Abstract
Background
Some of the pulmonary tuberculous patients who completed their medication course experience lung function impairment which may influence their quality of life. However, the pattern and nature of post-tuberculosis lung impairment are still not identified. Thus, the aim of this study was to determine the type and degree of lung physiology changes in previously treated tuberculous patients which latter may affect their quality of life, thus helping clinicians for early diagnosis of lung impairment, especially in tuberculous endemic areas.
Results
Adults (≥18 years) who were treated from first attack pulmonary tuberculosis were included in the study. Demographic data, respiratory symptoms, smoking history, comorbidities, Medical Research Council dyspnea score (MRC), spirometry, chest radiography, and oxygen saturation were collected. One hundred ninety-seven participants were finally included in the study. The mean age was 49.50±13.26 years with males representing 75.6% of total patients. MRC dyspnea scale grading showed that about 13.2% and 5.1% of patients suffer from dyspnea grade II and grade III, respectively. Main respiratory symptoms were cough in 38.1%, sputum production in 24.9%, and hemoptysis in 6.6% cases. Normal spirometry was documented in 53.3%, obstructive pattern in 31.98%, and mixed pattern in 7.11%, whereas 7.61% cases had a restrictive pattern. According to ATS staging of obstructive pattern, 27 patients (42.8%) had mild obstruction, 22 (34.9%) patients had moderate obstruction, 13 (20.6%) patients had moderate to severe obstruction, and one patient (1.6%) had severe obstruction.
Conclusions
Impairment of respiratory function after tuberculosis is one of the causes of chronic lung disease that is underestimated, especially in endemic countries. This impairment in function occurs early in the course of the diseases and even without symptoms, affecting the quality of life. Thus, clinicians should encourage patients for an earlier visit to a respiratory clinic for follow-up and further management if needed. Guidelines for the management of cured tuberculous patients are urgently needed.
Trial registration
ClinicalTrials.gov, NCT05097638. Registered on October 28, 2021—retrospectively registered
Similar content being viewed by others

Background
Tuberculosis (TB) is one of the infectious diseases that may cause death worldwide. Unlike other respiratory infections, TB can lead to permanent lung damage. Therefore, TB may turn from being a treatable infectious disease into a chronic disease that can cause morbidity in successfully treated patients [1].
In tuberculous patients, even after a full course of treatment and cure, permanent parenchymal sequelae and functional lung impairment of variable degrees sometimes occur [2] causing pulmonary function impairment, so altering their quality of life [3]. The degree of severity of functional changes is correlated to the extent of the initial TB affection [4]. Even minimal scar change on chest radiograph may lead to airflow limitation [5, 6].
During an active pulmonary tuberculosis treatment phase, ventilation impairment in lung function is usually restrictive. This may persist, resolve, or change to an obstructive pattern later [7, 8]. Tuberculous patients have two- to fourfold higher odds of permeant functional changes (restrictive or obstructive pattern) compared with patients without tuberculosis [9, 10].
Tuberculosis (TB) has become an emerging risk factor in the development of COPD [11]. Also, there is developing evidence of co-morbidity between tuberculosis (TB) and COPD [12]. Several population-based epidemiological studies found a relationship between TB and airflow obstruction [9]. Therefore, post-tuberculosis patients extensively contribute to the growing worldwide burden of COPD [9, 13, 14].
Aim of this study
This study aimed to determine the type and degree of lung physiology changes in previously treated tuberculous patients which later may affect their quality of life, thus helping clinicians for early diagnosis of lung impairment, especially in tuberculous endemic areas.
Methods
Study design and setting
This study was a cross-sectional cohort study. It was conducted at Assiut University Hospital from January 2018 to February 2020. The participant provided written informed consent before enrollment in the study after explaining the nature of the study. All patients were recruited from the tuberculosis clinic.
Inclusion criteria
Patients more than 18 years old who had been newly diagnosed drug-sensitive first episode pulmonary tuberculosis, confirmed by sputum smear microscopy, were included in the study. They completed an outpatient course of standard first-line antituberculosis therapy (6 months) and declared as cured without radiological change over the past year (in comparable with chest X-ray at the end of TB treatment).
