Abstract
Background
Noninvasive ventilation (NIV) is frequently employed as a treatment option for acute hypercapnic respiratory failure (AHRF) resulting from chronic obstructive pulmonary disease (COPD). Limited research has substantiated the claims made in recent studies regarding the feasibility of employing high flow nasal cannula (HFNC).
Aim
Our study assessed the outcome of using HFNC versus NIV for COPD patients with AHRF.
Patients and methods
Eighty COPD patients with AHRF were confined to the respiratory intensive care unit (RICU) at Ain-Shams University Hospitals from December 2021 to 2023 and subdivided into two groups (40/group), where the first group was placed on NIV while the second group was placed on HFNC. Data during their hospital stay as demographic data, vital data, arterial blood gases, device duration, treatment failure, and mortality were recorded.
Results
The majority were males with mean age 63.75 ± 9.05 years along with treatment failure and complications 25%, 12.5.% in NIV versus 45%, and zero% in HFNC, respectively, with longer hospital stay in NIV 10–15 days to 7–10 days in HFNC, and with no difference in mortality rate in both groups.
Conclusion
Both modalities NIV and HFNC were effective for treating COPD with AHRF. However, NIV group was significantly superior than HFNC along with apparently faster improvement in ventilatory and respiratory status especially in high CO2 level while less complications and duration of hospital stay in HFNC with no difference in mortality in both groups.
Similar content being viewed by others
Introduction
Globally, chronic obstructive pulmonary disease (COPD) continues to be a leading cause of morbidity and mortality. Acute respiratory failure (ARF) accompanied by hypercapnia is characterized by a significant requirement for respiratory support and an elevated risk of death among COPD patients [1].
Noninvasive ventilation (NIV) is regarded as the cornerstone of treatment for hypercapnic ARF patients and COPD [2]. Although NIV may not be suitable for all patients, nearly a quarter of them have contraindications to its use [3].
Therapy with high-flow nasal cannula (HFNC) oxygen is considered more acceptable than NIV [4], and over the past few years, it has been assessed as a potential replacement for NIV in ARF [5,6,7]. In stable COPD patients, HFNC increases exercise tolerance and decreases partial pressure of carbon dioxide (PaCO2), respiratory rate, and work of breathing [8, 9]. Nonetheless, the efficacy of HFNC in hypercapnic ARF has not been comprehensively evaluated [10].
Thus, our study assessed the outcome of using HFNC versus NIV for COPD patients with acute hypercapnic respiratory failure.
Methods
Our present prospective randomized control study was performed on COPD patients with AHRF who were admitted to the Respiratory Intensive Care Unit (RICU) at Ain Shams University Hospitals from December 2021 to December 2023. Eighty patients participated in the investigation; they were randomly divided into 2 groups of 40 each; in the first group, noninvasive ventilation was implemented, whereas in the second group, high-flow nasal cannula was utilized.
Participants
After the approval of Ain Shams University Ethical Committee (FMASU MD195/2020), and obtaining written informed consent, COPD patients diagnosed by global initiative for obstructive lung disease (GOLD) 2020 [11] with acute respiratory failure (defined as respiratory acidosis “pH ≤ 7.35 and PaCO2 ≥ 50 mmHg” or exacerbation of dyspnea with accessory respiratory muscle use or persistent hypoxemia inspite of oxygen therapy) [12] were collected by convenience sample, while patients with severe respiratory failure necessitating instant endotracheal intubation or contraindication to NIV or patients who had previously used any of those two devices (NIV or HFNC) were excluded.
The patients who were included in the study were classified into two distinct categories upon their admission to the RICU: individuals who commenced noninvasive ventilation (NIV) within the initial 4 h of their admission were classified as part of the NIV group. This group utilized the Nellcor Puritan Bennett 840 ventilator system, manufactured in Minnesota, USA, and employed an oronasal interface with bilevel-positive airway pressure (BiPAP). Specifically, inspiratory-positive airway pressure was set at 10–12 cm H2O, and expiratory positive airway pressure was initiated at 4–5 cm H2O, with subsequent adjustments made based on the patients’ arterial blood gases and physiological responses.
Patients who commenced HFNC within the initial 4 h of their admission were likewise classified as members of the HFNC group (using Fisher & Paykel Airvo 2 HFNC device made in Tamaki, New Zealand) with fraction of inspired oxygen adjusted to sustain oxygen saturation (spO2) between 88 and 92%, with adjusted flow, while the humidifier temperature was set to 37 °C. Furthermore, in the event where the patient subsequently underwent invasive mechanical ventilation or another ventilatory support device during their admission, their group classification remained unchanged.
