Abstract
Doxorubicin (DOX) has a cytotoxic effect on many tumor cells; however, its clinical application is limited owing to its strong side effects. Although Doxil® reduces the cardiotoxicity of free DOX, it has also introduced a new dose-limiting toxicity. In a previous study, a sialic acid-cholesterol conjugate (SA-CH) was synthesized and modified onto the surface of DOX-loaded liposomes to target tumor-associated macrophages (TAMs), further improving the efficacy of DOX-loaded liposomes over that of Doxil®. Meanwhile, the good retention characteristics and promising antitumor ability of sphingomyelin/cholesterol (SM/CH) system for water-soluble drugs have attracted wide attention. Therefore, we aimed to use SA-CH as the target and hydrogenated soybean phosphatidylcholine (HSPC) or egg sphingomyelin (ESM) as the membrane material to develop a more stable DOX-loaded liposome with stronger antitumor activity. The liposomes were evaluated for particle size, polydispersity index, zeta potential, entrapment efficiency, in vitro release, long-term storage, cytotoxicity, cellular uptake, pharmacokinetics, tumor targetability, and in vivo antitumor activity. In the liposomes prepared using HSPC/CH, sialic acid (SA) modification considerably increased the accumulation of DOX-loaded liposomes in the tumor, thus exerting a better antitumor effect. However, SA modification in DOX-ESL (SA-CH-modified DOX-loaded liposomes prepared by ESM/CH) destroyed the strong retention effect of the ESM/CH system on DOX, resulting in a reduced antitumor effect. Notably, DOX-ECL (DOX-loaded liposome prepared by ESM/CH) had the optimal storage stability, lowest toxicity, and optimal antitumor effect due to better drug retention properties. Thus, the ESM/CH liposome of DOX is a potential drug delivery system.
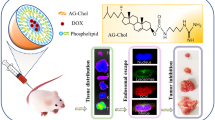
Graphical Abstract
Sketch of the effect of two DOX-loaded liposomes with hydrogenated soybean phospholipid (HSPC) and egg sphingomyelin (ESM) as lipid membrane material and surface-modified SA derivative on tumor growth inhibition.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Doxorubicin (DOX), a broad-spectrum anticancer drug, has extremely strong antitumor activity [1, 2]. However, as a cell cycle non-specific drug, it has a strong cytotoxic effect on both tumor and normal cells, which has also triggered its strong side effects. In addition to the common side effects such as bone marrow suppression, vomiting, nausea, and alopecia, it can damage myocardial cells through oxygen free radicals due to its significantly high affinity with the myocardium, thereby causing severe cardiac toxicity [3,4,5]. Liposomes have been well developed as drug delivery systems since their discovery in 1964 by Bangham et al. because of their unique advantages [6]. The encapsulation of DOX into liposomes not only increases drug accumulation in tumors but also effectively reduces its side effects, especially cardiotoxicity [7, 8].
Doxil® was the first liposomal DOX, with a lipid composition of hydrogenated soybean phosphatidylcholine (HSPC), cholesterol (CH), and mPEG2000-DSPE, approved in 1995 by Sequus Pharmaceuticals [9]. The coverage of a PEGylated layer on the surface of liposomes by “STEALTH” technology also avoids immune system recognition and phagocytosis and achieves long circulation in vivo [10, 11]. Although PEG-modified liposomes greatly reduce the cardiotoxicity of DOX, they cause skin toxicity, such as palmar-plantar erythrodysesthesia (PPE), with an incidence approaching 50% [12, 13]. Morever, Doxil® did not show significantly improved efficacy in clinical treatment [14, 15]. Therefore, DOX-loaded liposomes still need to be optimally formulated to increase stability, cycle time, and efficacy.
A previous study showed that SA-modified DOX-loaded liposomes prepared using HSPC/CH exhibited better antitumor effects in the S180 tumor-bearing mouse model than PEGylated liposomal DOX [16, 17]. Sialic acid (SA), an acidic amino sugar containing nine carbon atoms, plays an important role in many physiological and pathological processes [18]. Currently, SA binding proteins mainly include Selectin, Siglec, and factor H [19, 20]. Siglec-1 expressing tumor-associated macrophages (TAMs) affects tumor occurrence and development by promoting immunosuppression, angiogenesis, and tumor invasion and metastasis [21, 22]. Some TAMs tend to enter the hypoxic region of the tumor and deliver nano-drug carriers into the tumor tissue. Finally, the tumor is treated by specifically clearing TAMs and killing the tumor cells. In this study, we used a specific combination of SA and Siglec-1 to deliver drugs to TAMs.
Although SA-modified liposomes achieved a good antitumor effect [23, 24], the stability of this formulation needs to be further improved. Egg sphingomyelin (ESM) is a major lipid component of animal cell membranes, along with phosphatidylcholine (PC), and constitutes more than 50% of the membrane lipids. Although PC and SM have similar structures, their physicochemical properties are different [25,26,27]. Specifically, the fatty chains in the ESM and HSPC structures are linked by amide and ester bonds, respectively; therefore, ESM is less prone to acid hydration and enzymatic degradation than PC [28]. It was also pointed out that the nitrogen atom of the amide bond in the ESM structure could form an intermolecular hydrogen bond with the oxygen atom in CH, resulting in good retention characteristics and in vivo stability of water-soluble drugs [28, 29].
