Abstract
Over the past 20 years, solution-based spray dried powders have transformed inhaled product development, enabling aerosol delivery of a wider variety of molecules as dry powders. These include inhaled proteins for systemic action (e.g., Exubera®) and high-dose inhaled antibiotics (e.g., TOBI® Podhaler™). Although engineered particles provide several key advantages over traditional powder processing technologies (e.g., spheronized particles and lactose blends), the physicochemical stability of the amorphous drug present in these formulations brings along its own unique set of constraints. To this end, a number of approaches have been developed to maintain the crystallinity of drugs throughout the spray drying process. One approach is to spray dry suspensions of micronized drug(s) from a liquid feed. In this method, minimization of drug particle dissolution in the liquid feed is critical, as dissolved drug is converted into amorphous domains in the spray-dried drug product. The review explores multiple formulation and engineering strategies for decreasing drug dissolution independent of the physicochemical properties of the drug(s). Strategies to minimize particle dissolution include spray blending of particles of different compositions, formation of respirable agglomerates of micronized drug with small porous carrier particles, and use of common ions. The formulations extend the range of doses that can be delivered with a portable inhaler from about 100 ng to 100 mg. The spray-dried particles exhibit significant advantages in terms of lung targeting and dose consistency relative to conventional lactose blends, while still maintaining the crystallinity of drug(s) in the formulated drug product.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
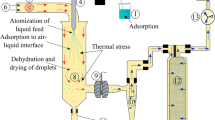
Spray drying is a process for producing a dry powder by using a hot gas to rapidly dry atomized liquid droplets. In its simplest embodiment, the liquid feed is comprised of a solution of drug dissolved in water, an organic solvent, or a mixture of the two (1,2,3). During spray drying, each atomized droplet becomes a solid particle. Because particle formation occurs on the millisecond timescale, most dissolved species have insufficient time for crystal nucleation and growth. As a result, inhaled therapeutics made via spray-drying of drug solutions typically comprise amorphous drug particles.
There are a large number of examples of inhalation particles prepared by spray drying from solution-based feeds, some of which are detailed in the following references (4,5,6,7,8,9,10,11,12). Exubera® (recombinant human insulin inhalation powder) and TOBI® Podhaler™ (tobramycin inhalation powder) represent the first spray-dried amorphous solids for inhalation to have achieved marketing authorization (11,12). The physical and chemical stability of amorphous formulations may be improved via the inclusion of buffers and glass-forming excipients, with room temperature stability of 2 years or more readily achievable provided that the powders are suitably formulated and packaged (11,12,13,14,15). Control of the surface composition with a hydrophobic shell-forming excipient (e.g., phospholipids, leucine, trileucine) enables high total lung doses (TLD) from about 40 to 90% of the nominal dose to be achieved (16,17,18). In addition to the improvements in lung targeting, spray-dried particles exhibit significant improvements in dose consistency, as reflected in reduced variability associated with oropharyngeal filtering of particles (19,20) and dose delivery that is largely independent of a patient’s inspiratory flow profile (19,20,21). The improved dispersibility of spray-dried porous particles enables effective dose delivery of dry powder formulations even at pressure drops as low as 0.2 kPa, i.e., less than what pediatric asthma patients achieve in periods of acute wheeze (21,22). The hydrophobic shell-forming excipients may also improve the environmental robustness of spray-dried amorphous formulations (23,24).
Although there are multiple approved amorphous drug products, such products tend to carry additional development risk and require demonstration of characterization and control of the amorphous form. The molecular mobility of an amorphous solid is significant when compared to that of its crystalline counterpart, and this mobility can lead to undesirable physical and chemical changes. Even small amounts of amorphous material may compromise the chemical and physical stability of a formulated drug product. Indeed, Ahlneck and Zografi suggested that most physical instability problems observed in pharmaceutical solids occur preferentially in the disordered non-crystalline regions (25).
Thus, there remains a strong preference for the use of crystalline drugs in pharmaceutical development, including inhaled drug products. Crystallization is the preferred approach to isolate and purify a compound in drug synthesis. Besides typically having a high degree of purity, crystalline drugs are often highly stable, particularly if the most thermodynamically stable polymorph has been selected. While some low molecular weight drugs can be crystallized from solution during spray drying (e.g., inorganic salts, metformin, isoniazid, naproxen), these molecules typically have molecular weights less than about 250 g/mol (26,27,28). Most inhaled therapeutics have higher molecular weights, particularly if therapeutics with improved lung targeting are desired (29,30,31). As a result, alternative process strategies are needed to maintain the crystallinity of larger-sized small molecule drugs while also achieving the benefits of particle engineering detailed above. One option is to spray dry a suspension of micronized drug with a shell-forming excipient that modifies the surface characteristics (e.g., hydrophobicity, rugosity, porosity) of the resulting engineered particles [32]. Maintaining the solid-state form of a crystalline solid when it is dispersed in a liquid can be challenging, however, as any dissolution of drug in the liquid feed may result in physical and chemical stability issues. Chief among these concerns is the formation of amorphous domains that adversely impact the physical and chemical stability of the drug substance. Additionally, drug dissolution may lead to hydrate or solvate formation, to disproportionation of salts to form the free base and corresponding acid, or to particle coarsening due to molecular diffusion (Ostwald ripening). The present review will provide examples of spray-dried formulations that maintain the crystallinity of the drug substance while achieving the performance benefits of spray-dried engineered particles prepared by solution-based spray drying. The review will further focus on formulation and engineering mitigations to minimize drug dissolution and to maintain the physical and chemical stability of the crystalline drug in the formulated drug product.
THE PULMOSPHERE™ TECHNOLOGY
The examples detailed herein are based on spray drying of crystalline drugs with the PulmoSphere™ technology (20). The PulmoSphere technology produces small porous particles via spray drying of a liquid feed comprising a perfluorooctyl bromide (PFOB)-in-water emulsion. The sub-micron PFOB emulsion droplets are stabilized by an interfacial layer comprising a long-chain phospholipid (distearoylphosphatidylcholine, DSPC) and calcium chloride present in a 2:1 mol:mol ratio. There are three formats available for incorporation of drug with the small porous PulmoSphere particles. In the solution-based format, the drug is simply dissolved in the continuous phase of the emulsion, and the drug-containing emulsion is spray-dried. This typically results in formation of a highly porous composite particle containing amorphous drug and PulmoSphere excipients, with the hydrophobic shell-forming PulmoSphere excipients enriched at the particle surface. In the suspension-based format, micronized drug particles are suspended within the emulsion feed and spray-dried, resulting in amorphous or crystalline drug particles coated with a porous layer of excipients. Finally, in the carrier-based format, small porous placebo particles containing just the PulmoSphere excipients are used as carriers for micronized drug particles. In this case, the small porous placebo particles and micronized drug particles are dispersed in a liquid feed comprising a fluorinated non-solvent. Evaporation of the liquid feed via spray drying leads to formation of agglomerates of the drug and small porous carrier particles. In the context of the present discussion, the suspension and carrier-based PulmoSphere formats enable maintenance of the crystallinity of a drug substance and will be discussed in greater detail below.
Each of the formats can be administered with a range of delivery systems including dry powder inhalers (DPIs), pressurized metered dose inhalers, and nebulizers. The particles may also be administered via liquid dose instillation in a fluorinated liquid in conjunction with liquid ventilation or liquid breathing (33,34). Most of the discussion which follows, however, is focused on delivery with DPIs.
SUSPENSION-BASED SPRAY DRYING
In suspension-based PulmoSphere feeds, each atomized droplet (mass median diameter ~ 10 μm) contains dispersed drug crystals and approximately 1000 sub-micron emulsion droplets (Fig. 1) (35). During the initial moments of the drying process, the more volatile aqueous phase begins to evaporate. The rapidly receding atomized droplet interface drives enrichment of the slowly diffusing drug and emulsion particles at the interface. This leads to formation of a void space in the center of the drying droplet. As the drying process continues, the less volatile oil phase in the emulsion droplets evaporates, resulting in formation of hollow pores in their place. Overall, the resulting hollow spray-dried composite particles contain drug crystals embedded in an interfacial layer of a porous phospholipid matrix (Fig. 1). For a detailed discourse on spray drying of suspension-based feeds, the reader is referred to the excellent publications by Vehring et al. (2,3,35).
Figure 1 also presents scanning electron microscopy (SEM) images of several suspension-based PulmoSphere formulations, illustrating the presence of the characteristic porous morphology at the particle surface (32,36,37). The characteristics of these suspension-based drug products will be described in greater detail in the examples that follow.
