Abstract
Background
Hypomagnesemia is a predictor of progression and mortality of chronic kidney disease (CKD) patients. However, limited data is available about the prevalence and kidney-related risk factors of hypomagnesemia in the CKD patients. We aimed to investigate the prevalence and risk factors of low serum magnesium level associated with proteinuria and its impact on CKD patients. This cross-sectional study enrolled 100 CKD patients with different stages according to estimated glomerular filtration rate (eGFR), divided into 2 groups (proteinuric and non-proteinuric) in the period from February 2020 to August 2020.
Results
The number of participants in this study was 100 subjects, 50 patients were proteinuric and 50 patients had no proteinuria. The study participants’ serum magnesium levels ranged from 1.2 to 2.7 mg/dL. Fourteen (28%) of proteinuric individuals had a serum magnesium level of less than 1.8 mg/dL. Hypomagnesemic patients had significantly higher urine albumin creatinine ratio (UACR) (2071 mg/g vs. 812 mg/g, P<0.001), significantly higher CRP (48 mg/L vs. 12 mg/L, P<0.001), and lower mean hemoglobin levels as well (10.4 g/dL vs. 10.91 g/dL, P= 0.044). Serum magnesium level showed negative correlation with UACR (r=−0.504, P<0.001), parathyroid hormone (r=−0.276, P=0.005), and CRP (r=−0.505, P<0.001).
Conclusions
Hypomagnesemia is a frequent electrolyte disorder in patients with CKD. Hypomagnesemia is independently associated with proteinuria. Hypomagnesemia is a risk factor of inflammation, anemia and hyperparathyroidism in pre-dialysis CKD population.
Similar content being viewed by others
Background
Magnesium is the second most significant intracellular cation and the fourth most common cation in the body [1]. In recent years, the awareness of magnesium has been increasing as it is implicated in multiple physiological functions of human cells [2]. Magnesium is involved in bone metabolism, adenosine triphosphate metabolism, neurotransmitter release, blood vessel tone, and cardiac rhythm [3,4,5]. Abnormal homeostasis of serum magnesium may occur in chronic kidney disease (CKD) and end-stage renal disease (ESRD) patients [6].
In early CKD stages (1–3), a rise in fractional magnesium excretion is compensating for the loss of kidney function, and serum magnesium levels are thus maintained within their normal ranges [7]. In late CKD stages (4–5), impairment of tubular reabsorption results in increase of the fraction excretion of filtered magnesium [8].
Although hypomagnesemia is clinically prevalent in CKD, it is reasonable to predict that it will be uncommon in patients with a low glomerular filtration rate (GFR). Its prevalence in these patients, however, is unknown. Furthermore, hypomagnesemia-related factors, particularly kidney-intrinsic risk factors, have not been thoroughly investigated.
Therefore, this study was conducted in the period from February 2020 to August 2020 aiming to assess the prevalence and risk factors of hypomagnesemia associated with proteinuria and its impact on chronic kidney disease patients.
Methods
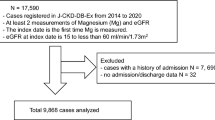
This is a cross-sectional study on 100 CKD patients with different stages according to estimated glomerular filtration rate (eGFR), divided into 2 groups (proteinuric and non-proteinuric) in the period from February 2020 to August 2020. CKD was defined according to The National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative (KDOQI) as the presence of kidney damage or glomerular filtration rate (GFR) of <60 mL/min/1.73m2 for ≥3 months. eGFR was estimated using CKD-EPI equation.
The study was approved by our University Hospital institutional ethical committee; written informed consent was taken from the patients to participate in this study.
CKD patients not on dialysis defined according to the KDOQI guidelines with age above 18 years old of both male and female sexes were included. We excluded any patient who had a history of chronic diarrhea, ileostomy or colostomy, patients with malignancy, on magnesium-based medications, and unwilling patients to participate.
All participants were submitted to history taking (diabetes mellitus, hypertension, CKD, drug history, previous operations), full physical examination, and investigations to fulfill inclusion and exclusion criteria including the following: serum creatinine (mg/dl), serum total magnesium level (mg/dl), serum albumin level (gm/dl), serum sodium level (mg/dl), serum potassium level (mg/dl), serum calcium level (total and ionized) (mg/dl), serum phosphorus level (mg/dl), intact parathyroid hormone (iPTH) (pg/ml), total cholesterol and triglycerides (mg/dl), UACR (mg/g), CRP (mg/L), and hemoglobin (gm/dl).
Serum magnesium values of less than 1.8 mg/dL were considered hypomagnesemia. The CKD-EPI equation was used to calculate the eGFR.
Results
The number of participants in this study was 100 subjects, 50 patients were proteinuric and 50 patients had no proteinuria. Fifty-three percent of the studied patients were males and 47% were female with mean age (in years) 50.64±13.48 in the proteinuric and 50.16 ± 11.31 in the non-proteinuric group (Table 1).
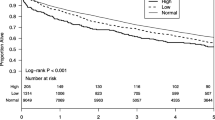
The serum magnesium levels ranged from 1.2 to 2.7 mg/dL in the study participants. Fourteen (28%) of proteinuric individuals had a serum magnesium level of less than 1.8 mg/dL (Table 2, Fig. 1).
