ABSTRACT
In a recent food effect clinical study, the authors concluded that a meal consisting of ≥500 kcal, regardless of fat content, produced the maximal bioavailability for ziprasidone. Using GastroPlus™, a commercially available pharmacokinetic simulation software, a semiphysiological model—a kind of physiologically based pharmacokinetic (PBPK) absorption model—was developed that could predict the concentration-time profiles when ziprasidone was administered with any one of the five test meals or fasting. Ziprasidone intravenous pharmacokinetics and oral absorption permeability were determined from clinical studies following the intravenous and duodenal infusion of ziprasidone to volunteers. From the detailed dietary information of each meal provided in the previously published food effect study, the stomach pH, volume, and gastric emptying could be predicted. Incorporating these meal-specific parameters into the model improved the predictions beyond the default fed/fasted parameters commonly used in the software. Compared to the default models, the improved models resulted in an improved prediction of the average ziprasidone concentration-time profile for each meal. Using this type of semiphysiological absorption model, we have shown that the dietary contents of the meals should be taken into account to predict food effects for ziprasidone and perhaps other BCS class I or II compounds.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Food has an important bearing on the absorption of many orally administered drugs (1). For some drugs, absorption is attenuated when taken with food. For others, food enhances absorption. Modification of drug absorption has important implications, not only for efficacy but also for toxicity.
Unexpectedly, low absorption may manifest itself as a reduction in efficacy, while higher drug absorption may result in a greater incidence of adverse events. Either consequence may influence therapeutic success and treatment compliance.
Ziprasidone HCl ((5-[2-(4-(1,2,-benzisothiazol-3-yl) piperazin-l-yl] ethyl]-6-chloro indolin-2-one hydrochloride hydrate) is an orally active antipsychotic drug used for the monotherapy of schizophrenia (2). Because the absolute bioavailability of a 20 mg dose under fed conditions is approximately 60% and because of its low intrinsic solubility (6), the marketed product containing ziprasidone HCl is classified as a Biopharmaceutics Classification System (BCS) class IV, with low solubility drug and borderline low permeability (3). However, from a research perspective, ziprasidone can resemble a drug with high permeability and either low solubility (class II) or high solubility (class I). Studies have shown that the bioavailability of ziprasidone in healthy subjects is enhanced when administered with the Food and Drug Administration (FDA) standard high-fat breakfast (4). However, the food-induced enhancement in ziprasidone bioavailability is short-lived, with a reduced absorption when taken 2 h after, rather than immediately following, food (4). We have recently published a clinical study that examined the impact of calories and fat content on the food-induced enhancement in ziprasidone bioavailability (5). We concluded that ziprasidone should be taken with food that provides at least 500 kcal for optimal bioavailability of 80 mg ziprasidone. Since ziprasidone is highly lipophilic, it is tempting to hypothesize that the positive food effect was a consequence of only an increased solubility, subsequent to biliary secretions of bile salts and lecithin. Using a commercially available software GastroPlus™, we attempted to model these variables in order to understand what additional factor(s) from the meals could have 25 contributed to the food effect for ziprasidone.