To the best of our knowledge, phospholipids play a crucial role in the stability of liposome preparations, and there has been no study reporting DOX-loaded liposomes prepared by ESM/CH. In this study, we prepared SA-modified DOX-loaded liposomes using HSPC/CH and ESM/CH as membrane materials to improve the stability and antitumor effect of DOX preparations.
Materials and Methods
Materials
Doxorubicin hydrochloride (DOX, purity ≥ 99%) was obtained from Beijing Huafeng United Technology Co., Ltd. (Beijing, China); hydrogenated soybean phosphatidylcholine (HSPC) was obtained from Lucas Meyer (Germany); egg sphingomyelin (ESM) was obtained from Lipoid GmbH (Ludwigshafen, Germany); cholesterol (CH) was obtained from Nanjing Xinbai Pharmaceutical Co., Ltd. (Nanjing, China); a sialic acid-cholesterol conjugate (SA-CH) was self-synthesized in the laboratory; Sephadex G50 (G50) was obtained from Shanghai YSRIBIO Industrial Co., Ltd. (Shanghai, China); 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) was obtained from Sigma-Aldrich (Saint Louis, USA); 1,1′-dioctadecyl-3,3,3′,3′-tetramethylindotricarbocyanine iodide (DiR iodide), RPMI-1640 cell culture, and Trypsin were obtained from Dalian Meilun Biotechnology Co., Ltd. (Dalian, China); FBS was obtained from Zhejiang Tianhang Biotechnology Co., Ltd. (Hangzhou, China).
Cells and Animals
Mouse S180 sarcoma cells and RAW264.7 monocyte-macrophage leukemia cells were supplied by the Cell Bank of the Chinese Academy of Sciences (Shanghai, China). Male Wistar rats (weighing 180–220 g) and male Kunming mice (weighing 18–22 g) were purchased from the Central Animal Laboratory of Shenyang Pharmaceutical University (Liaoning, China). All animal experiments were conducted in accordance with the guidelines of the Animal Welfare Committee of Shenyang Pharmaceutical University.
Preparation of DOX-loaded Liposome
Ethanol was added to a prescribed amount of liposome membrane material (HSPC/ESM, CH, a sialic acid-cholesterol conjugate (SA-CH)) and dissolved in a certain temperature water bath (HSPC/65℃, ESM/70℃). After the complete dissolution of membrane materials, ethanol was volatilized, and citrate buffer (200 mM, pH 4.0) was injected into the membrane materials at a speed of 4 mL/min. The initial product was obtained by stirring in a water bath at a certain temperature (HSPC/65℃, ESM/70℃) for 1 h. The product was treated by extrusion through polycarbonate membranes of 400 nm (5 times), 200 nm (10 times), 100 nm (10 times), and 80 nm (5 times) sequentially, thereby yielding blank liposomes with different prescriptions (phospholipid concentration of 50 mg/mL).
A phosphate solution (500 mM) was used to adjust the outer aqueous phase pH value of blank liposomes to 7.0, thus establishing a gradient of the inner and outer aqueous phase pH of blank liposomes. Then, the above pH gradient blank liposomes and DOX solution (5 mg/mL) were mixed and incubated at a certain temperature (HSPC/65℃, ESM/70℃) in a water bath with stirring for 20 min (EPI/phospholipid ratio 1/10, w/w). DOX-loaded liposomes were obtained after incubation in an ice-water bath for 5 min.
Characterization of DOX-loaded Liposome
Morphology
A slightly diluted DOX-loaded liposome preparation was dropped onto a copper grid covered with carbon film and negatively stained with 1.0% (w/v) phosphotungstic acid for 2 min. After natural drying at 23 ± 2℃, the morphology of each DOX-loaded liposome was observed and photographed using a transmission electron microscope (TEM) (JEOL JEM-2100, Japan).
Particle size, Polydispersity Index, Zeta Potential, and Entrapment Efficiency (EE%)
Particle size, polydispersity index (PDI), and zeta potential were determined at 23 ± 2℃ using a particle sizer (Nicomp-380, Particle Sizing Systems, USA). Sephadex G-50 was used to remove free DOX, and methanol was used to extract DOX from liposomes. Then, the content of DOX was measured at 480 nm using a multifunctional plate reader (Thermo Scientific, USA). We used the following formula to calculate the EE%:
where Abefore and Aafter represent the absorbance of liposomes with and without the free drug, respectively.
In Vitro Release Assay
Ammonium chloride (80 mM) and histidine salt buffer (10 mM) were selected as release media. Sodium hydroxide was also used to adjust the pH to 7.4, and 5% Glu was added to adjust for isotonicity. A dialysis bag (MW: 10 kDa) containing the DOX formulation was placed in a dissolution cup at 37℃ and stirred at a constant speed of 100 rpm/min. The dialysate was aspirated at 1 h, 2 h, 4 h, 8 h, 12 h, 24 h, and 48 h, and an equal amount of release medium was placed at the same temperature. The samples were spotted on a 96-well blackboard, and the concentration of DOX was determined using a multifunctional plate reader at λex = 482 nm and λem = 590 nm.
Long-term Storage Stability
Each DOX-loaded liposome was stored at 4 ± 2℃ with light-free. Particle size and EE% of each sample were determined at 0 month, 1 month, 2 months, and 3 months.