As intimated above, the millisecond timescale of particle formation during spray-drying typically results in conversion of any drug dissolved in the liquid medium into an amorphous solid. The percentage of drug dissolved in a suspension-based feed can be calculated from Eq. 1 (38,39).
where SAPI is the solubility of the drug in the suspension medium (mg/ml), mfill is the fill mass (mg), ϕoil is the volume fraction of oil in a suspension medium that also contains dispersed oil droplets, Csolids is the solids concentration in the suspension medium (mg/ml), and Dnom is the nominal dose of the drug (mg). The ratio of Dnom/mfill is often termed the drug loading (mg/mg) in the formulation, and is expressed as XAPI.
For a 3-mg fill mass and a typical feed composition (i.e., ϕoil = 0.2, Csolids = 30 mg/ml), the %Dissolved can be approximated by a simple ratio of solubility to nominal dose, viz.:
Inhaled therapeutics, particularly those for the treatment of asthma and COPD, are often highly potent with nominal doses less than 0.1 mg. Current high-speed filling machines are unable to accurately and precisely fill these low doses. The minimum fill mass with drum fillers is about 1 to 3 mg, depending on the nature of the formulation and the micromeritic properties of the powder (e.g., bulk density). As such, the drug loading (XAPI) values of potent drugs are often quite low. For example, for a 0.1-mg nominal dose in a 3-mg fill mass, XAPI is just 0.03. Even materials that are classified as being “practically insoluble” (SAPI < 0.1 mg/ml) can have a %Dissolved of ~ 10%, if the nominal dose is less than 0.08 mg (80 μg). Given that small amounts (< 1%) of amorphous material can adversely affect the physical and chemical stability of the drug substance, the magnitude of %Dissolved is of concern. Preventing particle dissolution represents a critical process parameter for development of spray-dried formulations using suspension-based feeds.
Ciprofloxacin DPI
The first suspension-based spray-dried drug product to advance into late-stage clinical development is ciprofloxacin DPI (Bayer Healthcare, Berlin, Germany) (36,40,41). The PulmoSphere formulation is comprised of crystalline ciprofloxacin betaine 3.5 hydrate particles (i.e., the zwitterionic form of the drug crystallized at neutral pH) coated with a porous layer of DSPC/CaCl2 (Fig. 1c) (20,36,40,41). The formulated drug product is currently being developed for the treatment of chronic lung infections in bronchiectasis patients. It has also been studied in cystic fibrosis and COPD patients. The drug is administered twice daily via inhalation of the contents of a single capsule containing 50 mg of spray-dried powder (32.5 mg ciprofloxacin) with the portable T-326 dry powder inhaler.
The practically insoluble zwitterionic form of the drug was selected for development instead of the commonly used hydrochloride salt due to its improved “lung targeting” resulting from its reduced clearance rate from the lungs. The increased residence time of ciprofloxacin betaine in the lungs is associated with improved efficacy in a chronic infection model in rats, as evidenced by dramatic reductions in colony forming units of Pseudomonas aeruginosa relative to the more soluble hydrochloride salt (36).
The aerodynamic particle size distribution (APSD) is an important factor in achieving high delivery efficiency of a drug to the lungs. The APSD of suspension-based PulmoSphere particles depends to a significant extent on the size distribution of the micronized drug particles incorporated therein. The APSD is also influenced by the particle size distribution of the atomized droplets and other formulation variables, including the solids composition and concentration, and the volume fraction of the pore-forming oil phase (34). In the case of ciprofloxacin, the jet-milled crystals have a volume-weighted median diameter (X50) of about 2.5 μm (40). The mass median aerodynamic diameter (MMAD) of the spray-dried composite particles ranges from about 3.4 to 3.9 μm (36).
Given that particles interact with each other via their surfaces, engineering of surface morphology plays an important role in aerosol performance. Based on X-ray photoelectron spectroscopy, 96% of the surface of the spray-dried particles is comprised of the hydrophobic shell forming excipient, DSPC (36). The particles also exhibit increases in rugosity (i.e., surface roughness) by approximately 4-fold relative to the micronized drug (36). The asperities present on the particle surface help to reduce interparticle cohesive forces and improve the dispersibility of the micronized drug crystals.
Due to the low aqueous solubility of the drug substance (SAPI = 0.07 mg/ml) and high dose of the ciprofloxacin DPI drug product (32.5 mg), the percentage of drug dissolved in the feed is low (~ 0.3%). As a result, the crystallinity of the drug substance is likely maintained during spray-drying and storage. Of the impurities listed in the USP and Eur. Pharmacopeia for ciprofloxacin, only impurities A, B, C, and D are observed, with only impurity C being a known degradant. The ciprofloxacin DPI drug product is remarkably stable, with no impurities exceeding 0.1% w/w observed following storage at 25°C/60% RH over a period of 5 years (36,40). As well, no significant changes in the physical form of the drug substance, or in aerosol performance (emitted dose, mass median aerodynamic diameter, and fine particle dose < 4.5 μm) were observed over this period (36).
As with solution-based spray-dried formulations, the desired micromeritic properties in the spray-dried drug product afforded by the suspension-based spray-drying process improve lung targeting and dose consistency relative to that observed with current marketed DPI formulations. A pharmacoscintigraphy study was conducted with ciprofloxacin DPI in heathy volunteers, in patients with COPD and in patients with bronchiectasis (N = 6 subjects per group) (42). The mean emitted dose of ciprofloxacin from the T-326 DPI across the three groups ranged from 93 to 95% of the nominal dose, while the total lung dose (TLD) ranged from 51 to 53%. The in vivo variability in the TLD was low compared to most marketed inhaled therapeutics, ranging from 14 to 25%. The in vivo deposition results obtained by gamma scintigraphy correlate well with in vitro testing conducted in the Alberta idealized throat (AIT) model (36). The dependence of the TLD on inspiratory flow rate or pressure drop can be determined from a quantitative metric termed the Q index (21). The Q index represents the normalized difference in TLD determined between pressure drops of 1 kPa and 6 kPa. This range of pressure drops encompasses what most subjects achieve when inhaling comfortably through dry powder inhalers. Drug products with a Q index > 40% are deemed to have a high flow rate dependence: those with 40% > Q index > 15%, medium flow rate dependence; and those with a Q index < 15%, low flow rate dependence. As a class, spheronized particles typically exhibit a high flow rate dependence, lactose blends have a medium flow rate dependence, and spray-dried porous particles, a low flow rate dependence. Based on AIT data, ciprofloxacin DPI has a measured Q index of − 12.2%, indicative of a low flow rate dependence and consistent with other porous particle formulations (21,43).
The excellent safety and tolerability profile observed with ciprofloxacin DPI has been established across more than seven clinical studies in multiple patient populations (36,41,42,44,45,46,47). The primary treatment-emergent adverse events observed with ciprofloxacin DPI are abnormal taste (dysgeusia) and post-inhalation cough. In phase 3 trials in 933 bronchiectasis patients, post-inhalation cough was observed in just 6.4% of the patients, with no difference between the treatment groups (14-day versus 28-day on-off treatment regimens) and the pooled data for PulmoSphere placebo (47). Post-inhalation cough was also low in a phase 2 study in 286 cystic fibrosis patients (3.2% for a 32.5-mg dose and 2.2% for a 48.75-mg dose) (45). The assertion that cough is an inherent property associated with high dose delivery of dry powders (48,49) is clearly not a generalizable statement; additional data are needed to better understand the factors that influence post-inhalation cough. In a meta-analysis of inhaled antibiotics for patients with stable bronchiectasis, inhaled aminoglycosides significantly increased the risk of bronchospasm (risk ratio [RR] 4.78, p = 0.007), whereas inhaled ciprofloxacin (RR 1.07, p = 0.93) did not (36). Bronchospasm was observed in just 3.2% patients in the phase 2 study (N = 93) (46) and 3.9% of patients in the phase 3 study (N = 622 treated patients) (47).
Budesonide Inhalation Powder
The inhaled corticosteroid budesonide is practically insoluble in water (SAPI = 0.011 mg/ml). For a ~ 0.1-mg nominal dose, the %Dissolved is expected to be about 0.9% w/w (Eq. 2). A clinical pharmacoscintigraphy study was conducted in ten healthy volunteers with a suspension-based PulmoSphere formulation of budesonide administered with the Eclipse® dry powder inhaler (35). The dependence of TLD on inspiratory flow rate was explored in a crossover design where subjects were instructed to perform “forceful” and “comfortable” inhalations on separate visits. An in vivo TLD of 58% of the nominal dose (67% of the emitted dose) was observed following oral inhalation, with the TLD independent of inspiratory effort (i.e., the slope of a plot of TLD vs. flow rate was not significantly different from zero). The Q index based on the in vivo deposition results was just + 1.6% (21,35). These results are in contrast to what is observed for budesonide delivery with the Pulmicort® Turbuhaler® (AstraZeneca), where the TLD is 27.7% at a flow rate of 60 L/min and 14.8% at a flow rate of 35 L/min. This is an extremely high flow rate dependence, Q index = + 76.7% (21,50).