MATERIALS AND METHODS
Ziprasidone hydrochloride (HCl) was obtained from Pfizer Inc. (Groton, CT). Ziprasidone is poorly water-soluble (free-base solubility in pH 6.5 buffered media <0.1 mg/mL) (6). The basic pKa of ziprasidone HCl was determined using an automated micro titrator (Model T3, Sirius Analytical Instruments, Beverly, MA)Footnote 1. The fast UV assay was used to determine the pKa. This method consisted of completing potentiometric titrations of methanolic solutions of the active pharmaceutical ingredient (API) and monitoring the effect of ionization on a nearby UV chromophore. The values of the various pKas were then extrapolated using the Yasuda-Shedlovsky method (7, 8). Using the fast UV assay, the basic pKa of ziprasidone HCl determined in 0.15 M KCl was 6.58 ± 0.09. The c log P was reported as 3.6 (6). The pH solubility profile—determined using traditional methods (9)—was provided as an input file (Supplement Table 1). The radii of particle size of a typical lot were given as 10% < 1.89 μ, 50% < 8.23 μ, and 90% < 17.9 μ. A subprogram within GastroPlus™ fitted a log-normal distribution of these parameters to eight bins as an input file for the simulations (Supplement Figure 1). Ziprasidone HCl dissolution was greatly enhanced when the drug partitions into bile salt micelles. The neutral form of the drug had a micelle-to-aqueous partition coefficient of approximately 4000 (10). The bile salt effect in GastroPlus™ followed the following equation: Cs,bile = Cs,aq + Scaq × SR × Mw × [bile], where Scaq was the concentration of ziprasidone HCl at a particular pH, SR was the solubility ratio (4000), Mw was the molecular weight, and [bile] was the concentration of bile acids (11).
The computer modeling software GastroPlus™ (Version 8.5.0002, Simulations Plus, Inc., 45 Lancaster, CA) was used to develop a model that predicts the serum ziprasidone HCl concentrations after each of the six different meals studied in the food effect study. This software has recently been reviewed and summarized (12, 13). Briefly, the gastrointestinal tract in Gastroplus consists of an advanced compartmental absorption and transit model (ACAT). Nine compartments consist of the stomach, small intestine [duodenum, jejunum (two compartments), and ileum (three compartments)], and large intestine (cecum and ascending colon). The physical-chemical property inputs of ziprasidone included solubility, permeability, logP, pKa, particle size, and dose. The dissolution submodel is based on the Nernst-Brunner modification of the Noyes-Whitney equation. For passively absorbed drugs, the absorption—which is a sum of the absorption in the individual compartments—is a function of the concentration of drug in solution for each of the compartments, the surface area for absorption, and the transit of drug along the gastrointestinal tract.
Gastric emptying rates used in this model were estimated based on the relationship proposed by Hunt and Stubbs (14). They demonstrated a simple relationship to predict the effect of meal volume (V 0) and caloric density (K) on gastric emptying rate. The time for 50% emptying (t 50) is given by (14):
The actual calories, grams of protein, fat, and carbohydrates for each test meal, together with beverages administered were used to calculate K and V 0 for each meal. The meal volume (V 0) was calculated by summing the estimated volume of each meal component and adding 240 mL, since ziprasidone HCl was administered with 8 oz. water, for example, for the low calorie/low fat meal 8 oz. milk (240 mL), two slices of toast (50 mL), two pads of butter (50 mL), two packets of jelly (20 mL), with the water totaled 600 mL. Caloric density K was calculated with: kcal/V 0. The values of t 50 based on these parameters for the five meals were calculated. From these values of t 50, the first order rate constant for gastric emptying was then used to simulate the emptying curves. A clinical pharmacokinetic study of ziprasidone HCl following the administration of a single dose of ziprasidone HCl administrated via intravenous infusion vs. infusion into the duodenum had been conducted, and the IV pharmacokinetics and oral absorption permeability were determined from this study. As these data are important for pharmacokinetic modeling, the details of this study and related study results are included in this report (see Supplemental Data).