RAW264.7 Cell Uptake Assay
RAW264.7 cells were inoculated at a density of 6 × 105 cells/well into 6-well plates and incubated at 37℃ for 24 h. Next, the cell supernatants were replaced with DOX-S, DOX-HCL, DOX-HSL, DOX-ECL, and DOX-ESL (all at a DOX concentration of 50 μg/mL) diluted in a cell culture medium and incubated with the cells for 2 h. Meanwhile, SA pre-saturation groups, named DOX-HSL (SA) and DOX-ESL (SA), were set up. Briefly, excess SA solution was added to RAW264.7 cells to saturate the cell surface with SA receptors prior to incubation with the formulation. Finally, the cells were washed with PBS and quantified using flow cytometry (FCM) and confocal laser microscopy (CLSM).
MTT Assay
RAW264.7 and S180 cells were seeded in 96-well plates at a density of 5 × 103 cells/well. After 12 h in a CO2 incubator, the cells were incubated with different concentrations of DOX formulations (0.04 μM, 0.2 μM, 1 μM, 5 μM, 25 μM, and 125 μM) for 48 h. Subsequently, the MTT solution and the triple solution (10% SDS/5% isobutanol/12 mM HCl, w/v/v) were sequentially added to a 96-well plate. After the completion of the MTT assay, the optical density (OD) of each well was measured at a wavelength of 570 nm using a multifunctional plate reader.
In Vivo Pharmacokinetic Analysis
Male Wistar rats were randomly divided into five groups (n = 3) and then treated with DOX-S, DOX-HCL, DOX-HSL, DOX-ECL, or DOX-ESL at a dose of 5 mg/kg DOX. Subsequently, blood was sampled from the orbit at 0.0163 h, 0.087 h, 0.25 h, 0.5 h, 1 h, 2 h, 4 h, 8 h, 12 h, 24 h, and 48 h after injection, respectively, and the plasma was harvested after centrifugation at 5000 rpm for 10 min. The drug-containing supernatant was harvested after centrifugation at 3000 rpm for 5 min from a mixture consisting of 100 μL plasma and 900 μL methanol. The supernatants were transferred to 96-well plates, and the fluorescence intensity of the drug was measured at λex = 482 nm and λem = 590 nm.
Tumor Targetability
Tumor-bearing mice were randomly divided into four groups (n = 3) and injected with DiR-HCL, DiR-HSL, DiR-ECL, or DiR-ESL (DiR 1 mg/kg) via the tail vein. Mice were anesthetized at 1 h, 4 h, 8 h, 24 h, and 48 h after injection, placed under an in vivo FX Pro imaging system (Bruker, USA), and photographed (ex/em 750/790 nm). After taking photographs, the mice in each group were sacrificed. In addition, the heart, liver, spleen, lung, kidney, thymus, and tumor tissues of mice in each group were removed and similarly placed under the in vivo FX Pro imaging system for photography. The ROI live imaging software was used for the semiquantitative analysis of each tissue.
The distribution of DOX in the tumor tissues of each group was further determined. Briefly, sixty tumor-bearing mice were randomly divided into four groups with 15 mice in each group, namely DOX-HCL, DOX-HSL, DOX-ECL, and DOX-ESL groups. The mice were killed at 1 h, 4 h, 8 h, 24 h, and 48 h after administration, respectively, and their tumor tissues were dissected. Tumor tissue was homogenized, and 100 μL of the homogenate and 900 μL of the hydrochloric acid–methanol-in-water mixture were centrifuged at 12,000 rpm for 10 min to extract the drug. The supernatants were then transferred to 96-well plates, and the fluorescence intensity of the drug was measured using a multifunctional plate reader (ex/em 482/590 nm).
Biocompatibility of Drug-free Liposomes
Fifteen healthy Kunming mice were randomly divided into four groups, three in each group, namely control, HCL, HSL, ECL, and ESL. The dosage was 100 mg·lipid·kg−1. The drug was administered continuously for 7 days, and the weight changes of mice were detected.
Antitumor Assay
S180 cells were inoculated into the axilla of male Kunming mice at a density of 1 × 107 cells/mL to establish a mouse xenograft model. When the tumor volume reached approximately 100 mm3, the mice were randomly divided into six groups (n = 6). The control group was administered 10 mL/kg of 5% Glu by tail vein injection. DOX-S, DOX-HCL, DOX-HSL, DOX-ECL, and DOX-ESL were administered by tail vein injection of 5 mg/kg DOX in the other groups. Mice in each group were dosed once every three days for a total of five times during the pharmacodynamic period, and tumor volume and body weight were measured every two days. Tumor volume (V, mm3) was calculated as follows: V = 1/2 × a × b2, where a and b represent the major and minor diameters of the tumor, respectively. The tumor volume inhibition rate (TIRv) and net body weight (g) were calculated as follows: TIRV = (VControl − VTreated)/VControl × 100% and net body weight = body weight − tumor weight. In addition, in order to simultaneously consider the inhibitory effect of the preparation on tumor cells and the non-specific damage to the body, the tumor inhibition index (TIindex) was proposed by our laboratory [30]. The TIindex was calculated as follows: TIindex = body weight/tumor weight.
Histopathological Examination
At the end of the pharmacodynamic experiment, the heart, liver, spleen, lungs, kidneys, and tumor tissues of each mouse were dissected and washed with PBS. The surface water of each tissue was sucked out of the filter paper and fixed in 4% paraformaldehyde for 48 h. After a series of treatments, such as embedding, slicing, and staining, each tissue was observed and photographed under a microscope (Nikon Eclipse Ti-SR, Japan).
