Abstract
The purpose of this study was to develop and evaluate a new formulation of ziprasidone (ZIP) for improved fasted state absorption and sustained drug release. ZIP solid dispersions were produced via spray drying using Soluplus®, an amphiphilic polymer, as the solubility enhancer. Physicochemical analysis proved that ZIP presented at amorphous state in the spray-dried microparticles and the dissolution rate of ZIP from the Soluplus®-ZIP composite microparticles was significantly increased compared with that of the physical mixtures. Commonly used encapsulation materials including Eudragit® RL, Eudragit® S100 and Ethyl Cellulose were incorporated into the solid dispersions to regulate the drug release kinetics. The formulation containing ethyl cellulose provided the most sustained release behaviors. Pharmacokinetic studies in beagle dogs confirmed that there was no significant difference in oral bioavailability of the microparticles under fasted and fed states, and a prolonged Tmax value was simultaneously achieved compared with the commercial ZIP capsules.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Ziprasidone (ZIP) is an orally active atypical antipsychotic agent indicated for the monotherapy of schizophrenia and bipolar disorder (1,2,3). Despite the proved therapeutic efficacy, the oral bioavailability of ZIP is largely restricted by its low intrinsic solubility (4). Meanwhile, the oral drug absorption is significantly influenced by food intake and it is reported that the absorption of ZIP could increase up to two-fold in fed versus fasted state (5,6,7). Thus, the administration of medicament should be with foods and the time interval between dosing and food intake is another vital factor which affects the ZIP absorption (8,9,10). However, the commercially available ZIP products, such as Geodon® and Zeldox®, are both immediate release formulations, which should be dosed with food twice daily (4). Patients with schizophrenia are known to eat a poor diet, and about 50% of the patients do not necessarily comply with the medical instructions (11). The problematic patient compliance would certainly lead to serious dosing-related issues (12). There is an urgent need to develop new ZIP formulations with eliminated food effect and sustained release capability to ensure predictable bioavailability and optimal symptom control.
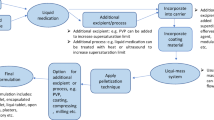
Numerous solubilization strategies have been developed in recent years to improve the poor and variable fasted state absorption of ZIP. The techniques investigated include complexation using β-cyclodextrins, solid dispersions, lipid-based delivery systems, and self-nanoemulsifying formulations (13,14,15,16). Formulations employing both solubilization and sustained release technologies were also reported. In these studies, self-nanoemulsifying formulation, ZIP-phospholipid complex, or solid dispersion were firstly prepared for solubility enhancement purpose and a subsequent treatment was required for the preparation of sustained release pellets or osmotic pump tablets (17,18,19). With the combination of these technologies, enhanced drug absorption in fasted state as well as prolonged in vivo actions were both achieved. However, the complex operation steps and high economic cost limit their industrial applications.
In this study, we aimed to develop a simple and easily scalable method for the production of sustained release ziprasidone formulations with eliminated food effect and enhanced bioavailability. A microfluidic jet spray drying technique was employed to produce ZIP formulations in a single step (20). An amphiphilic polymer polyvinyl caprolactam-polyvinyl acetate-polyethylene glycol graft copolymer (Soluplus®) was chosen as the carrier of ZIP with the purpose of solubility improvement. Soluplus® has been reported to possess excellent solubilizing properties for poorly water-soluble drugs and offers the possibility to form drug solid dispersions via spray drying. Meanwhile, we hypothesized that polymers with different hydrophobicity can be synchronously added into the immediate release solid dispersion systems during spray drying to adjust the drug release rate, which might be a promising approach to realize both the sustained release and improved dissolution of ZIP. Commonly used encapsulation polymers, i.e., Eudragit® RL, Eudragit® S100, and ethyl cellulose, were added into the precursors used for spray drying to tune the release rate of the drug. Performance of the developed formulations was characterized using scanning electron microscopy (SEM), X-ray powder diffraction (XRD), Fourier-transform infrared spectroscopy (FTIR), and in vitro dissolution tests. Pharmacokinetics of the ZIP formulations in fed and fasted state was studied in beagle dogs with commercial ZIP capsule used as control. With the employment of easily scalable spray drying production method, sustained release ZIP formulation with eliminated food effect might provide significant patient and physician benefit.