Exclusion criteria
Patients were excluded from the study if they were smokers (to avoid spirometry biases). Exclusion criteria inculde: extrapulmonary tuberculosis cases, multidrug-resistant tuberculosis, known contraindications to spirometry testing, individuals with chest wall deformities or neuromuscular diseases, patients who failed to achieve acceptability and reproducibility criteria of the spirometry test, defaulter cases or irregular treatment, known coexisting chronic lung disease as history of asthma or interstitial lung diseases, a history of illicit drug use, and patients with comorbidities: renal and hepatic insufficiency, heart diseases, and metabolic disorders.
The following variables were collected: past medical history, weight, height, symptom scores: Medical Research Council dyspnea score (MRC), pulmonary function tests (spirometry), and chest imaging which included chest radiography (CXR) at baseline (end of TB treatment) and 12 months, and oxygen saturation was measured by a pulse oximeter. All data were obtained on the day of the spirometry.
Study measurements
Functional assessment
Spirometry was performed by Quark PFTs ergo, P/N Co9035–12–99 (Cosmed Srl, Albano Laziale, RM, Italy). Spirometry results were interpreted according to the ATS guideline [15]. Participants who had a ratio of FEV1 to FVC less than LLN were subjected to a post-bronchodilator test using 15 min after administration of 400 μg salbutamol using a pressurized metered-dose inhaler with a small-volume spacer device [16]. COPD was defined as a ratio of FEV1 to FVC < 0.7 (this is the cutoff point for diagnosis of COPD according to the GOLD guidelin). The severity of obstruction was graded on the basis of FEV1 as follows: mild ≥70%, moderate 60–69%, moderate severe 50–59%, severe 35–49%, and very severe < 35%. A restrictive pattern is indicated by a ratio of FEV1 to FVC that is normal and FVC less than LLN [17].
MRC dyspnea scale
The MRC dyspnea scale [18] was used to assess the severity of dyspnea. It is a 5-point scale that measures the level of breathlessness. It is 5 grades:
-
Grade 1: short of breath with strenuous exercise
-
Grade 2: short of breath when hurrying on a level or walking up a slight hill
-
Grade 3: walks slower than people of the same age on the level or must stop for breath when walking at own pace
-
Grade 4: stops for breath after 100 m at own pace
-
Grade 5: too breathless to leave the house
Statistical analysis
The study variables were analyzed using the IBM SPSS Statistics software, version 22.0 (IBM Corporation, Armonk, NY, USA). Continuous variables are expressed as means and standard deviations whereas categorical variables are expressed as absolute and relative frequencies.
Results
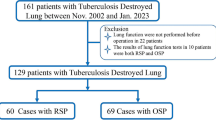
A total of 210 patients were enrolled and followed up for 1 year. Participants did not complete the final study: eleven were lost to follow-up and two relocated. One hundred ninety-seven participants were finally included in the study. The mean age was 49.50±13.26 years with males representing 75.6% of total patients. BMI was 20.79±4.03, and oxygen saturation was 97.69±0.93 as shown in Table 1. MRC dyspnea scale grading among participants showed that about 81.7% (161 cases), 13.2% (26 cases), and 5.1% (10 cases) patients suffer from dyspnea grades I, II, and III, respectively (Fig. 1). Moreover, participants reported different respiratory symptoms: cough in 38.1% cases, sputum production in 24.9% cases, and hemoptysis in 6.6% cases (Fig. 2).
Regarding spirometry assessment, normal spirometry was documented in 105 cases (53.3%), an obstructive pattern was documented in 63 (31.98%) cases with positive bronchodilator reversibility in 4 cases (6.35%), and a mixed pattern in 14 (7.11%) cases, whereas 15 (7.61%) cases had a restrictive pattern (Fig. 3). Regarding obstructive pattern, 27 patients (42.8%) had mild obstruction, 22 patients (34.9%) had moderate obstruction, 13 patients (20.6%) had moderate to severe obstruction, and one patient (1.6%) had severe obstruction. No patient was very severe (Fig. 4).
Discussion
The results of this prospective study on Egyptian patients who had pulmonary tuberculosis provided several information about lung function impairment and sequence of chronic lung disease following treatment. After 1 year of completing antituberculosis treatment, around half of patients suffer from lung function abnormality. This would decrease exercise capacity and decreased their quality of life.
Our study showed a male predominance with mean age 49.50±13.26. Participants reported different symptoms including cough, sputum, and breathlessness due to pulmonary tuberculosis sequelae.
