björk E, Ulvenlund S, Johansson F. Correlation between epithelial toxicity and surfactant structure as derived from the effects of polyethyleneoxide surfactants on caco-2 cell monolayers and pig nasal mucosa. J Pharm Sci. 2005;94(4):730–44.
Mohan EC, Kandukuri JM, Allenki VJJPR.Preparation and evaluation of in-situ-gels for ocular drug delivery. 2009;2(6):1089-94.
Baloglu E, Karavana SY, Senyigit ZA, Guneri T. Rheological and mechanical properties of poloxamer mixtures as a mucoadhesive gel base. Pharm Dev Technol. 2011;16(6):627–36.
Hao J, Zhao J, Zhang S, Tong T, Zhuang Q, Jin K, et al. Fabrication of an ionic-sensitive in situ gel loaded with resveratrol nanosuspensions intended for direct nose-to-brain delivery. Colloids Surf B Biointerfaces. 2016;147:376–86.
Almeida H, Helena AM, Lobão P, Manuel SLJ. Influence of drug incorporation, temperature and storage time on the pH, textural and rheological properties of different poloxamer hydrogels. Curr Drug Deliv. 2013;10(6):753–64.
He Y, Hassanpour A, Bayly AE. Combined effect of particle size and surface cohesiveness on powder spreadability for additive manufacturing. Powder Tech. 2021;392:191–203.
Galgatte UC, Chaudhari P. Development of metoclopramide hydrochloride in situ gel: nasal delivery and pharmacokinetics in New Zealand rabbits. 2019;12(4):280-5.
Baranauskaite-Ortasöz J, Üner B. Preparation and characterization studies of nanofiber and orodispersable film formulations of enoxolone. 2022;26(5).
Shah V, Sharma M, Pandya R, Parikh RK, Bharatiya B, Shukla A, et al. Quality by design approach for an in situ gelling microemulsion of Lorazepam via intranasal route. Mater Sci Eng C Mater Biol Appl. 2017;75:1231–41.
Wang S-L, Wong Y-C, Cheng W-T, Lin S-Y. 2011 A continuous process for solid-state dehydration, amorphization and recrystallization of metoclopramide HCL monohydrate studied by simultaneous DSC-FTIR microspectroscopy. J Therm Anal Calorimet. 2011;104(1):261–4.
Sudhamani S, Prasad M, Sankar KU. DSC and FTIR studies on gellan and polyvinyl alcohol (PVA) blend films. Food Hydrocolloids. 2003;17(3):245–50.
Kuligowski J, Quintás G, Esteve-Turrillas F, Garrigues S, Dela GM. On-line gel permeation chromatography–attenuated total reflectance–Fourier transform infrared determination of lecithin and soybean oil in dietary supplements. J Chromatograph. 2008;1185(1):71–7.
Mitchell AG. Polymorphism in metoclopramide hydrochloride and metoclopramide. J Pharm Pharmacol. 1985;37(9):601–4.
Fukada H, Takahashi K, Kitamura S, Yuguchi Y, Urakawa H, Kajiwara KJJota, et al. Thermodynamics and structural aspect of the gelling process in the gellan gum/metal salt aqueous solutions. 2002;70:797-806.
Shiyani B, Dholakiya R, Akbari B, Lodhiya D, Ramani GJJOPR. Development and evaluation of novel immediate release tablets of metoclopramide HCl by direct compression using treated gellan gum as a disintegration-accelerating agent. 2009;2(9):1460-4.
Tai K, Rappolt M, Mao L, Gao Y, Yuan F. Stability and release performance of curcumin-loaded liposomes with varying content of hydrogenated phospholipids. Food Chem. 2020;326:126973.
Hasan M, Belhaj N, Benachour H, Barberi-Heyob M, Kahn C, Jabbari E, et al. Liposome encapsulation of curcumin: physico-chemical characterizations and effects on MCF7 cancer cell proliferation. Int J Pharm. 2014;461(1–2):519–28.
Khater A-J, Mahmood S, Arifin MAB, Abdul-Halim N, Almurisi S, Technology. Development and validation of HPLC method for determination of benidipine hydrochloride in lipid vesicles formulations. 2022;9(2):40-7.