MATERIALS AND METHODS
Materials
Ziprasidone hydrochloride monohydrate was provided by Carbosynth China co., Ltd. Soluplus® was a kind gift from BASF Corporation, China. Ethyl cellulose (viscosity of 90 to 100 cp, ethoxy content of 44.0% to 51.0%) was purchased from Shanghai Macklin Biochemical Co., Ltd. Eudragit® RL and Eudragit® S100 were obtained from Shanghai Chineway Pharmaceutical Technology Co., Ltd. Ammonium acetate (CH3COONH4) and absolute ethanol (C2H5OH) of laboratory-grade were from Sinopharm Chemical Reagent Co. Ltd. (Shanghai, China). Methanol (CH3OH, ACS spectrophotometric grade) was obtained from Anaqua Chemicals. Deionized water was provided by a laboratory water purification system (Hitech Instruments Co., Ltd., shanghai, China).
Preparation of ZIP Formulations
The ZIP formulations were prepared using a microfluidic jet spray drying technique. For the preparation of Soluplus®-ZIP precursors, an appropriate amount of Soluplus® was dissolved in 300 mL of ethanol-water (2:1, v/v) followed by the addition of prescribed amount of ZIP forming a clear solution after ultrasonication. For the incorporation of encapsulation polymer, the encapsulation polymer (Eudragit® RL, Eudragit® S100 or Ethyl Cellulose) was pre-dissolved in 200 mL pure ethanol facilitated by ultrasonication, and 100 mL water was added subsequently to get a solvent system of ethanol-water (2:1, v/v). The procedure for the addition of Soluplus® and ZIP was the same as the preparation of Soluplus®-ZIP precursors. The prepared precursors were spray dried using a Mono Disperse Spray Dryer (China Nantong Dong-Concept New Material Technology Co., Ltd.) to form ZIP composite microparticles. Monodisperse droplets were generated using a microfluidic aerosol nozzle system with an orifice diameter of 100 μm (21). The flow rate of disperse air was set at 12 L/min. The well-dispersed droplets were dried with 180°C and 80°C as the inlet and outlet temperatures, respectively. The spray-dried microparticles were collected from the collection vessel at the bottom of the dryer and then stored in a desiccator. Formulations of the spray-dried microparticles were summarized in Table I.
PHYSICOCHEMICAL CHARACTERIZATIONS
Scanning Electron Microscope (SEM)
The morphologies of pure ZIP, pure Soluplus®, and spray-dried samples were examined using a scanning electron microscope (JSM-IT300LA, JEOL, Tokyo, Japan) at an acceleration voltage of 15 kV. The samples were coated with a thin gold-palladium layer by sputter coater (JEOL, Japan). Size of the spray-dried microparticles was obtained by analyzing the SEM images using the Image J™ software. The average particle size (\( \overline{d} \)) was defined as \( \overline{d}={\sum}_{i=1}^n\Big({d}_i \))/N, and the standard deviation of the particle size was described as SD=\( {\left(\left(\sum {\left({d}_i-\overline{d}\right)}^2\right)/\left(N-1\right)\right)}^{1/2} \), where di was the diameter of the ith particle and N was the total number of particles counted.
X-Ray Powder Diffraction (XRD)
X-ray powder diffraction measurements were carried out using an Advance D8 X-ray diffractometer (BRUKER, Switzerland) with Cu Kα radiation (λ = 1.54 Å). Each sample was scanned in the range of 3–40° (2θ) at a rate of 1° per second.
Fourier-Transform Infrared Spectroscopy (FTIR)
FTIR spectra were obtained using an FTIR spectrophotometer (SHIMADZU, IRTracer-100). The procedure consisted of dispersing a sample in KBr followed by gentle mixing, and this mixture was converted into a disc by using KBr press. The disc was kept in a sample holder of FTIR spectrophotometer and scanned in the range of 400–4000 cm−1 at a resolution of 2 cm−1.