RESULTS AND DISCUSSION
Intravenous and duodenal administrations of ziprasidone HCl
The serum ziprasidone concentrations in each of seven subjects administered the intravenous infusion of ziprasidone were determined by assay and averaged (Supplement Table 2). The pharmacokinetics from the averaged serum ziprasidone HCl concentrations following intravenous administration were optimized using the Akaike information criterion (15) in the built-in PKPlus™ module (Supplement Fig. 2). The resulting three compartment model pharmacokinetic parameters were exported directly into GastroPlus™ (Supplement Table 3). The serum ziprasidone concentration in each of six subjects administered the nasogastric infusion of ziprasidone HCl into the duodenum was determined by assay and averaged (Supplement Table 4). The permeability of ziprasidone after oral administration was determined in GastroPlus™ by optimizing the effective permeability (Peff) with the average serum ziprasidone concentration-time profile following the infusion into the duodenum. The absorption of ziprasidone in each of the seven small intestinal compartments (duodenum, jejunum 1, jejunum 2, ileum 1, ileum 2, ileum 3) and the two large intestinal compartments (colon 1, colon 2) was determined by the Absorption Scale Factor (ASF) model Opt logD Model SA/V 6.1.Footnote 2 The fasting and fed values of pH and bile salt concentrations for the stomach and intestines in the default GastroPlus™ human physiological models were given in (Supplement Table 5). The nasogastric administration of ziprasidone HCl into the duodenum is not a typical route of administration. The following adjustments were made to simulate this administration: (1) the gastric emptying time (GET) was set to 0.01 h (a minimum value), (2) the duodenum pH was set to 3.5 (pH of the administered solution), (3) the dosage form was set to CR: dispersed, with a zero order release over 20 min (duration of the infusion). The Peff value was 50 cm/s × 104, and the precipitation rate (Tppt) for this controlled infusion into the duodenum was 300 s. This model fit the data well (Supplement Fig. 3).
Food effect study
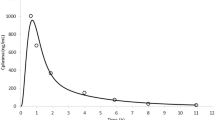
The patients were administered ziprasidone HCl under six different meal conditions in the clinical study (5), as described in Table I: fasted, high calorie/high fat, high calorie/low fat, medium calorie/high fat, low calorie/high fat, and low calorie/low fat. The averaged serum ziprasidone concentration vs. time profiles from fasted volunteers or volunteers following one of 5 meals and 2 weeks of oral administration of 80 mg of ziprasidone HCl every 12 h are shown in Fig. 1 (Table II).
Fasting meal condition
The average concentration-time profile following oral administration of 80 mg ziprasidone HCl in fasting patients was simulated. The GastroPlus™ default values for a capsule of the gastric emptying time (0.1 h), gastric pH (1.3), and Tppt (1 s) were left unchanged (see Supplemental Table 5).
The values of the small intestine water volume (SIWV, 4.5%) and large intestine water volume (0.9%) were set based on published data (16), accounting for the difference in ASF models.Footnote 3 As shown in Fig. 2 and summarized in Table III, the model seemed to predict the average fasting concentration-time profile.
Fed meal conditions
The effect of meals on GI physiology can be described as (1) buffering stomach contents resulting in a slight rise in gastric pH, (2) gastric emptying, (3) an increase in SIWV, and (4) secondary effects such as bile acid secretion (17). The clinical food effect study (5) examined the effect of meal caloric content (high = 1000 kcal, medium = 500 kcal, low = 250 kcal) and fat content (50 and 15% of total calories, Supplemental Table 6) on oral ziprasidone absorption, but the investigators did not control for meal volume. Using the relationship defined by Hunt and Stubbs (14), the values of t 50 for gastric emptying were calculated based on caloric content and meal volume for the five meals. From these values of t 50, the first order rate constant for gastric emptying was then used to simulate the emptying curves summarized in Fig. 3.
High calorie/high fat meal
For the modeling of ziprasidone HCl absorption after the high calorie/high fat meal, the default Human Physiology Fed ACAT Physiology was used, but with a percent fluid in the small intestine set to 10%, and in the colon set to 10%, and the calculated stomach volume of 788 mL (Table IV and Supplemental Table 3). These were calculated for each meal using the stated liquid volumes and estimated fluid displacement of solids. The new model predicted the average data reasonably well (Fig. 4). As shown in Fig. 4, the “default model”—which used 40 and 10% for the small and large intestine, respectively, and 967 mL for the stomach volume—overshot the observed Cmax. The high calorie/high fat meal mimicked the “high fat FDA breakfast” that resulted in the approximately twofold increase in ziprasidone HCl exposure observed in normal volunteers (4). Table III summarizes the fraction of the dose absorbed (Fa) for ziprasidone HCl after this meal (83%). Also in this table are both the observed and simulated pharmacokinetic parameters: Cmax for the maximum serum ziprasidone concentration, Tmax for the time of the Cmax, and AUCτ for the area under the serum ziprasidone concentration vs. time curve in one dosing interval (τ = 12 h).