Data collection
All patients were subjected to detailed medical history (age, gender & smoking status, relevant comorbidities) and past history (previous hospital and ICU admission, need of long-term oxygen therapy), and then general and local examination was done for all patients as well as laboratory and radiological investigation (complete blood count, Chest X-ray). Clinical parameters like respiratory rate, heart rate, blood pressure, Sequential Organ Failure Assessment “SOFA” score, and arterial blood gases were assessed at the moment of admittance, 4 h and 24 h subsequent to the initiation of NIV or HFNC therapy (4 h and 24 h were chosen as time of recording vital data and arterial blood gases as they were considered to serve as a predictive factor for the success of the device utilized in our patients) [13]. Also, the duration of using the device, length of hospital and ICU stays, complications, treatment failure, and switch were recorded.
NB: Treatment failure refers to a deterioration in clinical parameters after 4-h post-treatment requiring treatment switch or escalation to invasive mechanical ventilation (IMV) directly. Treatment switch was defined as a change in ventilation modality due to a lack of improvement in clinical parameters within 4 h of treatment initiation, without meeting the criteria for IMV — criteria for IMV: respiratory or cardiac arrest, development of condition that requires intubation to guard the airway as coma or seizure, progressive respiratory muscle fatigue, and hemodynamic instability which lack response to fluids and vasoactive agents [14].
And to avoid any biases, one researcher collected data about NIV group, another researcher collected data about HFNC group, and then data was coded and sent for statistical analysis.
Statistical analysis
The quantitative data were analyzed utilizing IBM SPSS version 27. For parametric data, the results were presented as means, standard deviations, and ranges; for nonparametric data, the median and interquartile range were utilized. The values of qualitative variables were represented as percentages and numerals. Group comparisons for qualities of data utilized the chi-square or Fisher exact test, while for quantitative data, the independent t-test was used for parametric distribution and the Mann–Whitney test for nonparametric distribution. Repeated measures ANOVA and Friedman tests were employed for comparisons among more than two paired groups with parametric and nonparametric distribution, respectively. Univariate and multivariate logistic regression analyses were conducted to identify predictors of treatment failure in the HFNC group, and Kaplan–Meier analysis was used to assess overall survival. A confidence interval of 95% and a significance level of < 0.05 were considered to be statistically significant.
Results
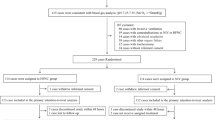
Our results showed that there was treatment failure in nearly half the patients of HFNC in comparison to nearly quarter the patients of NIV. Among the 18 patients experiencing treatment failure in the HFNC group, 10 patients (55.0%) were switched to NIV, of whom 8 patients (80.0%) achieved successful treatment, while 2 (20.0%) required mechanical ventilation. In contrary, no patients in the NIV group who experienced treatment failure were switched to HFNC; instead, they were all promptly shifted to invasive mechanical ventilation as shown in Fig. 1.
Table 1 showed that there were no significant differences observed in demographic data and characteristics between the NIV and HFNC groups.
Vital signs, arterial blood gases, and SOFA score were recorded at baseline and 4 h in both groups, but after 24 h, the data was recorded in all NIV group and only succeeded patients in HFNC group (22 patients). There were no significant differences between both studied groups regarding vital signs, SOFA score, and PiO2/FiO2%, while regarding the arterial blood gases parameters, the improvement was faster in NIV group in Table 2.
In Table 3, treatment failure rate was lower in the NIV group compared to the HFNC, although this difference did not reach statistical significance (p = 0.061), and circulatory failure was a significant cause of failure in NIV group. As regards the mortality rate between both groups, it was nearly the same. There was also a high statistical significance regarding duration of device application and total hospital stay between both groups, as NIV group had longer duration of device application and longer hospital stay. Also, number of patients who had complications on NIV (five patients) was higher than those on HFNC (0 patient) (p 0.065) but not reaching statistical significance. Psychosis exhibited a notably higher incidence rate among patients in the NIV group compared to those in the HFNC group (p 0.040).
In Table 4, in the univariate analysis, several factors showed significant associations with the outcome. These include hypertension (HTN) (p = 0.007), baseline and 4-h SOFA score > 2 (p = 0.016, 0.000) respectively, 4-h respiratory rate > 24 (p = 0.000), heart rate > 95 (p = 0.000), pCO2 > 58 (p = 0.001), PaO2/FiO2% < = 171 (p = 0.000), duration of device application < = 5 h (p = 0.000), and oxygen flow rate > 35 (p = 0.028). These results indicate that these variables may play a significant role in predicting the outcome. In the multivariate analysis, baseline only PaO2/FiO2% < = 171 at 4 h (p = 0.000) remained significant predictor, while other variables did not show significant associations with the outcome in the multivariate analysis.