Meghji et al. noted that respiratory symptoms were reported by 30.7% of patients after 1 year of antituberculosis treatment, with breathlessness being more common than cough and sputum [10]. Dyspnea is a predictor of quality of life, and improving dyspnea should be a great objective in those patients [19]. One study done in Uganda introduced the post-tuberculous patients in a 6-week pulmonary rehabilitation program to improve exercise tolerance [20].
In our patient sample, the prevalence of abnormal spirometry was 46.7%, with a predominant obstructive pattern (31.9%). Several studies [21,22,23,24] assessing pulmonary function after the end of anti-TB treatment showed that more than half of patients had lung function impairment either obstructive, restrictive, or mixed with different grades of severity. A study done in the USA showed that around 60% of tuberculous patients had abnormal function [25]. Chushkin et al. observed that approximately 50% of tuberculous patients suffered from impaired pulmonary function; obstructive was the frequent one followed by restrictive [26]. Many studies [24,25,26,27] reported restriction as the predominant pattern. This is explained by lung parenchyma destruction [28]. On the contrary, other studies documented obstruction as the most common abnormality [13, 29, 30]. Patil et al. noted the same pattern of spirometry abnormality [31]. Agarwala et al. observed that 52.7% of treated tuberculous Indian patients had an obstructive defect [32]. Gothi et al. in an Indian study explained that post-tuberculous airflow obstruction may be sequala of obliterative bronchiolitis [33]. In three large studies, their authors concluded a significant association between pulmonary tuberculosis history and the presence of obstructive airway diseases [13, 34, 35]. Several studies [8, 36,37,38,39] estimated that 20% of non-smoker patients fulfilled COPD criteria by spirometry. Di Naso et al. [30] in a Brazilian study found that 15.7% of COPD patients had previous pulmonary tuberculosis.
Our result suggests that impaired lung function after tuberculosis is one of the causes of chronic lung disease that is underestimated especially in endemic countries. The impairment in function and decrease in quality of life occur start early after being cured and even without symptoms. This is in agreement with Pasipanodya et al. [25]. In a systematic review done in 2009, they concluded that tuberculosis had a negative impact on quality of life even after being cured [40]. An International Post-tuberculosis Symposium in 2019 defines post-TB lung disease as “evidence of chronic respiratory abnormality, with or without symptoms, attributable at least in part to previous tuberculosis” [19, 41]. However, TB as a risk factor for the development of COPD is still unclear. Past history of pulmonary tuberculosis is an important risk factor for chronic lung diseases as smoking and pollution [19].
Because no relevant guidelines illustrate how to follow up post-tuberculous patients, most of them either suffer silently or receive irrelevant treatment [14]. Therefore, tuberculosis guidelines must have a systematic approach for how to follow up these patients (functional and radiological), thus helping clinicians for early diagnosis of chronic lung affection, especially in tuberculous endemic areas [20].
Conclusions
Impairment of respiratory function after tuberculosis is one of the causes of chronic lung disease that is underestimated, especially in endemic countries. This impairment in function occurs early in the course of the diseases and even without symptoms, affecting the quality of life. Thus, clinicians should encourage patients for an earlier visit to the respiratory clinic for follow-up and further management if needed. Guidelines for the management of cured tuberculous patients are urgently needed.
Availability of data and materials
The data sets generated and/or analyzed during the present study are not publicly available, but they are available from the corresponding author on reasonable request.