Mohammed A, Weston N, Coombes A, Fitzgerald M, Perrie Y. Liposome formulation of poorly water soluble drugs: optimisation of drug loading and ESEM analysis of stability. Int J Pharm. 2004;285(1–2):23–34.
Agnihotri SA, Soppimath KS, Betageri GV. Controlled release application of multilamellar vesicles: a novel drug delivery approach. Drug Deliv. 2010;17(2):92–101. https://doi.org/10.3109/10717540903509027.
Garhy DM, Ismail S, Ibrahim HK, Ghorab MM. Technology. Buccoadhesive gel of carvedilol nanoparticles for enhanced dissolution and bioavailability. J Drug Del Sci Technol. 2018;47:151–8.
Dash S, Murthy PN, Nath L, Chowdhury PJ. Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol Pharm. 2010;67(3):217–23.
Tolvanen E. Ruuviekstruusioon perustuvan 3D-tulostustyökalun soveltuvuus polymeeripohjaiseen lääkeformulaatioon. 2021.
Rothstein SN, Federspiel WJ, Little SR. A unified mathematical model for the prediction of controlled release from surface and bulk eroding polymer matrices. Biomaterials. 2009;30(8):1657–64.
Lao LL, Venkatraman SS, Peppas NA. Biopharmaceutics Modeling of drug release from biodegradable polymer blends. Eur J Pharm Biopharm. 2008;70(3):796–803.
Radhakrishnan V, Pai V, Rajaraman S, Mehra N, Ganesan T, Dhanushkodi M, et al. Olanzapine versus metoclopramide for the treatment of breakthrough chemotherapy–induced vomiting in children: an open-label, randomized phase 3 trial. Pediatr Blood Cancer. 2020;67(9):e28532.
Mogharbel BF, Cardoso MA, Irioda AC, Stricker PEF, Slompo RC, Appel JM, et al. Biodegradable nanoparticles loaded with levodopa and curcumin for treatment of Parkinson’s disease. Molecules. 2022;27(9):2811.
Desta Z, Wu G, Morocho A, Flockhart DA. The gastroprokinetic and antiemetic drug metoclopramide is a substrate and inhibitor of cytochrome P450 2D6. Drug Metab Dispos. 2002;30(3):336–43.
Imam SS, Aqil M, Akhtar M, Sultana Y, Ali A. Formulation by design-based proniosome for accentuated transdermal delivery of risperidone: in vitro characterization and in vivo pharmacokinetic study. Drug Del. 2015;22(8):1059–70.
Labana S, Pandey R, Sharma S, Khuller G. Chemotherapeutic activity against murine tuberculosis of once weekly administered drugs (isoniazid and rifampicin) encapsulated in liposomes. Int J Antimicro Agents. 2002;20(4):301–4.
Rompicherla SKL, Arumugam K, Bojja SL, Kumar N, Rao C-P. Pharmacokinetic and pharmacodynamic evaluation of nasal liposome and nanoparticle based rivastigmine formulations in acute and chronic models of Alzheimer’s disease. Naunyn Schmiedebergs Arch Pharmacol. 2021;394(8):1737–55.
Bashyal S, Seo J-E, Keum T, Noh G, Lamichhane S, Lee SJP. Development, characterization, and ex vivo assessment of elastic liposomes for enhancing the buccal delivery of insulin. Pharmaceutics. 2021;13(4):565.
Author information
Authors and Affiliations
Contributions
Juste Baranauskaite: conceptualization, methodology, investigation, formal analysis, data curation, writing—original draft. Meryem Aydin: investigation, formal analysis, data curation. Burcu Uner: formal analysis, writing—review and editing. Cetin Tas: supervision, review and editing
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baranauskaite, J., Aydin, M., Uner, B. et al. Formulation of Metoclopramide Hydrochloride-Loaded Lipid Carriers by QbD Approach for Combating Nausea: Safety and Bioavailability Evaluation in New Zealand Rabbit. AAPS PharmSciTech 25, 73 (2024). https://doi.org/10.1208/s12249-024-02791-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-024-02791-0