Immunohistochemical Staining Examination
F4/80 (a mature mouse macrophage marker) was used to mark the tumor tissue in each group as a test index for TAMs. Briefly, sections were incubated with CD68 monoclonal antibody (Santa Cruz, USA) for 12 h at 4℃ and then with HRP-labeled goat anti-rabbit antibody (Zhongshan Jinqiao, China) for 4 h at 23 ± 2℃. Hematoxylin was used to stain nuclei. Finally, the sections were observed under a microscope (Nikon Eclipse Ti-SR, Japan), and the proportion of positive cells (TAMs) was calculated using Image-Pro Plus 6.0.
Results
The characterization of liposomes composed of two different membrane materials was conducted in this study. As shown in Table I, the particle sizes of the liposomes were 100–105 nm, the PDI was < 0.1, the zeta potential was in the range of − 20 to − 15 mV, and EE% was > 95%. Liposome morphology was further characterized using TEM. As shown in Fig. 1a, each DOX-loaded liposome was round or quasi-round with a relatively uniform size. In addition, the liposome particle size observed under TEM was in accordance with the particle size measurement data from the Nicomp-380 particle size meter (approximately 100 nm).
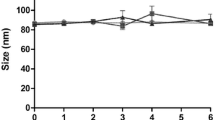
(a) The transmission electron microscopy images of a DOX-HCL, b DOX-HSL, c DOX-ECL, and d DOX-ESL. (b) In vitro cumulative release of DOX from different DOX formulations (n = 3). (c) Change of particle size a and EE% b of different DOX liposomes during a storage period of three months. Stability data were represented for initial, 1 month (1 M), 2 months (2 M), and 3 months (3 M) (n = 3) (*p < 0.05, **p < 0.01)
The release behavior of each DOX prescription is shown in Fig. 1b. DOX-S release was the fastest, with almost complete release at approximately 8 h. The four DOX-loaded liposomes exhibited a significantly lower release rate compared with DOX-S (P < 0.05), indicating that the preparation had a drug-sustained-release effect. After 48 h, the release rates of DOX-loaded liposomes were in the order: DOX-HCL ≈ DOX-HSL > DOX-ESL > DOX-ECL.
Figure 1c illustrates the changes in particle size and EE% of each liposome after three months of storage at 4 ± 2℃. The particle size of DOX-HCL and DOX-HSL increased significantly (P < 0.05), while those of DOX-ECL and DOX-ESL showed no significant change (P > 0.05). Moreover, the EE% of DOX-HCL, DOX-HSL, and DOX-ESL decreased significantly after three months (P < 0.05), whereas no significant change was observed in the EE% of DOX-ECL (P > 0.05).
As shown in Fig. 2a and Table II, each DOX preparation had a dose-dependent inhibitory effect on the growth of S180 and RAW264.7 cells. The inhibitory effect of each liposome on the cells was lower than that of DOX-S. Regardless of whether the DOX-loaded liposomes were prepared using HSPC/CH or ESM/CH, the SA modification significantly increased the inhibitory effect of drugs on the cells (P < 0.05). In addition, liposomes prepared with ESM/CH exhibited significantly weaker cell inhibition than DOX-loaded liposomes prepared with HSPC/CH (P < 0.05).
(a) Cell viability of the RAW264.7 cells a and S180 cells b incubated with different DOX formulations (n = 3). (b) The cellular uptake of different DOX formulations in RAW264.7 cells. a Flow cytometry analysis of the RAW264.7 cells treated with different DOX formulations at 37℃. b Quantitative results of flow cytometry analysis (n = 3). (c) Confocal images of the RAW264.7 cells incubated with different DOX formulations at 37℃. Note: scale bar = 50 μm (**p < 0.01)
The results of FCM (Fig. 2b) and CLSM (Fig. 2c) collectively revealed that the fluorescence intensity of each DOX prescription taken up by RAW264.7 cells was in the following order: DOX-S > DOX-HSL > DOX-HCL ≈ DOX-HSL (SA) > DOX-ESL > DOX-ECL ≈ DOX-ESL (SA). The fluorescence intensity of DOX-HSL was significantly higher than that of DOX-HCL and DOX-HSL (SA) (P < 0.01), and the fluorescence intensity of DOX-ESL was significantly higher than that of DOX-ECL and DOX-ESL (SA) (P < 0.01).
As shown in Fig. 3 and Table III, DOX-S was completely eliminated from blood circulation within 15 min, whereas DOX-loaded liposomes significantly delayed drug elimination (P < 0.05). The AUC0–48 h values of the DOX-HCL, DOX-HSL, DOX-ECL, and DOX-ESL groups were 1168-, 1232-, 2117-, and 1783-fold higher than that of the DOX-S group, respectively.
To further evaluate the biodistribution of each liposome in vivo, DiR dye was chosen as a fluorescent probe in live imaging experiments in mice (Fig. 4a,b). The fluorescence intensities of the tumors in the DiR-HCL and DiR-HSL groups reached a maximum at 8 h and then gradually decreased, showing only a weak fluorescence at 48 h. The fluorescence intensities of the tumors in the DiR-ECL and DiR-ESL groups reached a maximum of 24 h. On the other hand, the results of the DOX distribution experiment in tumor tissue further proved the different distribution behaviors of different liposomes in vivo (Fig. 4c). In addition, although the fluorescence intensity of DOX-ECL decreased at 48 h, it was significantly higher than that of DOX-loaded liposomes prepared with HSPC/CH (P < 0.05).