In Vitro Dissolution Test and Drug Loading Efficiency
In vitro dissolution tests were carried out using Chinese Pharmacopeia type II Apparatus, paddle method (Tianda Tianfa Technology Co., Ltd) in 900 mL of deionized water at a temperature of 37 ± 0.5°C and 50 rpm rotation speed (22). Meanwhile, we also tested the release of ZIP from physical mixtures of Soluplus® and ZIP (6:1) from dissolution medium of different pH values, it was found that the release of ZIP in dissolution medium of deionized water was relatively faster than that in dissolution media of 0.1 M HCl or PBS with the pH of 6.8 (as shown in Fig. 1). Considering the low aqueous solubility of ZIP, deionized water in which ZIP displayed relatively fast release rate was used as the dissolution medium. Each formulation containing 20 mg ZIP was filled into a gelatin capsule and introduced into the dissolution medium. At predetermined time intervals, 2 mL samples were withdrawn and replaced with fresh medium. The samples were filtered (0.45 μm) and analyzed via a HPLC system (Agilent 1200, Agilent Technologies, Inc.) with a TC-C18 (2) column (250 mm × 4.6 mm, 5 mm). The variable UV detector was set at 254 nm. The mobile phase was a mixture of 0.05 mol/L ammonium acetate and methanol at the ratio of 15/85 (v/v), eluted at a flow rate of a 1.0 mL/min. This HPLC assay had a linear peak-area response from 0.625 to 40 μg/mL. All the experiments were done in triplicate.
The amount of ZIP loaded into the formulations was determined by adding an accurately weighted amount of microparticles (around 25 mg) in 50 mL of ethanol-water (2:1, v/v), followed by complete extraction of the loaded ZIP with ultrasonification. The samples were filtered (0.45 μm) and analyzed via the HPLC method as described before. The drug loading efficiency was calculated by dividing the amount of drug in the microparticles by the initial amount of drug added. All the experiments were done in triplicate.
Pharmacokinetic Studies in Beagle Dogs
The in vivo pharmacokinetic experiment was approved by the Animal Management and Ethics Committee of Hunan Provincial Drug Safety Evaluation Research Center (China). The commercial ZIP formulation (Zeldox®, 20 mg of ZIP) and the optimal spray dried ZIP formulation were both tested under fasted and fed states with two groups of laboratory beagle dogs (n = 6). The tested formulation of spray-dried microparticles containing 20 mg ZIP was filled into a gelatin capsule.
The fed treatment group was given a diet of 150 g dry dog food (containing ≥ 50% w/w crude fat) 0.5 h prior to dosing, while the fasted treatment group were fasted 12 h pre-dose and 12 h post-dose. Water was accessible at all time. Venous blood samples (4 mL) were collected into heparinized test tubes at predetermined time intervals and centrifuged at 4000 rpm for 10 min. The supernatant plasma samples were stored at − 20°C until assayed. The drug content in the plasma were analyzed using the HPLC system as described before with clozapine employed as an internal standard. In detail, 20 μL of an internal standard solution (40 μg/mL in methanol) was added into 1.0 mL plasma sample in a 10-mL Eppendorf tube. The mixture was vortexed for 1 min, then 5 ml ethyl acetate was added and followed by vortexing for 3 min to extract analytes. Subsequently, the contents of the tube were centrifuged at 4000 rpm for 10 min, then the upper organic layer was carefully transferred to a new tube and was dried under nitrogen gas flow at 50°C. One hundred microliter mobile phase was added to redissolve samples, and 20 μL of each sample was subjected to HPLC analysis. The mobile phase consisted of 0.05 M ammonium acetate and methanol (27:73 v/v) and eluted at a flow rate of 1.0 mL/min. The effluents were monitored by a UV detector at 254 nm. The pharmacokinetic parameters were determined using WINNONLIN® software version 6.1 (Certara, USA).