Regional deposition within the respiratory tract is especially important with inhaled corticosteroids as drug deposition in the upper respiratory tract (URT) can lead to dysphonia and opportunistic infections (e.g., candidiasis and descending pneumonia). URT deposition with the budesonide PulmoSphere formulation was just 29% of the nominal dose as compared to 58 to 71% with Pulmicort Turbuhaler (35,50). More effectively bypassing deposition in the URT also leads to decreases in interpatient variability associated with the TLD (35). For the spray-dried budesonide formulation, the variability associated with oropharyngeal filtering of particles was just 12%.
The suspension-based PulmoSphere formulation also exhibits uniform deposition in the central, intermediate, and peripheral regions of the lungs (i.e., 17.6%, 20.3%, and 19.5%, respectively) (35).
Amphotericin B Inhalation Powder (ABIP)
A suspension-based PulmoSphere formulation of the antifungal amphotericin B (AmB) has been advanced to end-of-phase 2 meetings with Health Authorities. The drug is indicated for the prophylaxis of immunocompromised patients susceptible to invasive pulmonary aspergillosis (IPA). Unfortunately, this project stalled after the 2009 acquisition of Nektar Therapeutics’ pulmonary business unit by Novartis.
The practically insoluble AmB molecule (SAPI ~ 1 μg/ml) has a %Dissolved in the amphotericin B inhalation powder (ABIP) liquid feed of ~ 0.0008%, making it an ideal candidate for the suspension-based manufacturing process. Size reduction of AmB crystals to X50 of about 1 μm was achieved in an aqueous suspension via high pressure homogenization. Spray-drying of the suspended AmB crystals in the PulmoSphere emulsion feed at a drug loading of 50% w/w yields “coated crystals” (Fig. 1d), with X50 of ~ 1.8 μm and X90 of ~ 3.6 μm (31).
The preferred dosing regimen for ABIP involves an initial loading dose of 50 mg, followed by administration of a 10-mg nominal dose once weekly with the T-326 DPI (Fig. 2). The once weekly dosing is thought to result from the slow clearance of the poorly soluble AmB molecule from the lungs and its propensity to bind to sterols present in the pulmonary epithelium. This treatment regimen enables maintenance of trough levels of AmB in the lungs that are about 10-fold greater than the minimum inhibitory concentration (MIC) of various strains of Aspergillus spp. (51,52). The high levels of AmB in lung tissue are achieved with low corresponding exposures in the systemic circulation. Peak AmB concentrations in plasma observed clinically are nearly two orders of magnitude below the threshold for systemic toxicity (51,52). As a result, ABIP is well tolerated with none of the debilitating systemic side effects (e.g., fever, shaking, chills, flushing, dizziness, diarrhea, vomiting) characteristic of parenteral AmB formulations.
The influence of the size of the AmB drug crystals on the aerodynamic size of the suspension-based PulmoSphere particles is illustrated in Fig. 3a. The FPD< 3.3 μm decreases by about 2-fold with increases in AmB crystal size from about 1 μm to 3 μm (31).
Aerodynamic performance of amphotericin B inhalation powder (ABIP) emitted from the T-326 DPI (fill mass = 10 mg). a Correlation between the primary particle size distribution of AmB drug microcrystals (X50) with the aerosol performance (FPD< 3.3 μm) of the resulting spray-dried particles (nominal AmB dose = 5 mg) (32). b Emitted powder mass of ABIP as a function of inhaled volume and flow rate. c Aerodynamic particle size distributions of ABIP as a function of different inhalation conditions (inhaled volume and flow rate)
For the phase 3 ready ABIP formulation and process, the emitted powder mass with the T-326 DPI was found to be independent of variations in flow rate and inhaled volume, with a grand mean emitted powder mass across all test conditions of 96 ± 3% (Fig. 3b) (21). At a flow rate of 60 L/min in a Next Generation Impactor, the MMAD was 2.3 μm, with an FPD< 4.5 μm of 83% (representing the stage grouping from stage 3 to filter), and an FPD< 2.8 μm (representing the stage grouping from stage 4 to filter) of 58% of the nominal dose. Drug delivery was also independent of inspiratory flow rate with a Q index of just + 1.3% (Fig. 3c) (21).
PA-1806
PA-1806 is a catechol-containing monobactam antibiotic with activity against Gram negative bacteria including Pseudomonas aeruginosa (53). It is poorly soluble in water (SAPI = 0.14 mg/ml). PA-1806 provides an excellent example of the advantage that maintaining drug crystallinity can have on chemical stability of a spray-dried drug product. Table I provides a comparison of three PA-1806 formulations: a lyophilized powder formulated with a glass-forming excipient, a solution-based PulmoSphere powder (via in-situ salt formation with an acid to increase aqueous solubility), and a suspension-based PulmoSphere powder.
The lyophilized powder and the solution-based PulmoSphere powder comprise drug in amorphous form, while for the suspension-based PulmoSphere powder, the drug is in crystalline form. The lyophilized powder shows an increase in total impurities by 2.5% following storage for 3 months at 40°C/75%RH. The solution-based PulmoSphere powder is highly unstable with a nearly 14% increase in degradants in the first month of storage at 40°C/75%RH. It should be noted that the base PulmoSphere excipients are shell-formers that are present in a separate phase from the drug; they do not contribute to stabilization of an amorphous solid, as is possible with formulations comprising glass-forming excipients and buffers. As such, PA-1806 is an unsuitable candidate for formulation with the solution-based PulmoSphere manufacturing process. Nonetheless, excellent stability with negligible chemical degradation following 3 months storage at 40°C/75%RH was achieved when the crystallinity of the drug was maintained (Table I). The same trend in drug stability was observed regardless of whether the drug product was packaged in blistered capsules or in capsules with no primary packaging.
This suspension-based PulmoSphere powder has a high drug loading (67% w/w), resulting in a powder resembling phospholipid-coated crystals. This is borne out when comparing the primary particle sizes (X50) of the drug crystals and the formulated powder, which are 1.5 μm and 2.2 μm, respectively (54). The aerosol performance of the suspension-based PulmoSphere powder of PA-1806 administered with the Turbospin® DPI at a flow rate of 60 L/min was also maintained under the accelerated stability conditions studied, as indicated by the lack of change in ED, MMAD, and FPD< 3.3 μm (Table I) (54).
SPRAY BLENDING
The previous examples have involved practically insoluble drugs (ciprofloxacin, budesonide, amphotericin B, and PA-1806), which will tend to result in a low %Dissolved in aqueous-based feeds. In contrast, many drugs have a non-negligible solubility in an aqueous-based feed. As a consequence, such drugs are prone to having a mixture of crystalline and amorphous drug in the spray-dried drug product. This is undesirable not only because of the challenges associated with physicochemical stability of the amorphous form but also because of possible regulatory requirements to control the amorphous content over a narrow range, either through manufacturing controls or analytics or both. Complexity in development is greatly reduced when the drug can be made either completely amorphous or crystalline. As such, it became critical to develop formulation and process strategies to limit the degree of drug dissolution so as to prevent formation of disordered material. The remainder of this manuscript will detail some possible solutions to this problem, which enable maintenance of crystal form during spray drying, even for materials that are soluble in water.
One way to reduce %Dissolved in suspension-based feeds is to utilize a novel process termed “spray blending” (38,39). Spray blending employs a custom atomizer that contains multiple twin-fluid nozzles with non-interacting plumes (e.g., the “Hydra” atomizer detailed in Fig. 4) (39). Each nozzle can be operated independently, using a different feed composition and liquid flow rate. To prevent amorphous drug formation, one nozzle utilizes a feed comprising micronized drug particles and PulmoSphere excipients at a sufficient drug loading to reduce drug dissolution (i.e., large increases in XAPI in Eq. 1), while the remaining nozzles typically use a common feed that contains only excipients. During the drying process, the blending of the two types of powder particles occurs “one particle at a time” in a single-step particle creation and blending process. As a result, the spray-blending process leads to highly uniform powder blends of micron-sized particles, an outcome that can be difficult to achieve with standard low-shear and high-shear blending equipment (38,39). This process ensures that the final, spray-blended drug product has the required drug loading to achieve the target nominal dose, while simultaneously preventing significant dissolution of drug.