(a) In vivo fluorescence images of S180 tumor-bearing mice at different time points following injection of DiR-labeled liposomes. (b) Ex vivo DiR fluorescence images of tumor and major organs at 48 h. (c) Quantification of the DOX distribution in the tumor after injection of different DOX formulations (n = 3)
As shown in Fig. 5, the body weight of mice in each group showed a steady rising trend within 7 days after the administration of drug-free liposomes, and there was no significant difference with the control group, which indicated the low toxicity of drug-free liposomes.
As shown in Fig. 6a, the tumors grew rapidly in the control group mice, and each DOX formulation inhibited the tumor growth rate to some extent. The tumor volume of DOX-HSL was smaller than that of DOX-HCL in liposomes prepared with HSPC/CH (P < 0.01), and the tumor volume of mice in the DOX-ECL group was smaller than that of the DOX-ESL group (P < 0.01). To better compare the antitumor efficacy of different DOX formulations, TIRV after 30 days was calculated separately for each group of mice to quantify the antitumor efficacy of each DOX formulation. Figure 6b indicates that the inhibitory effect of each DOX formulation on S180 tumors in mice occurred in the order of DOX-ECL > DOX-ESL > DOX-HSL > DOX-HCL > DOX-S, in accordance with the results shown in Fig. 6a,c. As shown in Fig. 6d,e, the percent change in body weight and net percent change in body weight before day 24 did not significantly differ between DOX-loaded liposomes during the pharmacodynamic experiment. However, the body weight gain after 24 days was significantly higher in the ESM/CH-prepared liposomes than in the HSPC/CH-prepared liposomes. As shown in Fig. 6f, all the rats in the untreated group and the DOX-S group died on days 32 and 31 after modeling, respectively, and all the rats in the DOX-HCL group died on day 60. On day 75, the survival rates of DOX-HSL, DOX-ECL, and DOX-ESL groups were 37.5%, 75%, and 50%, respectively.
(a) Tumor growth curves of tumor-bearing mice receiving diverse DOX formulations (n = 1 ~ 6). (b) Tumor inhibition index change in tumor-bearing mice receiving diverse formulations (n = 1 ~ 6). (c) Tumor volume inhibition rate on day 30 in tumor-bearing mice receiving diverse formulations (n = 1 ~ 6). Percentage of body weight change (d) and net weight change (e) of tumor-bearing mice treated with different DOX formulations (n = 1 ~ 6) (**p < 0.01). (f) Percent survival of the tumor-bearing mice following administration of DOX formulations (n = 8)
Figure 7a depicts the pathological examination of each tissue. The heart, liver and spleen were all damaged to different extents in the DOX-S group, while DOX-HCL showed slight heart and liver injuries. No abnormalities were found in the heart, liver, spleen, lungs, or kidneys in the other preparation groups. Notably, a large number of necrotic areas were observed in the tumor tissues of the DOX-HSL, DOX-ECL, and DOX-ESL cohorts, and almost all of the tumor tissues in the DOX-ECL group were necrotic.
(a) Histopathology of heart, tumor, liver, lung, kidney, and spleen sections with hematoxylin and eosin (H&E) staining of different DOX groups. The sites where the solid arrows point represented the abnormal region. The scale bar represented 100 μm. (b) a Immunohistochemistry staining of F4/80 of different experimental groups within tumor stroma. The scale bar represents 100 μm. b The positive area of TAMs (%) in each group. The positive rate was calculated with the positive cell area/the total cell area × 100% (n = 1 ~ 6) (**p < 0.01, ***p < 0.001)
As shown in Fig. 7b, the F4/80 positive expression rates decreased after treatment with DOX in all preparation groups when compared with the control group. Specifically, the order of positive F4/80 expression in each DOX preparation group was as follows: DOX-S > DOX-HCL > DOX-HSL > DOX-ESL > DOX-ECL.
Discussion
There existed obvious intermolecular hydrogen bonds in the ESM/CH system that resulted in the close accumulation of the bilayer, which played a good role in protecting the drugs in the internal water phase and the drugs were not easy to leak [29]. There was no statistically significant difference in the release rates of DOX-HCL and DOX-HSL (P > 0.05), which suggests that SA modification in liposomes prepared by HSPC/CH did not change the in vitro release behavior of drugs in the preparations [17, 31]. However, in the liposomes prepared using ESM/CH, the cumulative drug release in the DOX-ESL group was significantly higher than that in the DOX-ECL group (P < 0.05). This finding suggests that the SA modification accelerated the release of DOX in the liposomes prepared using this membrane material [32].
As mentioned previously, the internal aqueous phase of the liposomes is citrate buffer (pH = 4), which induces liposome hydrolysis to some extent. However, ESM is less sensitive to acid and enzymatic degradation than HSPC because it is linked only by amide and ether bonds. Thus, liposomes prepared from the ESM/CH system had the lowest sensitivity to acid, but the addition of SA reduced the stability of this system [28].