Statistical Data Analysis
All the data were demonstrated as mean ± standard deviation. Statistical analysis was performed by SPSS version 21.0 (IBM, USA). Analysis of variance was conducted for Cmax, AUC0 − t, AUC0 − ∞, and mean residence time (MRT) and a non-parametric test was performed for Tmax. The level of significance was set at p < 0.05.
RESULTS AND DISCUSSION
XRD Analysis
Figure 2 displayed the XRD profiles for pure ZIP, Soluplus®, ethyl cellulose, and representative samples of spray-dried microparticles as well as their physical mixtures (PM-1 & PM-2). The crystalline ZIP exhibited intense and sharp characteristic peaks at diffraction angle (2θ) values of 10.8°, 14.8°, 15.8°, 16.1°, 16.8°, 18.0°, 19.0°, 19.5°, 24.3°, 24.8°, 25.5°, 25.9°, 26.4°, 27.9°, and 28.8° (23). XRD patterns of Soluplus® and ethyl cellulose did not exhibit any obvious diffraction peaks and thus confirmed that it was in the amorphous state. Similarly, obvious crystalline peaks of ZIP were also observed in the physical mixtures of drug and excipients mixed in the same ratio, which suggested that the excipients had no effect on the drug crystalline transition under the physically mixed state. For the samples of spray-dried microparticles, the characteristic peaks of ZIP at corresponding 2θ angles disappeared and were replaced with a broad hump implying the amorphous nature of the loaded drug. And it was confirmed that ZIP was successfully transferred to its amorphous form and was well dispersed into the amorphous polymeric matrix during the rapid convective evaporation process in spray dryer.
FTIR Analysis
The FTIR spectra of ZIP, Soluplus®, ethyl cellulose, representative samples of solid dispersions, and their physical mixtures (PM-1 & PM-2) were depicted in Fig. 3. The FTIR spectra of ZIP displayed characteristic bands at 3354 cm−1 (for NH stretch vibration), 1713 cm−1 (C=O stretch vibration), 972 cm−1 (C=N stretch vibration), and 745 cm−1 (C–H binding), which was in agreement with previously reported data (17). Soluplus® demonstrated characteristic broad bands around 3200–3700 cm−1 and aliphatic C–H stretch at 2927 cm−1 due to the stretching of O–H and C–H, respectively. And the peaks at 1635 and 1740 cm−1 could be attributed to C=O stretch. Formation of hydrogen bond between the loaded drug and Soluplus® were confirmed by weak interactions observed at 1033 cm−1 (24,25). The carbonyl peaks of free and hydrogen-bonded carboxylic acid C=O of ZIP appeared at 1630 and 1713 cm−1, which also presented in PM-1 (1632 and 1716 cm−1) and PM-2 (1632 and 1715 cm−1). However, in case of the composite microparticles, these peaks were found to shift from the original ketone stretch of 1713 to 1740 cm−1. The hydrogen bond formation between Soluplus® and ZIP was also confirmed by the resultant broad peak at 3470 cm−1. These two selected formulations of composite microparticles displayed very similar FTIR spectra with shifted and broadened peaks of ZIP compared to that of pure ZIP. These FTIR results proved that intermolecular interactions occurred between ZIP and polymers in the composite microparticles.
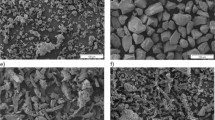
SEM Analysis
The overview and surface morphology of pure ZIP, Soluplus®, representative spray-dried microparticles (SZ-1 and SZEC-5) were displayed in Fig. 4. Pure ZIP crystals presented rod-shaped morphology (Fig. 4a1 and a2) while the Soluplus® particles exhibited near spherical shape with rugged surface and pores as seen in Fig. 4b1 and b2. SEM micrographs for SZ-1 microparticles (Fig. 4c1 and c2) displayed internally collapsed pleated particles with smooth surface on which rod-shape crystals were not seen. This probably attribute to the complete miscibility of the drug and polymer. The SZEC-5 microparticles (Fig. 4d1 and d2) show a wrinkled appearance. And the absence of drug crystals on the particle surface further indicated that the drug was well dispersed in the polymer matrix.