High calorie/low fat meal
The high calorie/low fat meal consisted of the same 1000 kcal content as the high calorie/high fat meal, but with only 15% calories as fat. Based on the meal content (see below), the stomach pH was set to a slightly smaller value for the high calorie/low fat meal than the high calorie/high fat meal (4.65 vs. 4.9). However, whereas the fat content was considered low—based on the percent calories as fat calories—the total amount of fat (15–16 g) was similar in both high calorie/low fat and the low calorie/high fat meals. Since Festi et al. reported that 10 g of fat was sufficient for gallbladder emptying (18), the default fed concentration of bile acids in the small intestines was used in this simulation. In addition, the high calorie components probably produced nearly the same effect on stomach pH as the high calorie/high fat meal (19–21). Since this meal resulted in the most API absorbed (Fa 89%), increasing the small/large intestine fluid volumes from 10/3 used in this model to 40/10 used in the default fed model did not significantly increase the Fa. As shown in Fig. 5, the new model simulated the observed average concentration-time profile.
Medium calorie/high fat meal
The medium calorie/high fat meal had almost the same magnitude of a positive food effect on apparent ziprasidone bioavailability (RBA 169%), as the previous two meals (172 and 180%, Table III). Since the high fat content of the meal was assumed to stimulate a fed-like secretion of bile salts, the default fed parameters for bile salt concentration were used. The medium calorie content combined with the high fat content probably resulted in a “fed” stomach pH (19–21); therefore, the stomach pH was set to the fed default model value of 4.9. However, because the calorie content was lower than previous meals, the percent fluid volume in the small intestine was set to 5%. This is reasonable, since fat does not contribute to osmolarity and therefore to the meal-induced volume of fluid in the intestine. The new model predicted the observed data reasonably well (Fig. 6). The default fed model—which had the larger fluid volumes for the stomach (967.5 mL)—slightly overpredicted the observed data (Fig. 6).
Low calorie/high fat meal
The food effect of the low calorie/high fat meal was not clinically significant (RBA 122%) (5). Since there was a high fat content in this meal, the “fed” concentrations of bile salt were incorporated and pH was set at 4.75, which seemed reasonable, since the normal pH of “whole milk” was approximately 6.65 (22) (Supplemental Table 6). As shown in Table I and Supplemental Table 6, the low calorie/high fat meal had only 120 kcal that were not from fat. Since fat does not contribute to osmolarity and therefore to the meal-induced volume of fluid in the intestine, the remaining calories would probably not greatly affect the fluid volume values of the small intestine and colon. These values were set to fasted values. The new model provided a reasonably good prediction of the observed average serum ziprasidone concentration-time profile (Fig. 7). The default model using the fed values of small and large intestines of 40 and 10%, respectively, resulted in a 23% overprediction of the Cmax and a 44% overprediction of the AUCτ. The default fasted model resulted in an even worse fit of the data (not shown).
Low calorie/low fat meal
The low calorie/low fat meal did not produce a clinically relevant positive food effect (RBA 112%) (5). When the default fed physiology was used, the default model overestimated the observed concentration-time profile (Fig. 8). Moreover, when the default fasted physiology was used, the model underestimated the average observed Cmax. However, by setting the stomach volume to the actual meal volume and setting the gastric emptying rate to the value calculated from the caloric density, the new model resulted in a better prediction (Fig. 8).