To evaluate whether SA-modified DOX-loaded liposomes could effectively increase the internalization effect of TAMs on drugs, RAW264.7 cells were subjected to an uptake profile analysis as an in vitro macrophage model [17, 33]. The fluorescence intensity of DOX-S was significantly higher than that of other DOX-loaded liposome groups, indicating that free DOX could more easily enter cells via passive diffusion. In each liposome group, the SA modification significantly increased the accumulation of formulations in the cells, regardless of whether the liposomes were prepared with HSPC/CH or ESM/CH (P < 0.01). However, this increased uptake phenomenon disappeared after the SA solution pre-saturated RAW264.7 cell surface receptors (P > 0.05), which illustrates that the cellular uptake was mediated by the specific binding of SA to Siglec-1 expressed by macrophages [34]. In addition, the results showed that the uptake of DOX-loaded liposomes prepared with ESM/CH by RAW264.7 cells was significantly lower than that of liposomes prepared with HSPC/CH. This result indicates that ESM/CH system had excellent drug retention characteristics in the inner aqueous phase [28, 35].
The AUC0–48 h of DOX-HCL and DOX-HSL were not significantly different (P > 0.05), which suggests that the SA-CH modification did not alter the pharmacokinetic characteristics of the formulation prepared by HSPC/CH [17, 31]. However, DOX-ECL significantly increased the AUC0–48 h of DOX in DOX-loaded liposomes prepared by ESM/CH (P < 0.05). In addition, DOX-loaded liposomes prepared with ESM/CH had a longer circulation effect than DOX-loaded liposomes prepared with HSPC/CH. A possible reason for this is that the liposomes prepared by ESM/CH had a significantly reduced interaction with plasma proteins, thus effectively avoiding the recognition and phagocytosis of monocyte macrophages [28, 29]. Moreover, the drug retention ability of liposomes is closely related to their antitumor activity [36], which was confirmed in the “antitumor assay.”
Tumor tissues were homogenized to further verify the distribution of the formulation. Among them, the fluorescence intensity of DOX-HSL in liposomes prepared with HSPC/CH was higher than that of DOX-HCL, which indicated that DOX-HSL was able to enter tumor-recruited macrophages through Siglec receptor-mediated endocytosis and thus accumulate more in tumor tissues. The fluorescence intensity of DOX-ECL in liposomes prepared by ESM/CH was higher than that of DOX-ESL, and in general, DOX-ECL accumulated the most in tumor tissues and had the longest retention time. This can be attributed to the long cycle times of the ESM/CH system, which was disrupted by SA insertion (Fig. 4C) [37,38,39].
Next, the in vivo antitumor activity of the liposomes in each group was further determined. To take into account the level of tumor inhibition by the preparation and the non-specific damage to the body, this study combined the tumor volume and body weight. A new evaluation index “TIindex” (tumor inhibition index) was used, in which the larger the TIindex, the better the overall treatment effect [40]. The TIindex of DOX-S was similar to that of the control group, which indicated that DOX-S produce serious toxicity in the body and did not exert therapeutic effects. However, each DOX-loaded liposome presented reduced toxicity relative to free drugs and had a good tumor suppressive effect to some extent. The SA modification significantly improved the therapeutic efficacy of DOX in liposomes prepared from HSPC/CH (P < 0.01), whereas the SA modification also significantly decreased the therapeutic efficacy of DOX in liposomes prepared from ESM/CH (P < 0.01). This further verifies that the SA modification disrupted the excellent retention characteristics of the drugs in the ESM/CH system, reducing the antitumor effect. Similarly, in the experiment of mouse survival analysis, the DOX-loaded liposome group significantly prolonged the survival time of mice, among which DOX-ECL had the best effect. The modification of SA plays a positive role in HSPC/CH system and a negative role in ESM/CH system.
The ultimate goal of cancer therapy is to improve patient survival time and quality of life by reducing the systemic toxicity of chemotherapy [41]. The percent change in body weight and the percent change in net body weight of each DOX-loaded liposome were higher than those of DOX-S, indicating that each DOX-loaded liposome played a protective role in tumor-bearing mice to a certain extent, and the liposome group prepared by ESM/CH had the optimal effect. Histopathology analysis further illustrated that DOX-ECL was the most formulation for killing tumor tissues without causing damage to other tissues.
Macrophages are the most abundant inflammatory cells that infiltrate into tumors, and their content can reach more than 50% of the mass of solid tumors. Macrophages also play the most predominant role in the inflammatory response of the TME (tumor microenvironment) [42, 43]. To further test the effect of each DOX formulation on the colonization of TAMs in tumor tissue, F4/80 (a mature mouse macrophage marker) was selected as an indicator for TAMs detection. Then, immunohistochemical labeling of tumor tissues from each group was performed. Among them, in the liposome group prepared by HSPC/CH, the SA modification significantly reduced TAMs colonization in the TME (P < 0.01). This may be attributed to the fact that SA binds to Siglec-1 on the surface of TAMs to release drugs to kill TAMs. However, in the liposome group prepared with ESM/CH, the SA modification did not reduce TAMs colonization. In addition, the colonization of TAMs in the DOX-ECL group was significantly less than that in the other DOX-loaded liposome groups because of the long circulation function of the vehicle and good drug retention capacity.