Impact of spray blending on the chemical stability of a dry powder formulation of a prostacyclin analog, QCC374. The left panel shows the Hydra atomizer comprising five independent twin-fluid nozzles. The middle panel shows the process strategy for spray blending using five nozzles. The right panel shows the impact of spray blending on reducing the percentage of drug dissolved in the feed and its subsequent impact on chemical stability following storage of blistered capsules at 40°C/75%RH (38). Reducing the %Dissolved to less than 0.1% w/w effectively slows QCC374 degradation
One challenge with any blended product is that blend uniformity can be lost over time due to particle segregation. This is especially a concern for formulations of highly potent drugs. In spray-blended powders, the size of the particles and their surface characteristics are controlled by the shell-forming excipient, which are similar for the particles with and without drug. As such, spray blends have little tendency for particle segregation during filling or on storage (38,39).
QCC374
The utility of the spray blending process is detailed below for a novel prostacyclin analog that is in phase 2 clinical development for the treatment of pulmonary arterial hypertension (PAH) (55). The free base form of the drug has a solubility of just 0.01 mg/ml (38). However, the drug is highly potent with an anticipated nominal dose less than 0.1 mg (55). Assuming a capsule fill mass of 3 mg, this leads to a target drug loading of less than 0.033 w/w and a %Dissolved of ~ 1% w/v. While this does not seem like a high amount of drug dissolution, in this case it has a profound impact on the stability of the drug substance in the formulated drug product (Fig. 4). Even with just 1% drug dissolution, more than 3% chemical degradation was observed following storage for 1 month at 40°C/75% RH (38).
To maintain the physical form of the prostacyclin analog, a spray blending process was developed wherein particles with a higher drug loading (XAPI up to 0.4 w/w to limit drug dissolution) were blended with PulmoSphere placebo particles containing a 2:1 mol:mol ratio of DSPC:CaCl2 (20,38). The final spray-blended formulations had an XAPI = 0.025 w/w, which for a 3-mg fill mass yields a nominal dose of 0.075 mg. Formulations with various amounts of %Dissolved were prepared on a Niro PSD-1 scale spray dryer. Following storage for 4 weeks at 40°C/75% RH, the total degradation was less than 0.35% for all of the spray blends tested (38). For formulations where the feed contained drug at a 0.4 w/w drug loading (%Dissolved = 0.075% w/v), the total degradation was less than 0.20%. Importantly, there was no difference in degradation between the 2-week and 4-week stability samples for formulations with %Dissolved < 0.1% w/v (circled), and the degradation was comparable to that observed in the non-formulated crystalline drug substance. Hence, the spray blending process was effective in reducing the %Dissolved and in minimizing chemical degradation issues associated with the suspension-based QCC374 drug product.
Indacaterol Maleate
The long-acting beta-agonist indacaterol maleate is very slightly soluble in water and has a low nominal dose (0.075 to 0.30 mg), factors that lead to significant drug dissolution in aqueous feeds. The %Dissolved can be as high as ~ 20% w/v for a 0.075-mg dose (Eq. 2) (38,39). This results in a moderate amorphous content, which can negatively impact the chemical stability of indacaterol (38,39). Indeed, accelerated stability at 60°C, over a period of 1 week for a formulation containing a %Dissolved of about 20%, resulted in a “forest of peaks” when assessed by high performance liquid chromatography.
According to Eq. 1, %Dissolved can be reduced by decreasing SAPI or by increasing Csolids or XAPI. One approach to reduce the solubility of the salt form of the drug (SAPI) is to take advantage of the common ion effect. This can be predicted by Le Chatelier’s principle—the addition of a common ion shifts the equilibrium between a salt and its dissociated components towards the undissociated form. This can dramatically reduce SAPI and, as a result, reduce the %Dissolved and amorphous content in the spray-dried powder. For example, the addition of 20 mM sodium maleate (i.e., a common ion for indacaterol maleate) into the liquid feed reduces the aqueous solubility of indacaterol maleate by 20-fold to ~ 0.1 mg/ml, thereby lowering the %Dissolved to ~ 1% w/v (38,39). The %Dissolved of salt forms of drugs can also be modified by altering the pH (i.e., addition of a buffering agent) or by changing the counterion species.
The %Dissolved of indacaterol maleate can be further reduced with spray blending. In the example below, a suspension of micronized indacaterol maleate particles at a drug loading up to 0.18 w/w in an emulsion-based feed was atomized from one nozzle, and spray-blended with excipient-only PulmoSphere feeds from two additional nozzles to arrive at a final drug loading of 0.041 w/w. Overall, the combination of a common ion and spray blending reduced the %Dissolved by approximately two orders of magnitude to ~ 0.2% w/v. This improved the chemical stability (i.e., reduced enantiomer and total impurity formation) of the spray-blended dry powder under accelerated stability conditions (T = 60°C for 7 days) (Fig. 5) (38,39). At standard room temperature storage conditions of 25°C/60% RH, no significant indacaterol degradation was observed with the spray blends over a period of 9 months, with the principal chemical degradation products all present below their limit of quantitation (< 0.05%) (38). The enantiomer content was also low and comparable to levels observed in the incoming drug substance (0.30%) (38).
A clinical study with a spray-dried indacaterol maleate PulmoSphere formulation administered to asthma patients with the Concept1 dry powder inhaler demonstrated that comparable bronchodilation could be achieved with the spray-dried formulation at about half the current marketed dose (ca., 0.0375 mg) (56). This is driven by a doubling of the in vivo TLD from 34% w/w of the nominal dose for the marketed lactose blend to ~ 65–70% w/w with the spray-dried formulation (56). The doubling of the TLD was achieved primarily via reductions in the percentage of drug depositing in the device and oropharynx, and not by a significant reduction in the aerodynamic size of the respirable dry powder particles, as the APSD post-throat was comparable for the lactose blend and PulmoSphere formulations (56).
Excellent in vitro–in vivo correlations (IVIVC) for TLD were observed for the indacaterol-based formulations with the AIT model (21). Flow rate dependence with the indacaterol PulmoSphere formulation was assessed with the AIT at pressure drops between 1 and 6 kPa. The measured Q index was − 14.6%, again indicative of the low flow rate dependence observed with spray-dried porous particles (21,56).
Spray Blends of FDC
The previous examples have illustrated multiple approaches to reduce drug dissolution in suspension-based feeds. While, in principle, these approaches can be extended to fixed dose combinations (FDC), formulation becomes more complex when there are two or more drugs in a liquid feed. Oftentimes, each drug will have different requirements. For example, the pH requirements for optimal chemical stability of two drugs may differ, or the need for a common ion to prevent dissolution may differ for different drugs. And, in some cases, two drugs might be chemically incompatible when co-formulating them in a single particle. In such cases, spray blending with a multi-headed atomizer provides an option for overcoming challenges in FDCs by enabling control of the chemical milieu separately for each drug.
Formulation of FDCs in a spray blend can also overcome “co-formulation effects” often observed in lactose blends. Co-formulation effects occur when the adhesive force between drug and carrier in the monotherapy differs from that in the FDC due to the presence of a second drug component. This leads to differences in the aerosol performance of the monotherapy relative to the FDC. In contrast, the shell-forming excipients in PulmoSphere particles control the cohesive forces between particles. In spray blends, all of the particles have similar sizes and surface compositions, regardless of the drug formulated in the particle. Hence, no significant co-formulation effects are anticipated.
An example of a fixed dose combination prepared by spray blending is illustrated in Fig. 6 (38,39). In this example, indacaterol maleate (QAB) and the inhaled corticosteroid mometasone furoate (MF) are spray-dried from separate feeds and spray-blended using a Niro PSD-1 scale dryer equipped with a multi-headed spray blending atomizer (38,39).
a Primary particle size distributions and b aerodynamic particle size distributions of spray blends of indacaterol maleate and mometasone furoate (38,39). The APSD of indacaterol (“QAB”) in the mono formulation is provided for comparison. The primary particle size distributions were determined at a dispersing pressure of 4 bar via laser diffraction with a Sympatec HELOS instrument equipped with a VIBRI vibratory feeder and a RODOS dry powder dispersing unit (Sympatec GmbH, Clausthal-Zellerfeld, Germany). Aerodynamic particle size distributions were determined using a Next Generation Impactor (NGI). Aerosols were administered with the Breezhaler® at a flow rate of 60 L/min and an inhaled volume of 2 L. The nominal dose of each drug in the spray blend is 150 μg
The mass median diameter (X50) is ~ 1.0 μm for both micronized drugs. Under this scenario, the primary particle size distributions of the spray blends are controlled by the spray-drying conditions related to droplet atomization, drying, and collection in the spray-dryer and less by the particle size of the drug crystals. As such, the primary particle size distributions of spray blends of indacaterol (monotherapy) and indacaterol/mometasone fixed dose combinations (left panel in Fig. 6) are nearly identical.