The particle size of microparticles spray dried from different formulations were summarized in Table I, indicating relatively uniform particle size distributions. The microfluidic aerosol nozzle system used for atomization could work stably for more than 5 h in continuous mode to obtain a relatively high production rate in terms of the production of uniform particles (26). And the process can be easily scalable by the employment of multiple nozzles (27).
In Vitro Dissolution Test and Drug Loading Efficiency
The drug loading efficiency of different formulations (also close to 100%) were shown in Table I, indicating that all drugs in the atomized droplets were successfully transferred into the spray dried microparticles. Dissolution profiles of spray-dried ZIP-Soluplus® composite microparticles (SZ) and physical mixtures of ZIP and Soluplus® were depicted in Fig. 5a. It was found that the ZIP release rate from SZ microparticles was significantly faster than that of the physical mixtures. For all the SZ microparticles, more than 80% of the loaded drugs were released within 2 h, while that of the physical mixtures only achieved around 40% drug release. The improved dissolution of ZIP from SZ microparticles was largely due to the amorphous state of ZIP in the spray-dried powder and the formation of solid dispersions with amphiphilic Soluplus® polymer which were in well agreement with the XRD measurements (28). The ratio of ZIP and Soluplus® did not display clear influence on the drug release rate for both the physical mixtures and spray dried SZ microparticles. Thus, the formulation of SZ-1 (Soluplus®:ZIP = 4:1) which would allow high drug loading was further studied for the incorporation of sustained release materials.
Drug released profiles of different ZIP formulations. a solid dispersion and physical mixture of ZIP and Soluplus® (PM-1: physical mixture of Soluplus® and ZIP in ratio of 4:1, PM-2: physical mixture of Soluplus® and ZIP in ratio of 6:1); b solid dispersions containing Eudragit® RL; c solid dispersions containing Eudragit® S100; d solid dispersions containing ethyl cellulose. Data were expressed as mean ± SD (n = 3)
Commonly used encapsulation polymers, i.e., Eudragit® RL, Eudragit® S100 and ethyl cellulose, was incorporated into the precursors for spray drying to investigate their ability for sustained release of ZIP. The release curves of ZIP from composite microparticles with different encapsulation polymers were shown in Fig. 5b–d. The formulations incorporated with Eudragit® RL did not show clear sustained release behaviors possibly due to the high permeability of Eudragit® RL polymer (Fig. 5b). While the incorporation of Eudragit® S100 incurred significant sustained release effect on the spray dried microparticles (Fig. 5c). Eudragit® S100 is a commonly used enteric polymer which was not soluble in water and low pH values. The Eudragit® S100 containing formulations would have different drug release profiles in dissolution media of different pH values. However, according to the results of in vitro dissolution test in deionized water, a large proportion of the loaded drug in the Eudragit® S100 containing formulations was locked and cannot be released until 12 h. Meanwhile, according to the solubility characteristic of Eudragit® S100, it may not be able to provide sustained release effect in dissolution medium of high pH values. Thus, the drug release properties of Eudragit® S100 containing formulations were not further studied in different release media.
When ethyl cellulose was used as the sustained release material, it has a certain effect on delaying drug release. As shown in Fig. 5d, small amount of ethyl cellulose incurred significant delay of drug release (SZEC-1 and SZEC-2). With the increase of ethyl cellulose, however, the drug release of SZEC-3 microparticles became relatively faster which was in contrast to the sustained release effect of ethyl cellulose as described in the literature. The abnormal drug release behaviors of SZEC-1 and SZEC-2 microparticles could be explained by the particle agglomeration in release medium and it was observed that the microparticles maintained as an agglomerate during the whole period of release test. Meanwhile, the amount of Soluplus® was further tuned to adjust the drug release rate and it was shown that a well sustained release effect could be achieved when the ratio of Soluplus® to drugs and ethyl cellulose (EC) was 6:1:4. As shown in Fig. 5d, about 20% of the loaded drug was released in the first 2 h and a total of around 80% of the loaded drug were released in 12 h for the formulation of SZEC-5. Therefore, this formulation (SZEC-5) was selected for the subsequent in vivo pharmacokinetic study in beagle dogs.