In Fig. 2, the Kaplan–Meier curve analysis for cumulative survival rate showed comparable outcomes between the NIV and HFNC groups, with no statistically significant difference observed. Both groups had similar mean total hospital stays, suggesting similar overall mortality rates. The log-rank test further confirmed the lack of statistical significance between the two groups, indicating that the choice of ventilatory support did not significantly impact mortality outcomes in this study population.
Discussion
Nowadays, NIV is on the top of interventions in order to manage respiratory failure caused by COPD. However, NIV intolerance, however, is prevalent, as well as elevated intubation rates and overall mortality [15]. In contrast, HFNC is a new method of oxygen therapy with a high tolerance profile. However, many literatures on HFNC have excluded patients with ARF and hypercapnia [16].
So, our study investigated the outcome of using HFNC versus NIV for COPD patients with AHRF, and it was found that treatment failure rate was 25% in NIV versus 45% in HFNC, but this difference did not reach a significant statistical level (p = 0.061), and by reviewing other literatures on this topic, it was found that treatment failure was also higher in HFNC (56%, 38.6%) than NIV (41%, 11.4%) respectively as mentioned in both retrospective studies of Koga et al. and Wang et al. [17, 18].
In contrast to the above mentioned studies, Sun et al. demonstrated a reduced treatment failure rate in the HFNC cohort relative to NIV. However, all of the above mentioned studies and ours did not reach statistical significance except that of Wang et al., so up until now, no device of them showed superiority in management of COPD with AHRF [18, 19].
Our study observed no significant differences in demographics and baseline characteristics between the NIV and HFNC groups. These findings resonate with the conducted research by Lee et al., who reported no baseline characteristic difference between the two groups, and this is considered as point of strength in our study to avoid any confounding factor that might affect the outcome of any of both devices [20].
A total of 80% were either current or ex-smokers with an average of 50 pack-years, closely resembling the study done by Sun et al., where 61.4% of the studied patients were either current or ex-smokers [19]; these findings correlate with Kohansal et al., who reported that individuals who smoke cigarettes experience a greater incidence of respiratory symptoms and lung function abnormalities, exhibit a more rapid annual decrease in FEV1, and have a higher mortality rate from COPD compared to non-smokers [21]. Also, hypertension was the most common comorbidity, observed in both our study (38.8%) and theirs (56.1%) [19]. This finding aligns with the latest COPD guidelines, which suggest that hypertension is likely the most prevalent comorbidity in COPD and may affect prognosis [22].
Analysis of vital data parameters attained no statistically significant differences between the HFNC and NIV groups 4- and 24-h post-treatment. These results are consistent with the study conducted by Cortegiani et al., who compared HFNC versus NIV as initial ventilatory strategy during COPD exacerbation in a non-inferiority randomized multicentric trial, and reported that no differences in vital data parameters were found between both groups after 2- and 6-h post-treatment. It also agrees with the study carried out by Sun et al., who reported no significant differences between the two groups in terms of respiratory rate 24-h post-treatment [19, 23].
Additionally, analysis of respiratory parameters revealed no substantial differences in pH, PaCO2, or PaO2/FiO2 between HFNC group and NIV group after 4 and 24 h. These findings agree with the study conducted by Lee et al. who reported similar improvement in both groups with no significant differences in respiratory parameters after 6- and 24-h post-treatment, but in contrary to Lee et al., this study showed faster improvement in respiratory parameter after 4 h in NIV in comparison to HFNC [20].
In our study, the HFNC group exhibited a shorter duration of device application along with shorter total hospital stay; these findings corroborate the results of the retrospective study performed by Wang et al., who found that HFNC also was substantially related to shorter length of ICU stay, hospital stay, and total ventilation days than NIV, despite exhibiting more treatment failure in our study and theirs [18].
In our study, complications in the NIV group occurred at twice the rate compared to the HFNC group. This agrees with Sun et al. who observed a higher rate of complications in the NIV group compared to the HFNC group. Notably, nasal facial breakdown was the most common complication in their study, whereas psychosis was more prevalent in ours. This may be explained by the diversity in the study population between both studies [19].