Aerodynamic particle size distributions were determined with a Next Generation Impactor (right panel in Fig. 6) (38,39). The MMADs for indacaterol monotherapy, indacaterol (in the FDC), and mometasone (in the FDC) were 2.9, 2.8, and 2.7 μm, respectively. The fine particle fractions on stage 3 to filter in an NGI, (FPFS3-F) corresponding to a cutoff of 4.5 μm, were 70.7, 73.9, and 71.4% of the nominal dose, respectively. The difference in FPFS3-F for the two drugs in the combination relative to indacaterol mono therapy was minimal, i.e., + 4.5% and + 1.0%, respectively. This indicates that no co-formulation effects are observed for the fixed dose combinations in the spray blends.
Following storage at 25°C/60%RH over a period of 9 months, all of the indacaterol and mometasone degradants in the spray blend remained below the limit of quantitation (i.e., < 0.05%), while the measured indacaterol enantiomer content was comparable to that measured for the drug substance (i.e., 0.32%) (38).
CARRIER-BASED FORMULATIONS
Spray blending reduces the %Dissolved of drugs with relatively low water solubilities. There are situations where it may be desirable to maintain the crystallinity of water soluble drugs in a spray drying process. Alternatively, it may be of interest to maintain the crystallinity of multiple drugs with diverse physicochemical properties for formulation in a fixed dose combination. One process option to achieve this end is to spray dry a suspension of micronized drug(s) and small porous carrier particles (median diameter = 2 to 3 μm) from a liquid non-solvent (57,58). For PulmoSphere formulations, this is referred to as the carrier-based format. Besides their role in diluting the drugs to the required concentration for downstream processing (i.e., filling), the small porous carrier particles form agglomerates with the micronized drug particles. In contrast to standard lactose blends comprising coarse carrier particles, the agglomerates remain of a “respirable size” for efficient delivery to the lungs with a portable dry powder inhaler (57,58).
Preferred non-solvents include perfluorinated oils (e.g., perfluorooctyl bromide, PFOB) and semi-fluorinated alkanes (e.g., perfluorooctyl ethane) (57,58). Most drugs are insoluble in these liquids, yet hydrophobic drug particles and shell-forming excipients can be effectively dispersed within them (20,59). Furthermore, the process aid helps to facilitate adsorption of the drug to the carrier, as the drug prefers to minimize its surface area in contact with the fluorinated medium, in much the same way as foods tend to not adsorb/stick to Teflon®-coated pans.
Triple Combinations of LABA/LAMA/ICS
The potential of the carrier-based PulmoSphere technology is illustrated below for a fixed dose combination of a long-acting beta-agonist (LABA), a long-acting muscarinic antagonist (LAMA), and an inhaled corticosteroid (ICS) (57,58). The three drugs have diverse physicochemical properties, with differences in aqueous solubility that span five orders of magnitude, and differences in lipophilicity, as given by their octanol-water partition coefficient (log P), that span about six orders of magnitude (Table II).
Respirable agglomerate formulations comprising micronized particles of indacaterol acetate (QAB), mometasone furoate (MF), and glycopyrronium bromide (NVA) were prepared in two discrete spray-drying steps. In the first step, standard PulmoSphere placebo particles were prepared via spray drying an emulsion-based feedstock (20,57). In the second step, ~ 20% w/v of the small porous PulmoSphere placebo particles was dispersed with a high-shear mixer in PFOB, to form a homogeneous suspension. The term “homodispersion” has been coined to describe these unique suspensions, where their porous morphology and hydrophobic surface composition significantly reduces interparticle attractive forces (59). Furthermore, the filling of the pores of the particles with PFOB results in a closely matched density between the suspended particles and the medium, which reduces settling and/or creaming rates. Micronized drug particles (up to ~ 6% w/v) were then added to the homodispersion of small porous carrier particles while mixing. This results in the formation of an adhesive mixture, with micronized drug particles adhered to the surface of the porous carrier particles in the liquid medium (57,58). The non-solvent is then removed in a second spray-drying step, resulting in a dry powder formulation for inhalation (Fig. 7) (58). For a pMDI delivery system, the volatile non-solvent (i.e., the propellant) is removed (evaporated) at the time of use. To reduce consumption of the non-solvent, the powder formulations are typically prepared by spraying the homodispersion feed from one nozzle and spray blending these particles with an aqueous feed of PulmoSphere placebo excipients from the remaining nozzles. Because no water is involved in the liquid feed, the carrier-based process maintains the salt form and crystallinity of indacaterol acetate. This is critical because indacaterol acetate readily disproportionates to the free base and acetic acid when suspended in water in the suspension-based format (57,58). It also maintains the crystallinity of the glycopyrrolate which, given its high aqueous solubility, would be impossible to accomplish using the suspension-based PulmoSphere format (57,58).
Carrier-based PulmoSphere dry powder formulations comprising micronized drug adhered to small porous phospholipid particles. The left panel is a scanning electron microscopy image showing the colorized drug crystals adhered to PulmoSphere vehicle particles. The right panel shows the aerodynamic particle size distributions of various formulations comprising the inhaled corticosteroid, mometasone furoate. Formulations include the commercial Asmanex® drug product and various mometasone PulmoSphere formulations, including a monotherapy formulation, its fixed dose combination with indacaterol, and a triple combination of mometasone, indacaterol, and glycopyrrolate. Aerodynamic particle size distributions of the PulmoSphere formulations were determined with the Concept1 dry powder inhaler at a flow rate of 60 L/min and an inhaled volume of 2 L (58) (Reproduced with permission from Virginia Commonwealth University (2015))
Content uniformity of the carrier-based PulmoSphere formulations was assessed by measurement of the content of each of the three drugs in the spray-dried powders following filling into capsules with a drum filler. Capsules were sampled at the beginning, middle and end of the filling process. The variability in content of each drug was comparable to the variability observed in the filling process (2.4%). The variability in the content of indacaterol, mometasone, and glycopyrronium were 1.9%, 2.1%, and 2.9%, respectively, with excellent uniformity across the batch.
In contrast to standard lactose blends where a large number of micronized drug particles are adhered to a single large, carrier particle, the number of low-density porous carrier particles in the carrier-based PulmoSphere formulations far exceeds the number of drug particles. In this scenario the binding of one drug to a carrier particle likely has little impact on the binding of a subsequent drug particle to a carrier. As such, no co-formulation effects are anticipated (57,58). This is illustrated for MF in the right panel of Fig. 7. The APSD remains consistent, independent of whether the formulation comprises mometasone only, its dual combination with indacaterol, or its triple combination with indacaterol and glycopyrrolate. The fine particle dose less than 4.5 μm varies by less than 3% across the various formulations (63.8% for the mono, 62.5% for the dual combination, and 66.9% for the triple combination). The flow rate dependence for these formulations is generally low with a Q index < 10% (21,58).
Also in contrast to a standard lactose blend, the carrier particles in carrier-based PulmoSphere formulations are respirable. The aerodynamic particle size distribution (APSD) of the respirable agglomerates is intimately linked to the size of the agglomerates and, in particular, to the size of the micronized drug crystals. For example, the size of the glycopyrrolate crystals was significantly larger than the other two drugs (Table II). This results in preferential delivery to the large airways where the muscarinic receptors are located. Note, however, that this decreases the efficiency of delivery to some degree due to increased deposition in the oropharynx (57,58).
METERED DOSE INHALERS
Although this manuscript has focused on dry powders, all three PulmoSphere formats (solution, suspension, and carrier) have also been explored in pressurized metered dose inhalers [60,61,62,63,64]. The PulmoSphere technology as applied to the development of pMDIs for the treatment of asthma and COPD was spun out of Nektar Therapeutics in 2006 as the start-up Pearl Therapeutics (Redwood City, CA).
Early work by the Pearl Therapeutics team focused on the development of a spray-dried formulation of glycopyrronium bromide, using the solution-based PulmoSphere format. Owing to the significant solubility of the amorphous drug in hydrofluoroalkane propellants, the particles rapidly coarsened and crystallized by a molecular diffusion (Ostwald ripening) mediated growth process (64). Due to the high solubility of the drug in water (Table II), suspension-based PulmoSphere formulations were also not feasible. This left only the carrier-based format as a means to produce a spray-dried formulation of crystalline glycopyrronium bromide in hydrofluoroalkane propellants.