Model prediction of the average ziprasidone concentration-time profile when ziprasidone HCl was administered with the low calorie/low fat meal, using the conditions described in the text. The observed average serum ziprasidone concentrations (triangle), the default model simulation (default fed model, dotted line), and the improved model simulation (continuous line) showed that the improved model better predicts the observed data
Overall, the “new” model using accurate parameter inputs based on data obtained through additional clinical trials as well as accurate gastric emptying models for various meals provided a qualitatively better fit of the ziprasidone absorption profile under various fed states (when compared to using default parameters for fed or fasted states in GastroPlus™). In each case, adjusting for meal volume and utilizing predicted gastric emptying rates for these meals qualitatively improved the model prediction for ziprasidone absorption. This type of modeling approach would likely be useful for BCS classes I (high solubility/high permeability) and II (low solubility/high permeability) compounds where prediction of food effects on absorption can be difficult.
CONCLUSIONS
For many compounds, the GastroPlus™ default parameters for gastric emptying rate, percent volume (for the stomach, small and large intestines), and bile salt concentrations may be suitable to predict food effect concentration-time profiles. However, for ziprasidone and perhaps other BCS class I or II compounds that are sensitive to the effects of these parameters on the food effect, meal-specific values of these parameters can qualitatively improve the concentration-time profile prediction for ziprasidone HCl and perhaps other BCS class I or II compounds.
The FDA guidance on the food effect recommends a high calorie/high fat meal, which is intended to maximally effect the RBA (23). However, the results in this report suggest that slight modifications to the recommended meal may be useful to insure the maximum effect in RBA. It also points to the importance of controlling for meal type and volume when designing a clinical trial for ziprasidone and perhaps for other BCS class I or II compounds.
ACKNOWLEDGEMENTS
This study was sponsored by Pfizer Inc., and all three authors were employees of Pfizer Inc. during the course of these studies. The authors acknowledge the following current or former Pfizer Inc. employees: Lisa Yuhas and Gene Fiese PhD (for determining the physical chemical properties of ziprasidone HCl), Jeffrey Alderman, PhD, Jeffrey J. Miceli, PhD, and Keith Wilner, PhD (for numerous comments and advice on the manuscript), and Drs. William J Curatolo, Timothy Hagen, and Hylar Friedman (for their foresight and encouragement). We also acknowledge the insights of Dr. Brett Caldwell of Bend Research and Simulations Plus, Inc. for the gift of GastroPlus™. The authors also wish to thank the reviewers for their excellent comments and suggestions.
Notes
pKa was determined by SCS at UNE College of Pharmacy.
The ASF models are the best fits of experimental data across a diverse set of compounds (GastroPlus™ Manual, August 2013, Version 8.5, p. 168). The data could also be fitted to the Optimized logD Model by adjusting percent volume in the small and large intestines.
The ASF model used in reference [16] was “Opt logD”, whereas in this work, the model used as “Opt logD Model SA/V 6.1”.
REFERENCES
Welling PG. Effects of food on drug absorption. Annual Review of Nutrition. 1996;16(1):383–415.
Harvey PD, Bowie CR. Ziprasidone: efficacy, tolerability, and emerging data on wide-ranging effectiveness. Expert Opinion on Pharmacotherapy. 2005;6(2):337–46.
Amidon G, Lennernas H, Shah V, Crison J. A theoretical basis for a biopharmaceutic drug classification: correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res. 1995;12:413–20.
Hamelin BA, Allard S, Laplante L, Miceli J, Wilner KD, Tremblay J, Lebel M. The effect of timing of a standard meal on the pharmacokinetics and pharmacodynamics of the novel atypical antipsychotic agent ziprasidone. Pharmacotherapy. 1998;18(1):9–15.
Gandelman K, Alderman JA, Lombardo I, LaBadie RR, Versavel M, Preskorn SH. The impact of calories and fat content of meals on oral ziprasidone absorption: a randomized, open-label, crossover trial. J Clin Psychiatry. 2009;70(1):58–62.