Abbreviations
- MRC:
-
Medical Research Council dyspnea score
- GOLD:
-
The Global Initiative for Chronic Obstructive Lung Disease
- TB:
-
Tuberculosis
- FEV1:
-
First second of forced expiration
- FVC:
-
Forced vital capacity
- BMI:
-
Body mass index
- COPD:
-
Chronic obstructive pulmonary disease
- ATS:
-
American Thoracic Society
References
Allwood B, Van Der Zalm M, Amaral A, Byrne A, Datta S, Egere U et al (2020) Post-tuberculosis lung health: perspectives from the first international symposium. Int J Tubercul Lung Dis 24(8):820–828
Pefura-Yone EW, Balkissou AD, Djenabou A, Poka-Mayap V, Moifo B, Madjoumessi M-C et al (2019) Prediction of post-tuberculosis lung function impairment. Am J Intern Med 6(6):170
Harries AD, Ade S, Burney P, Hoa NB, Schluger NW, Castro JL (2016) Successfully treated but not fit for purpose: paying attention to chronic lung impairment after TB treatment. Int J Tubercul Lung Dis 20(8):1010–1014
Jung KH, Kim SJ, Shin C, Kim JH (2008) The considerable, often neglected, impact of pulmonary tuberculosis on the prevalence of COPD. Am J Respir Crit Care Med 178(4):431–431
Hnizdo E, Singh T, Churchyard G (2000) Chronic pulmonary function impairment caused by initial and recurrent pulmonary tuberculosis following treatment. Thorax 55(1):32–38
Hsu D, Irfan M, Jabeen K, Iqbal N, Hasan R, Migliori GB et al (2020) Post tuberculosis treatment infectious complications. Int J Infect Dis 92:S41–S45
Chakaya J, Kirenga B, Getahun H (2016) Long term complications after completion of pulmonary tuberculosis treatment: a quest for a public health approach. (Elsevier), pp 10–12
Radovic M, Ristic L, Ciric Z, Dinic-Radovic V, Stankovic I, Pejcic T et al (2016) Changes in respiratory function impairment following the treatment of severe pulmonary tuberculosis–limitations for the underlying COPD detection. Int J Chron Obstruct Pulmon Dis 11:1307
Amaral AF, Coton S, Kato B, Tan WC, Studnicka M, Janson C et al (2015) Tuberculosis associates with both airflow obstruction and low lung function: BOLD results. Eur Respir J 46(4):1104–1112
Meghji J, Lesosky M, Joekes E, Banda P, Rylance J, Gordon S et al (2020) Patient outcomes associated with post-tuberculosis lung damage in Malawi: a prospective cohort study. Thorax 75(3):269–278
Allwood BW, Gillespie R, Galperin-Aizenberg M, Bateman M, Olckers H, Taborda-Barata L et al (2014) Mechanism of airflow obstruction in tuberculosis-associated obstructive pulmonary disease (TOPD) D39. In: Connecting the dots: drawing lines between COPD and comorbid conditions. (American Thoracic Society), pp A5832–A5832
O'Toole RF, Shukla SD, Walters EH (2015) TB meets COPD: an emerging global co-morbidity in human lung disease. Tuberculosis 95(6):659–663
Menezes AMB, Hallal PC, Perez-Padilla R, Jardim J, Muiño A, Lopez M et al (2007) Tuberculosis and airflow obstruction: evidence from the PLATINO study in Latin America. Eur Respir J 30(6):1180–1185
Pandey A, Agrawal R, Agarwal R, Kumar A, Gupta U, Sharma D (2020) Assessment of symptomatic post tuberculosis patients by spirometry and chest X ray
Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL et al (2019) Standardization of spirometry 2019 update. An official American Thoracic Society and European Respiratory Society technical statement. Am J Respir Crit Care Med 200(8):e70–e88
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A et al (2005) Standardisation of spirometry. Eur Respir J 26(2):319–338
Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J et al (2017) Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med 195(5):557–582
Cotes J (1987) Medical research council questionnaire on respiratory symptoms (1986). Lancet 330(8566):1028
Ozoh O, Ojo O, Dania M, Dede S, Adegboyega O, Irurhe N et al (2021) Impact of post-tuberculosis lung disease on health-related quality of life in patients from two tertiary hospitals in Lagos, Nigeria. Afr J Thoracic Crit Care Med 27(2):46–52
Jones R, Kirenga BJ, Katagira W, Singh SJ, Pooler J, Okwera A et al (2017) A pre–post intervention study of pulmonary rehabilitation for adults with post-tuberculosis lung disease in Uganda. Int J Chron Obstruct Pulmon Dis 12:3533
Pasipanodya JG, McNabb SJ, Hilsenrath P, Bae S, Lykens K, Vecino E et al (2010) Pulmonary impairment after tuberculosis and its contribution to TB burden. BMC Public Health 10(1):1–10
Maguire G, Anstey NM, Ardian M, Waramori G, Tjitra E, Kenangalem E et al (2009) Pulmonary tuberculosis, impaired lung function, disability and quality of life in a high-burden setting. Int J Tubercul Lung Dis 13(12):1500–1506