According to the original PulmoSphere pMDI patent filed in 1998 by Alliance Pharmaceutical Corp (San Diego, CA) (60): “the perforated microstructures of the present invention may also be used to stabilize dilute suspensions of micronized bioactive agents. The selected bioactive agent(s) may be associated with the perforated microstructures in any form that provides the desired efficacy and is compatible with the chosen production techniques.” In one embodiment, the terms associate or associating means that the “perforated microstructure may adsorb or be coated with the bioactive agent.” The carrier-based format was first reduced to practice in 1999 at Alliance with a phosphodiesterase type-4 inhibitor (PDE4i) that Pfizer had in early development. The PDE4i showed extensive Ostwald ripening of the amorphous drug in hydrofluoroalkane propellants. The Ostwald ripening mediated crystal growth process was effectively mitigated with the carrier-based PulmoSphere format.
At Pearl Therapeutics, the carrier-based PulmoSphere format was also effective in maintaining both the crystallinity of glycopyrronium bromide and the physical stability of the formulated drug product in HFA-134a (64). The carrier-based PulmoSphere formulations of glycopyrronium bromide and its fixed dose combination with formoterol fumarate exhibit the benefits observed with other PulmoSphere pMDI formats (60,61,62,63,64,65,66). This includes the formation of stable suspensions in hydrofluoroalkane propellants that reduce variability associated with the time between shaking the canister and administering the dose (65,66). The formulations also increase the lung delivery efficiencies relative to other suspension pMDI technologies, enabling accurate and precise metering of drugs at low drug contents (as low as ca., 200 ng with glycopyrronium bromide) (65,66). Finally, the carrier-based formulations exhibit no co-formulation effects in fixed dose combinations (65,66).
Pearl Therapeutics was subsequently acquired by AstraZeneca in 2013, after which they re-branded the carrier-based PulmoSphere technology as Aerosphere® co-suspensions, and received Health Authority approval for Bevespi Aerosphere®, its fixed dose LABA/LAMA combination (67). They are currently in late-stage development with a LABA/LAMA/ICS triple combination with budesonide as the ICS component (68).
DISCUSSION
A popular refrain in review articles directed to inhaled drug delivery is that the cost of manufacturing engineered particles significantly exceeds the costs associated with manufacture of adhesive mixtures of micronized drug and lactose carrier particles (69,70). For example, Morton and Barling (69) stated that: “Practicalities of scale and cost have limited the commercial uptake of drug particle engineering techniques.” To date, dry powder formulations of engineered particles have been developed to support new indications, be it systemic delivery of proteins or delivery of antibiotics at doses that are 1000 to 10,000 times higher than asthma therapeutics. As such, direct comparisons of the cost-of-goods (CoGs) of these products relative to traditional formulation technologies are not possible. It is possible, however, to construct a high-level apples-to-apples comparison of the CoGs of potent asthma drugs.
A typical commercial lot size of a lactose blend is between 20 and 50 kg. For spray drying, scale is not a limiting factor, with powder production rates of more than 1 ton/h achievable with commercially available equipment. Indeed, lot sizes comparable to the aforementioned commercial blending operations (i.e., 30 kg) were commercialized in the manufacture of Exubera with a Niro PSD-3 scale spray dryer.
Advances in cyclone design have enabled increased yields for spray-dried powders, particularly for larger lot sizes. For 30 kg lots, it is not uncommon for spray-drying yields to be in excess of 90%. As well, advances in atomizer design have led to the ability to achieve higher solids contents in the liquid feed without compromising the size distribution of the atomized droplets, and, in turn, the size distribution of the spray-dried particles. Hence, solids contents for PulmoSphere feeds are typically 3- to 5-fold higher than was utilized in the production of Exubera, thereby shortening the production time required for spray-drying.
The number of unit operations needed to produce formulated powder is comparable between the two technologies. The production of lactose blends is essentially a two-step process: micronization of the drug substance, followed by sieving/blending of the micronized drug with lactose carrier particles. In some cases, the drug substance and/or the blend requires an additional conditioning/deamorphization step. Solution-based spray-drying is a single-step process. No micronization step is needed, as the drug is dissolved in the liquid feed. For the suspension and carrier-based PulmoSphere formats detailed herein, the complexity of the manufacturing process is similar to that of a lactose blend, as micronization of the drug substance is also required. Compounding of PulmoSphere formulations also requires production of sub-micron emulsion droplets using standard high-pressure homogenization technologies. Overall, the powder production processes do not differ significantly in scale and/or complexity.
The facility requirements and equipment costs are also not expected to differ significantly for the two technologies. Moreover, the number of operators needed to manufacture and release a lot is similar.
The primary difference between commercial lactose blends and spray-dried formulations for delivery of potent molecules lies in a difference in powder fill mass between the two technologies. This is significant, as it defines the number of doses that can be produced per kilogram of powder and ultimately the number of lots needed to service the market. The labor requirements for powder manufacture and release are tied directly to the number of lots required.
The powder fill mass in the capsule-based OnBrez® Breezhaler® drug product (Novartis) is 25 mg. For blister-based products like Advair® Diskus® and Breo® Ellipta® (GSK), the powder fill mass is 12.5 mg (25 mg in total for the dual blisters in Breo Ellipta). The corresponding fill mass for administration of the same drugs in low density spray-dried particles would be between 1 and 3 mg. Hence, an equivalent number of doses require manufacture of up to ten lots of lactose blend for every lot of spray-dried powder.
The lower fill mass requirements for spray-dried powders also decrease the quantity of excipients and process aids required per dose. Indeed, the cost of these materials contributes minimally to the overall product CoGs. For example, if a pore-forming agent like PFOB is used at a volume fraction of 10% v/v, the contribution to the CoGs is only about a penny ($0.01) per dose and can be lowered even further with recycling. The cost of the phospholipid is far less than a penny per dose and can be decreased 3-fold by use of a saturated soy phosphatidylcholine as opposed to synthetic DSPC.
Overall product CoGs for spray-dried asthma therapeutics are expected to be no more than a few pennies per dose, driven mostly by labor costs. Moreover, the CoGs associated with the powder are significantly less than the costs associated with packaging of the drug product or the cost of the delivery device. Hence, suggestions that spray-dried powders have not advanced for delivery of asthma therapeutics because of scale and CoGs issues is simply not accurate. Indeed, such concerns did not slow the development and commercialization of Bevespi Aerosphere.
In the context of high dose delivery, the mass of powder needed to deliver a therapeutic dose becomes a key driver of costs. TOBI Podhaler requires a powder dose of ~ 400 mg daily, i.e., two orders of magnitude greater than for an asthma drug.
One logical assertion is that it may be advantageous to formulate high dose therapeutics as the neat drug, with no added excipients. Moreover, it may also be desirable to utilize the non-ionized (e.g., free base) form of the drug, to avoid the added mass of counterion utilized in salt forms. While these aspirations may be possible in some cases, the intended use and additional constraints imposed by the physicochemical properties of the drug substance often make the use of excipients desirable and, in many cases, necessary. These constraints may be related to physical stability, chemical stability, tolerability, efficacy, and the overall quality of the drug product (e.g., dose consistency) in the hands of patients.
The pulmonary delivery of tobramycin for the treatment of Pseudomonas infections represents an example of the complexity that formulators often face. Utilization of the free base raises potential tolerability concerns related to elevation of the pH in epithelial lining fluid (pKa1 = 9.8), resulting from the high dose and significant buffering capacity afforded by tobramycin’s five amine groups. Solution-based spray drying of tobramycin base to form an amorphous solid also raises concerns with respect to the physical stability of the amorphous solid, which can compromise device use-life and long-term stability. The glass transition temperature (Tg) of the free base at 11.3% RH (RH typical for packaged capsules) is just 67°C for the free base versus 105°C for the sulfate salt (14). Hancock suggested that the Tg should be at least 50°C above the storage temperature to achieve long-term physicochemical stability (71). Hence, the long-term stability of neat formulations comprising amorphous free base may be at risk.
Another potential concern is related to exposure of residual powder left in the device during use at higher RH values. Typically, Tg decreases by about 10–15°C with each 1% of water content (72). Exposure to moderate humidity conditions (e.g., 40%RH) is expected to reduce the Tg of the free base to values well below room temperature. Under these conditions, the water would plasticize the residual powder in the device. This ultimately leads to viscous flow and “stickiness,” related phenomena that are common to amorphous organic materials stored or handled above Tg. This can negatively impact capsule precession and device performance. This is mitigated in TOBI Podhaler by the higher Tg of the sulfate salt (14,15), by specific design features in the device (73), and by the 1-week use life of the Podhaler device. Hence, the use of the salt form of tobramycin may be important in maintaining the physical stability and tolerability of the formulated drug product.