In Vivo Pharmacokinetics
The mean ZIP concentration versus time profiles following oral administration of Zeldox® capsule and SZEC-5 capsule to fasted and fed dogs were shown in Fig. 6. The corresponding mean pharmacokinetic parameters for Zeldox® capsule and SZEC-5 capsule were tabulated in Table II. As the data shown, the plasma concentration of ZIP from Zeldox® capsules increased quickly and reached maximum at 1.25 ± 0.27 h and 1.91 ± 0.58 h in fed and fasted state, and then decreased rapidly. Meanwhile, the maximum plasma concentration for SZEC-5 capsules was reached at 4.33 ± 0.51 h and 4.33 ± 0.81 h in fed and fasted state and decreased more slowly than that of the Zeldox® capsule. The Cmax values of SZEC-5 capsules in fed and fasted states were 862.73 ± 431.91 ng/mL and 723.27 ± 176.69 ng/mL, respectively, which were both comparable to that of Zeldox® capsules administrated in fed state. The results revealed that the formulation of SZEC-5 solid dispersion significantly enhanced and prolonged in vivo absorption of ZIP.
No significant difference was found in Cmax, Tmax, and AUC values between the fasted and fed states of SZEC-5 capsule. On the contrary, Zeldox® showed significant difference in Cmax between the fasted and fed state with P < 0.01. Zeldox® capsule exhibited a more positive food effect in dogs, which was similar to that of the reported clinical data (7). The comparable AUC and Cmax for SZEC-5 capsule between the fasted and fed state indicated essentially no food effect of the formulation on drug absorption. The AUC and Cmax of SZEC-5 capsule in fed state showed no significant difference compared with Zeldox® capsule in corresponding state, while the significant difference observed in Tmax and MRT meant that a sustained release formulation of ZIP had been prepared successfully. The results from in vivo pharmacokinetic study clearly demonstrated that a sustained release formulation of ZIP with enhanced oral drug absorption and eliminated food effect was achieved in SZEC-5 capsule.
CONCLUSIONS
In this paper, an improved formulation of ZIP solid dispersion was developed. Physicochemical characterization confirmed that ZIP was present in an amorphous state in the microparticles of solid dispersions. From the in vitro dissolution tests, the SZEC-5 capsule exhibited sustained release characteristics of ZIP. For the in vivo pharmacokinetic study, enhanced drug absorption, prolonged Tmax, and eliminated food effect were simultaneously achieved for the SZEC-5 capsule, indicating a sustained release with prolonged actions of potential schizophrenia and bipolar disorder treatment. Such formulations could provide simple and convenient dosing while retaining the familiar safety and efficacy profile of currently marketed capsules. And the formulation development strategy presented here might shed some light on the design of sustained release formulations of other poorly water-soluble drugs in the future.
Abbreviations
- AUC:
-
Area under the curve
- ZIP:
-
Ziprasidone
- SEM:
-
Scanning electron microscopy
- XRD:
-
X-ray diffraction
- FTIR:
-
Fourier-transform infrared spectroscopy
- HPLC:
-
High-performance liquid chromatography
- SOL:
-
Soluplus®
- RL:
-
Eudragit® RL
- S100:
-
Eudragit® S100
- EC:
-
Ethyl cellulose
- PM-1:
-
Physical mixture of Soluplus® and Ziprasidone (4:1)
- PM-2:
-
Physical mixture of Soluplus®, Ziprasidone and Ethyl Cellulose (6:1:4)
- SZ-1:
-
Soluplus®: Ziprasidone = 4:1
- SZEC-5:
-
Soluplus®: Ziprasidone: Ethyl Cellulose = 6:1:4
- MRT:
-
Mean residence time
References
Greenberg WM, Citrome L. Ziprasidone for schizophrenia and bipolar disorder: a review of the clinical trials. CNS Drug Rev. 2007;13(2):137–77. https://doi.org/10.1111/j.1527-3458.2007.00008.x.