Thombre A, Herbig S, Alderman J. Improved ziprasidone formulations with enhanced bioavailability in the fasted state and a reduced food effect. Pharmaceutical Research. 2011;28(12):3159–70.
Yasuda M. Dissociation constants of some carboxylic acids in mixed aqueous solvents. Bulletin of the Chemical Society of Japan. 1959;32(5):429–32.
Shedlovsky T, Kay RL. The ionization constant of acetic acid in water-methanol mixtures at 25° from conductance measurements. The Journal of Physical Chemistry. 1956;60(2):151–5.
Fiese EF. General pharmaceutics—the new physical pharmacy. J Pharm Sci. 2003;92:1331–42.
Thombre AG, Caldwell WB, Friesen DT, McCray SB, Sutton SC. Solid nanocrystalline dispersions of ziprasidone with enhanced bioavailability in the fasted state. Molecular Pharmaceutics. 2012;9:3526–34.
Mithani SD, Bakatselou V, TenHoor CN, Dressman JB. Estimation of the increase in solubility of drugs as a function of bile salt concentration. Pharmaceutical Research. 1996;13(1):163–7.
Agoram B, Woltosz WS, Bolger MB. Predicting the impact of physiological and biochemical processes on oral drug bioavailability. Advanced Drug Delivery Reviews. 2001;50(Supplement 1):S41–67.
Parrott N, Lukacova V, Fraczkiewicz G, Bolger M. Predicting pharmacokinetics of drugs using physiologically based modeling—application to food effects. The AAPS Journal. 2009;11(1):45–53.
Hunt J, Stubbs D. The volume and energy content of meals as determinants of gastric emptying. J Physiol (Lond). 1975;245:209–25.
Akaike, H. Information theory and the extension of the maximum likelihood principle. in Proceedings of the Second International Symposium on Information Theory. 1973. Budapest Akailseoniai-Kiudo.
Sutton S. Role of physiological intestinal water in oral absorption. The AAPS Journal. 2009;11(2):277–85.
Fleisher D, Li C, Zhou Y, Pao LH, Karim A. Drug, meal and formulation interactions influencing drug absorption after oral administration. Clinical implications. Clin Pharmacokinet. 1999;36:233–54.
Festi D, Colecchia A, Larocca A, Villanova N, Mazzella G, Petroni ML, Romano F, Roda E. Review: low caloric intake and gall-bladder motor function. Alimentary Pharmacology & Therapeutics. 2000;14:51–3.
Fox M, Barr C, Nolan S, Lomer M, Anggiansah A, Wong T. The effects of dietary fat and calorie density on esophageal acid exposure and reflux symptoms. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2007;5(4):439–44. e1
Kotrba C, Code C. Gastric acid secretory responses to some purified foods and to additions of sucrose or olive oil. The American Journal of Digestive Diseases. 1969;14(1):1–8.
Colombo P, Mangano M, Bianchi PA, Penagini R. Effect of calories and fat on postprandial gastro-oesophageal reflux. Scandinavian Journal of Gastroenterology. 2002;37(1):3–5.
Ikonen T, Morri S, Tyrisevä AM, Ruottinen O, Ojala M. Genetic and phenotypic correlations between milk coagulation properties, milk production traits, somatic cell count, casein content, and pH of milk. Journal of dairy science. 2004;87(2):458–67.
FDA, Guidance for industry: food-effect bioavailability and fed bioequivalence studies, CDER. 2002: Washington, DC.
Author information
Authors and Affiliations
Corresponding author
ELECTRONIC SUPPLEMENTARY MATERIAL
ESM 1
(PDF 508 kb)
Rights and permissions
About this article
Cite this article
Sutton, S.C., Nause, R. & Gandelman, K. The impact of gastric pH, volume, and emptying on the food effect of ziprasidone oral absorption. AAPS J 19, 1084–1090 (2017). https://doi.org/10.1208/s12248-017-0065-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12248-017-0065-9