The use of shell-forming excipients is also important for improving lung targeting and dose consistency in these products, as demonstrated in the present review. For TOBI Podhaler, achievement of > 60% total lung dose independent of patient breathing profile was considered to be worth the added 15% mass associated with the addition of the shell-forming excipients (16). These benefits have yet to be demonstrated for formulations comprising neat drug.
CONCLUSIONS
The present review has described numerous formulation and engineering solutions designed to reduce dissolution of drug molecules in liquid feeds to be spray dried. Maintaining the crystalline form improves the physical and chemical stability of the formulated dry powder for inhalation. The suspension-based and carrier-based PulmoSphere formats enable improvements in lung targeting and dose consistency with a portable inhaler over doses ranging from ca., 100 ng to 100 mg, independent of the physicochemical properties of the drug. Total lung deposition on the order of 50–80% of the nominal dose is readily achievable with minimal dependence on the patient’s inspiratory flow profile. The formulation and spray-drying strategies detailed here also enable formulation of fixed dose combinations of drugs with diverse physicochemical properties with no co-formulation effects.
The examples detailed herein have utilized three different formats of the PulmoSphere technology. In this regard, the same excipients (DSPC, CaCl2) and process aids (PFOB, water) were used throughout. Nonetheless, dramatic differences in physical and chemical stabilities of the incorporated drug are observed, conclusively illustrating that how one combines materials within a formulation and manufacturing process does indeed matter!
References
Snyder HE, Lechuga-Ballesteros D. Spray drying: theory and pharmaceutical applications. In: Augsburger LL, Hoag SW, editors. Pharmaceutical dosage forms: tablets, volume 1: unit operations and mechanical properties. New York: Informa Healthcare; 2008. p. 227–60.
Vehring R, Foss WR, Lechuga-Ballesteros D. Particle formation in spray drying. J Aerosol Sci. 2007;8:728–46.
Vehring R. Pharmaceutical particle engineering via spray drying. Pharm Res. 2008;25:999–1022.
Edwards DA, Hanes J, Caponetti G, Hrkach J, Ben-Jebria A, Eskew M-L, et al. Large porous particles for pulmonary drug delivery. Science. 1997;276:1868–72.
Lipp MM, Batycky R, Moore J, Leinonen M, Freed MI. Preclinical and clinical assessment of inhaled levodopa for off-episodes in Parkinson’s disease. Sci Transl Med. 2016;8:360ra136.
Lord JD. AeroVanc: a novel dry powder inhaler for the treatment of methicillin-resistant Staphylococcus aureus infection in cystic fibrosis patients. Proc Respir Drug Deliv 2014. 2014;3:563–8.
Adi H, Young PM, Chan H-K, Stewart P, Agus H, Traini D. Co-spray dried antibiotics for dry powder lung delivery. J Pharm Sci. 2008;97:3356–66.
Rabbani NR, Seville PC. The influence of formulation components on the aerosolization properties of spray-dried powders. J Control Release. 2005;110:130–40.
Shoyele SA, Cawthorne S. Particle engineering techniques for inhaled biopharmaceuticals. Adv Drug Deliv Rev. 2006;58:1009–29.
Healy AM, Amaro MI, Paluch KJ, Tajber L. Dry powders for oral inhalation free of lactose carrier particles. Adv Drug Deliv Rev. 2014;75:32–52.
Stevenson C, Bennett D. Development of Exubera® insulin pulmonary delivery system. In: das Neves J, Sarmento B, editors. Mucosal delivery of biopharmaceuticals. New York: Springer Science; 2014. Chapter 21.
Geller D, Weers J, Heuerding S. Development of a dry powder formulation of tobramycin using PulmoSphere technology. J Aerosol Med Pulm Drug Del. 2011;24:175–82.
Sadrzadeh N, Miller DP, Lechuga-Ballesteros D, Harper NJ, Stevenson CL, Bennett DB. Solid-state stability of spray-dried insulin powder for inhalation: chemical kinetics and structural relaxation modeling of Exubera above and below the glass transition temperature. J Pharm Sci. 2010;99:3698–710.
Miller DP, Tan T, Tarara T, Nakamura J, Malcolmson R, Weers J. Physical characterization of tobramycin inhalation powder I: rational design of a stable engineered-particle formulation for delivery to the lungs. Mol Pharm. 2015;12:2582–93.
Miller D, Tan T, Nakamura J, Malcolmson R, Tarara T, Weers J. Physical characterization of tobramycin inhalation powder II. State diagram of an amorphous engineered particle formulation. Mol Pharm. 2017;14:1950–60.
Haynes A, Geller D, Weers J, Ament B, Pavkov R, Malcolmson R, et al. Inhalation of tobramycin using simulated cystic fibrosis patient profiles. Pediatr Pulmonol. 2016;51:1159–67.
Ung KT, Rao N, Weers JG, Huang D, Chan H-K. Design of spray-dried insulin microparticles to bypass deposition in the extrathoracic region and maximize total lung dose. Int J Pharm. 2016;511:1070–9.
Ung KT, Weers J, Huang D, Rao N, Son Y-J. Targeted delivery of spray-dried formulations to the lungs. WO 2017/042696 A1. 2017.
Weers JG, Miller DP. Formulation of dry powders for inhalation. J Pharm Sci. 2015;104:3259–88.
Weers JG, Tarara TE. The PulmoSphere™ platform for pulmonary drug delivery. Ther Deliv. 2014;5:277–95.
Weers JG, Clark AR. The impact of inspiratory flow rate on drug delivery to the lungs with dry powder inhalers. Pharm Res. 2017;34:507–28.
Pedersen S. How to use a Rotahaler. Arch Dis Child. 1986;61:11–4.
Li L, Sun S, Parumasivam T, Denman JA, Gegenbach T, Tang P, et al. L-leucine as an excipient against moisture on in vitro aerosolization performance of highly hygroscopic spray-dried powders. Eur J Pharm Biopharm. 2016;102:132–44.
Zhou QT, Gegenbach T, Denman JA, Heidi HY, Yi J, Chan H-K. Synergistic antibiotic combination powders of colistin and rifampicin provide high aerosolization efficiency and moisture protection. AAPS J. 2014;16:37–47.
Ahlneck C, Zografi G. The molecular basis for moisture effects on the physical and chemical stability of drugs in the solid-state. Int J Pharm. 1990;62:87–95.
Kumar S, Shen J, Zolnik B, Sadrieh N, Burgess DJ. Optimization and dissolution performance of spray-dried naproxen nano-crystals. Int J Pharm. 2015;486:159–66.
Barot BS, Parejiya PB, Patel TM, Parikh RK, Gohel MC. Development of directly compressible metformin hydrochloride by the spray-drying technique. Acta Pharma. 2010;60:165–75.
Miller DP, Huang D, Rao N, Weers JG. Highly dispersible powders comprising inorganic salts. Proc Respir Drug Deliv. 2016;2:471–5.
Selby MD, de Koning PD, Roberts DF. A perspective on synthetic and solid-form enablement of inhalation candidates. Future Med Chem. 2011;3:1679–701.
Yeadon M. The paradox of respiratory R&D, and why ‘inhaled-by-design’ heralds a new dawn in asthma and chronic obstructive pulmonary disease treatments. Future Med Chem. 2011;3:1581–3.
Weers JG. Enhanced design of inhaled therapeutics: what does the future hold? Ther Deliv. 2016;7:145–8.
Weers JG, Tarara T, Malcolmson R, Leung D. Embedded crystals in low density particles: formulation, manufacture, and properties. Proc Respir Drug Deliv X. 2006;2:296–304.
Faithfull NS, Weers JG. Partial liquid breathing of fluorochemicals. US Patent 5,490,498, 1996.
Dickson EW, Heard SO, Tarara TE, Weers JG, Brueggemann AB, Doern GV. Liquid ventilation with perflubron in the treatment of rats with Pneumococcal pneumonia. Crit Care Med. 2002;30:393–5.
Ivey JW, Vehring R. The use of modeling in spray drying of emulsions and suspensions accelerates formulation and process development. Comp Chem Eng. 2010;34:1036–40.
Duddu SP, Sisk SA, Walter YH, Tarara TE, Trimble K, Clark AR, et al. Improved lung delivery from a passive dry powder inhaler using an engineered PulmoSphere powder. Pharm Res. 2002;19:689–95.