Harvey PD, Bowie CR. Ziprasidone: efficacy, tolerability, and emerging data on wide-ranging effectiveness. Expert Opin Pharmacother. 2005;6(2):337–46. https://doi.org/10.1517/14656566.6.2.337.
Patel NC, Keck PE Jr. Ziprasidone: efficacy and safety in patients with bipolar disorder. Expert Rev Neurother. 2006;6(8):1129–38. https://doi.org/10.1586/14737175.6.8.1129.
Zakowiecki D, Cal K, Kaminski K, Adrjanowicz K, Swinder L, Kaminska E, et al. The improvement of the dissolution rate of ziprasidone free base from solid oral formulations. AAPS PharmSciTech. 2015;16(4):922–33. https://doi.org/10.1208/s12249-015-0285-1.
Xue X, Chen G, Xu X, Wang J, Wang J, Ren L. A combined utilization of Plasdone-S630 and HPMCAS-HF in ziprasidone hydrochloride solid dispersion by hot-melt extrusion to enhance the oral bioavailability and no food effect. AAPS PharmSciTech. 2019;20(1):37. https://doi.org/10.1208/s12249-018-1216-8.
Sachs GS, Ice KS, Chappell PB, Schwartz JH, Gurtovaya O, Vanderburg DG, et al. Efficacy and safety of adjunctive oral ziprasidone for acute treatment of depression in patients with bipolar I disorder: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2011;72(10):1413–22. https://doi.org/10.4088/JCP.09m05934.
Lincoln J, Stewart ME, Preskorn SH. How sequential studies inform drug development: evaluating the effect of food intake on optimal bioavailability of ziprasidone. J Psychiatr Pract. 2010;16(2):103–14.
Gandelman K, Alderman JA, Glue P, Lombardo I, LaBadie RR, Versavel M, et al. The impact of calories and fat content of meals on oral ziprasidone absorption: a randomized, open-label, crossover trial. J Clin Psychiatry. 2009;70(1):58–62.
Hamelin BA, Allard S, Laplante L, Miceli J, Wilner KD, Tremblay J, et al. The effect of timing of a standard meal on the pharmacokinetics and pharmacodynamics of the novel atypical antipsychotic agent ziprasidone. Pharmacotherapy. 1998;18(1):9–15.
Gu CH, Li H, Levons J, Lentz K, Gandhi RB, Raghavan K, et al. Predicting effect of food on extent of drug absorption based on physicochemical properties. Pharm Res. 2007;24(6):1118–30. https://doi.org/10.1007/s11095-007-9236-1.
Perkins DO. Predictors of noncompliance in patients with schizophrenia. J Clin Psychiatry. 2002;63(12):1121–8.
Thombre AG, Shamblin SL, Malhotra BK, Connor AL, Wilding IR, Caldwell WB. Pharmacoscintigraphy studies to assess the feasibility of a controlled release formulation of ziprasidone. J Control Release. 2015;213:10–7. https://doi.org/10.1016/j.jconrel.2015.06.032.
Thombre AG, Shah JC, Sagawa K, Caldwell WB. In vitro and in vivo characterization of amorphous, nanocrystalline, and crystalline ziprasidone formulations. Int J Pharm. 2012;428(1–2):8–17. https://doi.org/10.1016/j.ijpharm.2012.02.004.
Dening TJ, Rao S, Thomas N, Prestidge CA. Silica encapsulated lipid-based drug delivery systems for reducing the fed/fasted variations of ziprasidone in vitro. Eur J Pharm Biopharm. 2016;101:33–42. https://doi.org/10.1016/j.ejpb.2016.01.010.