Conclusions
In this study, SA-CH was modified on the DOX-loaded liposomes prepared using ESM/CH and HSPC/CH systems. Among them, DOX-HSL showed a stronger inhibitory effect on tumors than DOX-HCL, and SA enhanced tumor targeting based on TAMs. However, the modification of SA did not enhance the inhibitory effect of DOX-ESL on tumors but destroyed the stability of the ESM/CH system. Notably, DOX-ECL provides optimal tumor suppression with minimal toxicity, efficient depletion of TAMs, and inhibition of tumor growth. In conclusion, our study showed that DOX-loaded liposomes prepared using ESM/CH showed excellent stability and antitumor activity and provide a promising strategy for the development of DOX.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- DOX:
-
Doxorubicin
- TAMs:
-
Tumor-associated macrophages
- TME:
-
Tumor microenvironment
- SA-CH:
-
Sialic acid-cholesterol conjugate
- DOX-S:
-
DOX solution
- DOX-HCL:
-
DOX-loaded liposome prepared by HSPC/CH
- DOX-HSL:
-
SA-CH-modified DOX-loaded liposome prepared by HSPC/CH
- DOX-ECL:
-
DOX-loaded liposome prepared by ESM/CH
- DOX-ESL:
-
SA-CH-modified DOX-loaded liposome prepared by ESM/CH
- DiR-HCL:
-
DiR-loaded liposome prepared by HSPC/CH
- DiR-HSL:
-
SA-CH-modified DiR-loaded liposome prepared by HSPC/CH
- DiR-ECL:
-
DiR-loaded liposome prepared by ESM/CH
- DiR-ESL:
-
SA-CH-modified DiR-loaded liposome prepared by ESM/CH
References
Chen Y, Du Q, Zou Y, et al. Co-delivery of doxorubicin and epacadostat via heparin coated pH-sensitive liposomes to suppress the lung metastasis of melanoma. Int J Pharm. 2020;584: 119446.
Apetoh L, Ghiringhelli F, Tesniere A, et al. Toll-like receptor 4–dependent contribution of the immune system to anticancer chemotherapy and radiotherapy. Nat Med. 2007;13:1050–9.
Von Hoff DD, Layard MW, Basa P, et al. Risk factors for doxorubicin-induced congestive heart failure. Ann Intern Med. 1979;91:710–7.
Lefrak EA, Piťha J, Rosenheim S, Gottlieb JA. A clinicopathologic analysis of adriamycin cardiotoxicity. Cancer. 1973;32:302–14.
Singal PK, Deally CM, Weinberg LE. Subcellular effects of adriamycin in the heart: a concise review. J Mol Cell Cardiol. 1987;19:817–28.
Bangham AD, Horne RW. Negative staining of phospholipids and their structural modification by surface-active agents as observed in the electron microscope. J Mol Biol. 1964;8:660–8.
Akbarzadeh A, Rezaei-Sadabady R, Davaran S, et al. Liposome: classification, preparation, and applications. Nanoscale Res Lett. 2013;8:1–9.
Wagner A, Vorauer-Uhl K. Liposome technology for industrial purposes. J Drug Deliv. 2011;2011:591325.
Working P, Dayan A. Pharmacological-toxicological expert report CAELYXTM:(stealth® liposomal doxorubicin HCl). Hum Exp Toxicol. 1996;15:751–85.
Ranson MR, Cheeseman S, White S, Margison J. Caelyx (stealth liposomal doxorubicin) in the treatment of advanced breast cancer. Crit Rev Oncol Hematol. 2001;37:115–20.
Rastogi M, Saha RN, Alexander A, et al. Role of stealth lipids in nanomedicine-based drug carriers. Chem Phys Lipids. 2021;235: 105036.
Waterhouse DN, Tardi PG, Mayer LD, Bally MB. A comparison of liposomal formulations of doxorubicin with drug administered in free form: changing toxicity profiles. Drug Saf. 2001;24:903–20.
Gabizon A, Martin F. Polyethylene glycol-coated (pegylated) liposomal doxorubicin. Rationale for use in solid tumours. Drugs. 1997;54:15–21.
Skubitz KM. Phase II trial of pegylated-liposomal doxorubicin (Doxil™) in renal cell cancer. Invest New Drugs. 2002;20:101–4.
Maung K, O’Shaughnessy J, Overmoyer B. Pegylated liposomal doxorubicin (Doxil®) versus doxorubicin for first-line treatment of metastatic breast cancer. Clin Breast Cancer. 2002;3:183–4.
Ding J, Zhao D, Hu Y, et al. Terminating the renewal of tumor-associated macrophages: a sialic acid-based targeted delivery strategy for cancer immunotherapy. Int J Pharm. 2019;571: 118706.
Zhou S, Zhang T, Peng B, et al. Targeted delivery of epirubicin to tumor-associated macrophages by sialic acid-cholesterol conjugate modified liposomes with improved antitumor activity. Int J Pharm. 2017;523:203–16.
Schauer R, Kamerling JP. Exploration of the sialic acid world. Adv Carbohydr Chem Biochem. 2018;75:1–213.
Brown GD, Willment JA, Whitehead L. C-type lectins in immunity and homeostasis. Nat Rev Immunol. 2018;18:374–89.
Ding D, Yao Y, Zhang S, et al. C-type lectins facilitate tumor metastasis. Oncol Lett. 2017;13:13–21.
Biswas SK, Allavena P, Mantovani A. Tumor-associated macrophages: functional diversity, clinical significance, and open questions. In: Seminars in immunopathology. Springer; 2013. p. 585–600.
Grabowska J, Lopez-Venegas MA, Affandi AJ, Den Haan JM. CD169+ macrophages capture and dendritic cells instruct: the interplay of the gatekeeper and the general of the immune system. Front Immunol. 2018;9:2472.