McShane PJ, Weers JG, Tarara TE, Haynes A, Durbha P, Miller DP, et al. Ciprofloxacin dry powder for inhalation (Ciprofloxacin DPI): technical design and features of an efficient drug-device combination. Pulm Pharmacol Ther. 2018;50:72–9.
Weers J, Huang D, Tarara TE, Miller D. Deamorphization of spray-dried formulations via spray blending. US Patent 2015/0374623 A1. 2015.
Weers JG, Huang D, Tarara TE, Miller DP. Deamorphization of spray-dried formulations via spray blending. Proc Respir Drug Deliv. 2016;3:481–4.
Weers J, Tarara T. Pulmonary delivery of a fluoroquinolone. US Patent 8,834,930. 2014.
Stass H, Delesen H, Nagelschmitz J, Staab D. Safety and pharmacokinetics of ciprofloxacin dry powder for inhalation in cystic fibrosis: a phase I, randomized, single-dose, dose-escalation study. J Aerosol Med Pulm Drug Deliv. 2015;28:106–15.
Stass H, Nagelschmitz J, Kappeler D, Sommerer K, Kietzig C, Weimann B. Ciprofloxacin dry powder for inhalation in patients with non-cystic fibrosis bronchiectasis or chronic obstructive pulmonary disease and in healthy volunteers. J Aerosol Med Pulm Drug Deliv. 2017;30:53–63.
Haynes A, Mundry T, Durbha P, Miller DP, Tarara T, Malcolmson R, et al. Design of ciprofloxacin dry powder for inhalation. Proc Respir Drug Deliv 2016. 2016;3:455–8.
Stass H, Nagelschmitz J, Willmann S, Delesen H, Gupta A, Baumann S. Inhalation of a dry powder ciprofloxacin formulation in healthy subjects: a phase 1 study. Clin Drug Invest. 2013;33:419–27.
Dorkin HL, Staab D, Operschall E, Alder J, Criollo M. Ciprofloxacin DPI: a randomized placebo-controlled, phase IIb efficacy and safety study on cystic fibrosis. BMJ Open Respir Res. 2015;2:e000100. https://doi.org/10.1136/bmjresp-2015-000100/2:e000100.
Wilson R, Welte T, Polverino E, De Soyza A, Greville H, O’Donnell A, et al. Ciprofloxacin dry powder for inhalation in non-cystic fibrosis bronchiectasis: a phase II randomized study. Eur Respir J. 2013;41:1107–15.
Ciprofloxacin DPI (BAY q3939). In: Briefing document for FDA Advisory Committee Meeting on 16 Nov 2017, NDA 209367. https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/Anti-InfectiveDrugsAdvisoryCommittee/UCM584651.pdf. Accessed 07 Sep 2018.
Young PM. High dose powders: a critical assessment of needs, formulation, and delivery technologies. Proc Respir Drug Deliv. 2018;1:201–8.
Brunaugh AD, Smyth HDC. Formulation techniques for high dose dry powders. Int J Pharm. 2018:489–98. https://doi.org/10.1016/j.ijpharm.2018.05.036.
Borgström L, Bondesson E, Moren F, Trofast E, Newman SP. Lung deposition of budesonide inhaled via Turbuhaler®: a comparison with terbutaline sulphate in normal subjects. Eur Respir J. 1994;7:69–73.
Kugler AR, Lee JD, Samford LK, Sahner DK, Eldon MA. Clinical pharmacokinetics (PK) following multiple doses of amphotericin B inhalation powder (ABIP). Focus on Fungal Infections (FoFI) 17. 2007: Abstract P-0032, pp. 225–226.
Duddu S, Palakodaty S, Lechuga-Ballesteros, D, Miller D, Kugler AR, Frantz C, Tan T, Malcolmson R, Washco K, Sweeney T, Tarara TE, Dwivedi S, Eldon MA. Compositions comprising amphotericin B, methods and systems. US Patent 7,326,691 B2. 2008.
Schwan WR. Differences in sensitivity of PA-1806 among iron transport mutants of Pseudomonas aeruginosa compared to Escherichia coli. Antimicrob Agents Chemother. 2000;44:3237–8.
Tarara TE, Weers JG. Pharmaceutical formulations with an insoluble active agent. US Patent Application 2004/0156792 A1. 2004.
Safety, pharmacokinetics and efficacy study of QCC374 in PAH patients. Clinical Trial No. NCT02927366. 2017. https://clinicaltrials.gov/ct2/show/NCT02927366. Accessed 07 Sep 2018.
Weers JG, Clark AR, Rao N, Ung K, Khindri SK, Perry SA, et al. In vitro in vivo correlations observed with indacaterol-based formulations delivered with the Concept1 inhaler. J Aerosol Med Pulm Drug Deliv. 2015;28:268–80.
Hartman M, Tarara TE, Teung P, Weers JG: Respirable agglomerates of porous carrier particles and micronized drug. US Patent 9,452,139, 2016.
Weers JG, Tarara T, Teung P, Walsh K, Rao N, Le J, et al. Solving the particle adhesion paradox: respirable agglomerates of micronized drugs and porous (microcarrier) particles. Proc Respir Drug Deliv. 2015;1:177–85.
Weers JG, Tarara TE, Gill H, English BS, Dellamary LA. Homodispersion technology for HFA suspensions: particle engineering to reduce dosing variance. Proc Respir Drug Deliv VII. 2000;1:91–7.
Weers JG, Schutt EG, Dellamary LA, Tarara TE, Kabalnov A. Stabilized preparations for use in metered dose inhalers. US Patent 6,309,623, 2001.
Dellamary LA, Tarara TE, Smith DJ, Woelk CH, Adractas A, Costello M, et al. Hollow porous particles in metered dose inhalers. Pharm Res. 2000;17:168–74.
Hirst PH, Elton RC, Pitcairn GR, Newman SP, Weers JG, Clark AR, et al. In vivo lung deposition of hollow porous particles from a pressurized metered dose inhaler. Pharm Res. 2002;19:258–64.
Tarara TE, Hartman M, Gill H, Kennedy A, Weers JG. Characterization of suspension-based metered dose inhaler formulations comprised of spray-dried budesonide crystals dispersed in HFA-134a. Pharm Res. 2004;21:1607–14.
Vehring R, Lechuga-Ballesteros D, Joshi V, Noga B, Dwivedi SK. Co-suspensions of microcrystals and engineered microparticles for uniform and efficient delivery of respiratory therapeutics from pressurized metered dose inhalers. Langmuir. 2012;28:15015–23.
Doty A, Schroeder J, Vang K, Sommerville M, Taylor M, Flynn B, et al. Drug delivery from an innovative LAMA/LABA delivery technology fixed-dose combination MDI: evidence of consistency, robustness, and reliability. AAPS PharmSci Tech. 2018;19:837–44.
Taylor G, Warren S, Dwivedi S, Sommerville M, Mello L, Orevillo C, et al. Gamma scintigraphic pulmonary deposition study of glycopyrronium/formoterol metered dose inhaler formulated using co-suspension delivery technology. Eur J Pharm Sci. 2018;111:450–7.
Bevespi Aerosphere® package insert. www.bevespi.com. Accessed 07 Sep 2018.
Reisner C, Fernandez C, Darken P, et al. Pearl’s PT010 triple combination provides comparable budesonide exposure to Symbicort and comparable glycopyrronium exposure to PT003. Eur Respir J. 2014;44:1891.
Morton DAV, Barling D. Developing dry powder inhaler formulations. ISAM textbook, Chapter 7.2, www.isam.org/textbook. Accessed 27 Nov 2018.
deBoer AH, Hagedoorn P, Hoppentocht M, Buttini F, Grasmeijer F, Frijlink HW. Dry powder inhalation: past, present and future. Expert Opin Drug Deliv. 2017;14:499–512.
Hancock BC, Shamblin SL, Zografi G. Molecular mobility of amorphous pharmaceutical solids below their glass-transition temperatures. Pharm Res. 1995;12:799–806.
Roos YH. Phase transitions in foods. San Diego: Academic Press; 1995. p. 360.
Maltz DS, Paboojian JS. Device engineering insights into TOBI Podhaler: A development case study of high efficiency powder delivery to cystic fibrosis patients. Proc Respir Drug Deliv Eur. 2011;1:55–66.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guest Editors: Philip J. Kuehl and Stephen W. Stein
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Weers, J.G., Miller, D.P. & Tarara, T.E. Spray-Dried PulmoSphere™ Formulations for Inhalation Comprising Crystalline Drug Particles. AAPS PharmSciTech 20, 103 (2019). https://doi.org/10.1208/s12249-018-1280-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-018-1280-0