Thombre AG, Caldwell WB, Friesen DT, McCray SB, Sutton SC. Solid nanocrystalline dispersions of ziprasidone with enhanced bioavailability in the fasted state. Mol Pharm. 2012;9(12):3526–34. https://doi.org/10.1021/mp3003607.
Thombre AG, Herbig SM, Alderman JA. Improved ziprasidone formulations with enhanced bioavailability in the fasted state and a reduced food effect. Pharm Res. 2011;28(12):3159–70. https://doi.org/10.1007/s11095-011-0505-7.
Miao Y, Chen G, Ren L, Ouyang P. Preparation and evaluation of ziprasidone-phospholipid complex from sustained-release pellet formulation with enhanced bioavailability and no food effect. J Pharm Pharmacol. 2016;68(2):185–94.
Miao Y, Chen G, Ren L, Pingkai O. Characterization and evaluation of self-nanoemulsifying sustained-release pellet formulation of ziprasidone with enhanced bioavailability and no food effect. Drug Deliv. 2015;23(7):1.
Miao Y, Chen G, Ren L, Ouyang P. Controlled release of ziprasidone solid dispersion systems from osmotic pump tablets with enhanced bioavailability in the fasted state. Drug Dev Ind Pharm. 2015;41(8):1353.
Yang W, Liu W, Xiao DC, Selomulya C. Micro-encapsulation and stabilization of DHA containing fish oil in protein-based emulsion through mono-disperse droplet spray dryer. J Food Eng. 2016;175:74–84.
Wu WD, Amelia R, Hao N, Selomulya C, Zhao DY, Chiu YL, et al. Assembly of uniform photoluminescent microcomposites using a novel micro-fluidic-jet-spray-dryer. AICHE J. 2011;57(10):2726–37.
Yanfei M, Guoguang C, Lili R, Pingkai O. Controlled release of ziprasidone solid dispersion systems from osmotic pump tablets with enhanced bioavailability in the fasted state. Drug Dev Ind Pharm. 2015;41(8):1353–62. https://doi.org/10.3109/03639045.2014.950273.
Bera H, Boddupalli S, Nayak AK. Mucoadhesive-floating zinc-pectinate-sterculia gum interpenetrating polymer network beads encapsulating ziprasidone HCl. Carbohydr Polym. 2015;131:108–18. https://doi.org/10.1016/j.carbpol.2015.05.042.
Pawar JN, Shete RT, Gangurde AB, Moravkar KK, Javeer SD, Jaiswar DR, et al. Development of amorphous dispersions of artemether with hydrophilic polymers via spray drying: physicochemical and in silico studies. Asian J Pharm Sci. 2016;11(3):385–95.
Rumondor AC, Stanford LA, Taylor LS. Effects of polymer type and storage relative humidity on the kinetics of felodipine crystallization from amorphous solid dispersions. Pharm Res. 2009;26(12):2599–606. https://doi.org/10.1007/s11095-009-9974-3.
Wu WD, Lin SX, Chen XD. Monodisperse droplet formation through a continuous jet break-up using glass nozzles operated with piezoelectric pulsation. AICHE J. 2011;57(6):1386–92.
Wu WD, Patel KC, Rogers S, Chen XD. Monodisperse droplet generators as potential atomizers for spray drying technology. Dry Technol. 2007;25(12):1907–16.
Truong DH, Tran TH, Ramasamy T, Choi JY, Choi HG, Yong CS, et al. Preparation and characterization of solid dispersion using a novel amphiphilic copolymer to enhance dissolution and oral bioavailability of sorafenib. Powder Technol. 2015;283:260–5.
Acknowledgements
The authors would like to acknowledge financial support from National Natural Science Foundation of China (Grant No. 81503023).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, W., Wang, S., Lu, W. et al. Sustained Release Ziprasidone Microparticles Prepared by Spray Drying with Soluplus® and Ethyl Cellulose to Eliminate Food Effect and Enhance Bioavailability. AAPS PharmSciTech 21, 27 (2020). https://doi.org/10.1208/s12249-019-1592-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-019-1592-8