In our study, treatment failure was mainly linked to hypoxia, hypercapnia, and circulatory failure. Notably, there was no statistical significance between the two groups regarding hypoxia and hypercapnia as causes of treatment failure, mirroring the observations of Sun et al. who also noted no distinction in respiratory distress, hypoxemia, and carbon dioxide retention between the two groups. However, in our study, hypercapnia significantly contributed to treatment failure in NIV group, though it is not reaching statistical significance [19].
Additionally, in our study, circulatory failure emerged as a significant contributing factor, particularly affecting the NIV group more than the HFNC group; this finding is consistent with the pilot randomized controlled trial conducted by Jing et al., comparing effect of HFNC and NIV in hypercapnic COPD patients, and this can be explained that blood pressure decreased significantly after using NIV but not significantly after using HFNC, and this is due to the impact of NIV on affecting venous return than HFNC [24].
Mortality rates were nearly equivalent between the two modalities. Therefore, our study was maintaining consistency with the findings of the meta-analysis performed by Liu et al., who reported no significant differences in mortality outcomes between the two modalities. Also, Wang et al., reported that the 30-day mortality and 90-day mortality rates for the HFNC and NIV groups were nearly equivalent [18, 25].
Also, the previous nonstatistically significant difference in mortality was confirmed by Kaplan–Meier curve analysis which revealed comparable cumulative survival rates, indicating no significant distinction between both treatment modalities (log-rank test 2.265, p = 0.132).
Our study identified several predictors of treatment failure with HFNC therapy through performing univariable and multivariable logistic regression analyses. The univariate analysis of the HFNC group unveiled a number of factors that exhibited statistically significant correlations with the outcome. These include hypertension (HTN) (p = 0.007), baseline and 4-h SOFA score > 2 (p = 0.016, 0.000) respectively, 4-h respiratory rate > 24 (p = 0.000), heart rate > 95 (p = 0.000), pCO2 > 58 (p = 0.001), PaO2/FiO2% < = 171 (p = 0.000), duration of device application < = 5 h (p = 0.000), and oxygen flow rate > 35 (p = 0.028). According to these findings, these variables might have a substantial impact on the outcome prediction. In the multivariate analysis, only PaO2/FiO2% < = 171 at 4 h (p = 0.000) remained significant predictor, while other variables did not show significant associations with the outcome in the multivariate analysis.
In contrary to our findings, none of the above factors was significant in the univariable logistic regression analyses of the study conducted by Wang et al., who only exhibited NT-proBNP as the sole significant determinant of HFNC failure in the univariate analysis, a variable that was omitted from our analysis [18].
Limitations
Initially, the study was not multicentric hindering larger and more variable sample size with relatively brief duration. Additionally, the decision in the study to start with NIV or HFNC was made on a clinical basis, raising the possibility of selection bias. However, it is worth noting that there were no statistically significant differences in baseline characteristics between the two groups, so this factor did not impact the effectiveness of either device.
Conclusion
Both modalities NIV and HFNC were effective for treating COPD with AHRF. However, NIV group was significantly superior than HFNC along with apparently faster improvement in ventilatory and respiratory status especially in high CO2 level while less complications and duration of hospital stay in HFNC with no difference in mortality in both groups.
Availability of data and materials
The datasets utilized or examined in this study can be obtained from the corresponding author upon request.
Abbreviations
- HFNC:
-
High-flow nasal cannula oxygen therapy
- NIV:
-
Noninvasive ventilation
References
Brown H, Dodic S, Goh SS, et al. (2018). Factors associated with hospital mortality in critically ill patients with exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:2361–2366. https://doi.org/10.2147/COPD.S168983.
Shah NM, D’Cruz RF, Murphy PB (2018) Update: non-invasive ventilation in chronic obstructive pulmonary disease. J Thoracic Dis 10(Suppl 1):S71
Brochard L, Mancebo J, Wysocki M et al (1995) Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. NEJM 333(13):817–822
Ischaki E, Pantazopoulos I, Zakynthinos S (2017). Nasal high flow therapy: a novel treatment rather than a more expensive oxygen device. Eur Respir Rev. 2017;26(145):170042. https://doi.org/10.1183/16000617.0028-2017.
Frat JP, Thille AW, Mercat A et al (2015) High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. NEJM 372(23):2185–2196
Hernández G, Vaquero C, González P et al (2016) Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA 315(13):1354–1361
Hernández G, Vaquero C, Colinas L et al (2016) Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients: a randomized clinical trial. JAMA 316(15):1565–1574
Bräunlich J, Köhler M, Wirtz H (2016). Nasal highflow improves ventilation in patients with COPD. Int J Chronic Obstruct Pulm Dis. 2016;11:1077–1085. https://doi.org/10.2147/COPD.S104616.