Li C, Qiu Q, Gao X, et al. Sialic acid conjugate-modified liposomal platform modulates immunosuppressive tumor microenvironment in multiple ways for improved immune checkpoint blockade therapy. J Control Release. 2021;337:393–406.
Chen M, Wu W, Wang S, et al. Neutrophils as emerging immunotherapeutic targets: indirect treatment of tumors by regulating the tumor immune environment based on a sialic acid derivative-modified nanocomplex platform. Int J Pharm. 2022;620: 121684.
McIntosh TJ, Simon SA, Needham D, Huang CH. Structure and cohesive properties of sphingomyelin/cholesterol bilayers. Biochemistry. 1992;31:2012–20.
Barenholz Y, Thompson TE. Sphingomyelin: biophysical aspects. Chem Phys Lipids. 1999;102:29–34.
Li J, Wang X, Zhang T, et al. A review on phospholipids and their main applications in drug delivery systems. Asian J Pharm Sci. 2015;10:81–98.
Webb M, Harasym T, Masin D, et al. Sphingomyelin-cholesterol liposomes significantly enhance the pharmacokinetic and therapeutic properties of vincristine in murine and human tumour models. Br J Cancer. 1995;72:896–904.
Semple SC, Leone R, Wang J, et al. Optimization and characterization of a sphingomyelin/cholesterol liposome formulation of vinorelbine with promising antitumor activity. J Pharm Sci. 2005;94:1024–38.
Liu M, Luo X, Qiu Q, et al. Redox-and pH-sensitive glycan (polysialic acid) derivatives and F127 mixed micelles for tumor-targeted drug delivery. Mol Pharm. 2018;15:5534–45.
Ding J, Sui D, Liu M, et al. Sialic acid conjugate-modified liposomes enable tumor homing of epirubicin via neutrophil/monocyte infiltration for tumor therapy. Acta Biomater. 2021;134:702–15.
Webb MS, Saxon D, Wong FM, et al. Comparison of different hydrophobic anchors conjugated to poly (ethylene glycol): effects on the pharmacokinetics of liposomal vincristine. Biochim Biophys Acta. 1998;1372:272–82.
Zheng H, Li J, Wang M, et al. Exhausting tumor associated macrophages with sialic acid-polyethyleneimine-cholesterol modified liposomal doxorubicin for enhancing sarcoma chemotherapy. Int J Pharm. 2019;558:187–200.
Karmakar S, Bhaumik SK, Paul J, De T. Leishmania donovani cell surface sialoglycans regulate susceptibility for siglec mediated macrophage invasion and parasite survival. J Mol Biochem. 2012;1:6–20.
Slotte JP. Sphingomyelin–cholesterol interactions in biological and model membranes. Chem Pys Lipids. 1999;102:13–27.
Boman NL, Cullis PR, Mayer LD, et al. Liposomal vincristine: the central role of drug retention in defining therapeutically optimized anticancer formulations. In: Long circulating liposomes: old drugs, new therapeutics. Springer; 1998. p. 29–49.
Bhuvaneswaran C, Mitropoulos KA. Effect of liposomal phospholipid composition on cholesterol transfer between microsomal and liposomal vesicles. Biochem J. 1986;238:647–52.
Allen T, Everest J. Effect of liposome size and drug release properties on pharmacokinetics of encapsulated drug in rats. J Pharmacol Exp Ther. 1983;226:539–44.
Senior J, Gregoriadis G. Stability of small unilamellar liposomes in serum and clearance from the circulation: the effect of the phospholipid and cholesterol components. Life Sci. 1982;30:2123–36.
Luo X, Hu L, Zheng H, et al. Neutrophil-mediated delivery of pixantrone-loaded liposomes decorated with poly (sialic acid)–octadecylamine conjugate for lung cancer treatment. Drug Deliv. 2018;25:1200–12.
Byrne JD, Betancourt T, Brannon-Peppas L. Active targeting schemes for nanoparticle systems in cancer therapeutics. Adv Drug Deliv Rev. 2008;60:1615–26.
Solinas G, Germano G, Mantovani A, Allavena P. Tumor-associated macrophages (TAM) as major players of the cancer-related inflammation. J Leukoc Biol. 2009;86:1065–73.
Qian B-Z, Pollard JWJC. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141:39–51.
Acknowledgements
The authors are grateful for the laboratory facilities support provided by Shenyang Pharmaceutical University.
Funding
This study was supported by the Career Development Support Plan for Young and Middle-aged Teachers at Shenyang Pharmaceutical University (ZDN2021009) and the Natural National Science Foundation of China (Grant Numbers 81973271).
Author information
Authors and Affiliations
Contributions
Conceptualization: Hongxia Zhang, Yihui Deng, and Yanzhi Song; data curation: Xianmin Meng, Hongxia Zhang, Yihui Deng, and Yanzhi Song; acquisition: Hongxia Zhang, Lingyan Chen, Mingqi Wang, and Kaituo Zhang; writing and analysis: Xianmin Meng; supervision: Xinrong Liu. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Meng, X., Zhang, H., Chen, L. et al. Liposomal Doxorubicin: the Sphingomyelin/Cholesterol System Significantly Enhances the Antitumor Efficacy of Doxorubicin. AAPS PharmSciTech 24, 64 (2023). https://doi.org/10.1208/s12249-022-02489-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-022-02489-1