Hwang YI, Kim JH, Lee CY, Park S, Park YB, Jang SH et al (2014) The association between airflow obstruction and radiologic change by tuberculosis. J Thoracic Dis 6(5):471
Ngahane BHM, Nouyep J, Motto MN, Njankouo YM, Wandji A, Endale M et al (2016) Post-tuberculous lung function impairment in a tuberculosis reference clinic in Cameroon. Respir Med 114:67–71
Pasipanodya JG, Miller TL, Vecino M, Munguia G, Garmon R, Bae S et al (2007) Pulmonary impairment after tuberculosis. Chest 131(6):1817–1824
Chushkin MI, Ots ON (2017) Impaired pulmonary function after treatment for tuberculosis: the end of the disease? J Bras Pneumol 43:38–43
Pasipanodya JG, Vecino E, Miller TL, Munguia G, Drewyer G, Fernandez M et al (2012) Non-Hispanic whites have higher risk for pulmonary impairment from pulmonary tuberculosis. BMC Public Health 12(1):1–10
Báez-Saldaña R, López-Arteaga Y, Bizarrón-Muro A, Ferreira-Guerrero E, Ferreyra-Reyes L, Delgado-Sánchez G et al (2013) A novel scoring system to measure radiographic abnormalities and related spirometric values in cured pulmonary tuberculosis. PLoS One 8(11):e78926
Chung K-P, Chen J-Y, Lee C-H, Wu H-D, Wang J-Y, Lee L-N et al (2011) Trends and predictors of changes in pulmonary function after treatment for pulmonary tuberculosis. Clinics 66(4):549–556
Di Naso FC, Pereira J, Schuh S, Unis G (2011) Functional evaluation in patients with pulmonary tuberculosis sequelae. Revista Portuguesa de Pneumologia (English Edition) 17(5):216–221
Patil S, Patil R, Jadhav A (2018) Pulmonary functions’ assessment in post-tuberculosis cases by spirometry: obstructive pattern is predominant and needs cautious evaluation in all treated cases irrespective of symptoms. Int J Mycobacteriol 7(2):128
Agarwala A, Maikap MK, Panchadhyayee P, Mandal P, Roy PP (2016) Chronic airway obstruction in post tubercular fibrosis cases: a serious lung function changes. Int J Res Med Sci 4:5294–5296
Gothi D, Shah D, Joshi J (2007) Clinical profile of diseases causing chronic airflow limitation in a tertiary care Centre in India. JAPI 55:551–555
Lam KBH, Jiang CQ, Jordan RE, Miller MR, Zhang WS, Cheng KK et al (2010) Prior TB, smoking, and airflow obstruction: a cross-sectional analysis of the Guangzhou biobank cohort study. Chest 137(3):593–600
Caballero A, Torres-Duque CA, Jaramillo C, Bolívar F, Sanabria F, Osorio P et al (2008) Prevalence of COPD in five Colombian cities situated at low, medium, and high altitude (PREPOCOL study). Chest 133(2):343–349
Lamprecht B, McBurnie MA, Vollmer WM, Gudmundsson G, Welte T, Nizankowska-Mogilnicka E et al (2011) COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest 139(4):752–763
Baig IM, Saeed W, Khalil KF (2010) Post-tuberculous chronic obstructive pulmonary disease. J Coll Physicians Surg Pak 20(8):542–544
Lee SW, Kim YS, Kim D-S, Oh Y-M, Lee S-D (2011) The risk of obstructive lung disease by previous pulmonary tuberculosis in a country with intermediate burden of tuberculosis. J Korean Med Sci 26(2):268–273
Allwood BW, Myer L, Bateman ED (2013) A systematic review of the association between pulmonary tuberculosis and the development of chronic airflow obstruction in adults. Respiration 86(1):76–85
Guo N, Marra F, Marra CA (2009) Measuring health-related quality of life in tuberculosis: a systematic review. Health Qual Life Outcomes 7(1):1–10
Osman R, Mortimer K, Bjune G, El Sony A (2016) Chronic respiratory disease in adults treated for tuberculosis in Khartoum, Sudan. Public health action 6(3):199–204
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
NA, MK MN, and HB jointly conceived the study and contributed to the data acquisition. NA contributed to the analysis and interpretation of the data. All authors reviewed the manuscript prior to submission and all accept responsibility for the integrity of the research process and findings. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by an Assiut University Ethics Committee and registered on clinicaltrials.gov (ClinicalTrials.gov Identifier: NCT05097638). Written informed consent was obtained from their next of kin, because of the patient’s critical condition.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdelaleem, N.A., Ahmed, M.K., Mohamed, M.N. et al. Lung health after tuberculosis: clinical and functional assessment in post-pulmonary tuberculosis Egyptian patients. Egypt J Bronchol 16, 23 (2022). https://doi.org/10.1186/s43168-022-00123-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-022-00123-z