Pisani L, Fasano L, Corcione N et al (2017) Change in pulmonary mechanics and the effect on breathing pattern of high flow oxygen therapy in stable hypercapnic COPD. Thorax 72(4):373–375
Millar J, Lutton S, O’Connor P (2014) The use of high-flow nasal oxygen therapy in the management of hypercarbic respiratory failure. Therap Adv Res Dis 8(2):63–64
Rabe KF, Hurd S, Anzueto A et al (2007) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Res Crit Care Med 176(6):532–555
Bosnic-Anticevich SZ, Kim DK, Lee J et al (2018) What can we apply to manage acute exacerbation of chronic obstructive pulmonary disease with acute respiratory failure? Tuberc Res Dis 81(2):99–105
Chawla RK, Yadav V, Banerjee S et al (2021) Predictors of success and failure of non-invasive ventilation use in type-2 respiratory failure. Indian J Tubercul 68(1):20–24
Chen Q, Liu M, Liu B, et al. (2020). Predictive factors for failure of noninvasive ventilation in adult intensive care unit: a retrospective clinical study. Can Respir J. 2020;2020:1324355. https://doi.org/10.1155/2020/1324348.
Liu J, Duan J, Bai L et al (2016) Noninvasive ventilation intolerance: characteristics, predictors, and outcomes. Res Care 61(3):277–284
Friggeri A, Cazalis MA, Pachot A et al (2016) Decreased CX3CR1 messenger RNA expression is an independent molecular biomarker of early and late mortality in critically ill patients. Crit Care 20:1–13
Koga Y, Kaneda K, Fujii N et al (2020) Comparison of high-flow nasal cannula oxygen therapy and non-invasive ventilation as first-line therapy in respiratory failure: a multicenter retrospective study. Acute Medicine & Surgery 7(1):e461
Wang M, Zhao F, Sun L, et al. (2023). High-flow nasal cannula versus noninvasive ventilation in AECOPD patients with respiratory acidosis: a retrospective propensity score-matched study. Can Respir J. 2023;2023:6377451. https://doi.org/10.1155/2023/6377441.
Sun J, Li Y, Ling B, et al. (2019). High flow nasal cannula oxygen therapy versus non-invasive ventilation for chronic obstructive pulmonary disease with acute-moderate hypercapnic respiratory failure: an observational cohort study. Int J Chron Obstruct Pulmon Dis. 2019;14:1229–1237. https://doi.org/10.2147/COPD.S206567.
Lee MK, Choi J, Park B et al (2018) High flow nasal cannulae oxygen therapy in acute-moderate hypercapnic respiratory failure. Clin Res J 12(6):2046–2056
Kohansal R, Martinez-Camblor P, Agustí A et al (2009) The natural history of chronic airflow obstruction revisited: an analysis of the Framingham offspring cohort. Am J Res Crit Care Med 180(1):3–10
Divo M, Cote C, de Torres JP et al (2012) Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Res Crit Care Med 186(2):155–161
Cortegiani A, Longhini F, Madotto F et al (2020) High flow nasal therapy versus noninvasive ventilation as initial ventilatory strategy in COPD exacerbation: a multicenter non-inferiority randomized trial. Crit Care 24:1–13
Jing G, Li J, Hao D et al (2019) Comparison of high flow nasal cannula with noninvasive ventilation in chronic obstructive pulmonary disease patients with hypercapnia in preventing postextubation respiratory failure: a pilot randomized controlled trial. Res Nurs Health 42(3):217–225
Liu Y, Zhang Y, Zeng Y et al (2023) High-flow nasal cannula versus noninvasive ventilation after extubation in hypercapnic patients with COPD: a retrospective analysis. Chinese Med J 136(16):2008–2010
Acknowledgements
None
Funding
None.
Author information
Authors and Affiliations
Contributions
The idea and design of the study were contributed to all authors. AM handled the preparation of the materials as well as the data collecting and analysis. MA and DR authored the original draft of the manuscript, while MF revised it. Every author offered feedback on earlier drafts of the work. The final manuscript was read and approved by all writers.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval of Ain Shams University Ethical Committee was acquired (FMASU MD195/2020), and written informed consent from patients’ relatives was gained owing to their critical condition.
Consent for publication
None.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mashad, A.G., Farrag, M., Ali, M. et al. Comparing the outcome of using high-flow nasal cannula oxygen therapy versus noninvasive ventilation for chronic obstructive pulmonary disease patients with acute hypercapnic respiratory failure. Egypt J Bronchol 18, 74 (2024). https://doi.org/10.1186/s43168-024-00326-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-024-00326-6