Diabetic population are more likely to have hypomagnesemia as shown in (Table 3), 8 (57%) of hypomagnesemic patients were diabetic, 2 patients (14 %) were hypertensive, and 4 patients (22 %) were both diabetic and hypertensive. Compared with normomagnesemic patients, hypomagnesemic patients had significantly higher UACR (2071 mg/g vs. 812 mg/g, P<0.001) (Fig. 2), had significantly higher CRP (48 mg/L vs. 12 mg/L, P<0.001) (Fig. 3), much lower mean hemoglobin levels as well (10.4 g/dL vs. 10.91 g/dL, P= 0.044), had significantly low serum potassium (57.1% vs. 25.0%, P= 0.031), and lower serum sodium (35.7% vs. 8.3%, P= 0.030) (Table 4).
To investigate the parameters associated to serum magnesium levels, correlation analysis was used. Serum magnesium correlated positively with serum sodium (r=0.203, P=0.043), potassium (r=0.436, P<0.001), phosphorus (r=0.223, P=0.026), total albumin (r=0.246, P=0.014), although negatively correlated with UACR (r=−0.504, P<0.001) (Fig. 4), iPTH (r=−0.276, P=0.005), CRP (r=−0.505, P<0.001), and total cholesterol (r=−0.272, P=0.006) (Table 5).
Multivariate regression analysis was performed to determine the independent determinants of hypomagnesemia. UACR, CRP, serum potassium, and sodium were the independent predictors of hypomagnesemia (Table 6).
Discussion
Magnesium regulation and elimination in CKD patients is relatively understudied. Despite this gap in knowledge, we know that when the glomerular filtration rate (GFR) drops below 20–30 mL/min, serum magnesium levels rise; however, we do not know what happens to serum magnesium level in patients with CKD stages 1–3, GFR > 30 mL/min [9]. Therefore, this study was conducted in the period from February 2020 to August 2020 aiming to assess the prevalence and risk factors of low serum magnesium level associated with proteinuria and its impact on chronic kidney disease patients.
In the present study, the prevalence of hypomagnesemia among proteinuric patients was 28%. Oka et al. study was on about 5000 patients. The most frequent electrolyte abnormality was hypomagnesemia (14.7%), which had a similar prevalence among stages of CKD [10]. Another study conducted by Rao and Shariff on 100 CKD patients with type II DM, divided into 2 equal groups, proteinuric and non-proteinuric, showed about 6% of proteinuric group had hypomagnesemia (mean 2.09 ± 0.28 mg/dl) [11].
Proteinuric patients had significantly lower serum magnesium levels than non-proteinuric patients. This is in agreement with Corsonello et al., who studied diabetic patients with proteinuria and found a significant decrease in serum ionized magnesium compared to normoalbuminuria patients [12].
We found that the serum magnesium level was negatively correlated with UACR level. This is in agreement with Arpaci et al. [13], Corica et al. [14], and Corsonello et al. [12] who found that when compared to the non-proteinuria group, diabetic patients with proteinuria had a substantial drop in serum ionized magnesium. The association between hypomagnesemia and proteinuria may be explained by osmotic diuresis in proteinuric individuals, which leads in increased urinary magnesium excretion by the kidney.
There was no significant difference between the normomagnesimic and hypomagnesimic groups as regard the use of PPI or diuretics; this is in concordance with Koulouridis et al. [15], on their study on 804 well-matched inpatients, who found that use of proton-pump inhibitors prior to admission was not associated with hypomagnesemia. Van Ende et al. [16] studied 512 renal transplant recipients and concluded that use of proton-pump inhibitors was not a predictor of hypomagnesemia. Other studies show significant association between hypomagnesemia and PPI or diuretic use. Danziger et al. [17] who studied 11,490 patients admitted to an intensive care unit found that hypomagnesemia was disclosed exclusively in patients concurrently treated with both PPI and diuretics. Kim et al.’s [18] study on 1356 patients concluded that serum magnesium was lower (n = 112) in users of PPI than in nonusers (n = 1244). Concurrent treatment with cisplatin or carboplatin further exacerbated hypomagnesemia. Lindner et al.’s [19] study on 5118 emergency department patients showed that hypomagnesemia was significantly associated with the use of proton-pump inhibitor or both proton-pump inhibitors and diuretics. The difference between these studies may be due to different sample size, study design, duration of proton-pump inhibitors intake, and concomitant use of other drugs causing hypomagnesemia.
The current study showed that serum magnesium level was negatively correlated with PTH level. This is in agreement with Ohya et al. [20], who found that the serum magnesium level was significantly higher in patients with low PTH levels, and they also concluded that PTH levels had a significant negative correlation with the serum magnesium levels in their study on 1231 ESRD patients just prior to beginning HD in Japan (p < 0.01). Furthermore, the serum Mg level was an independent factor apart from the other factors regulating iPTH, and Mansour et al. [21] found that serum magnesium level was negatively correlated with iPTH (r=−0.253, P<0.05). Serum magnesium has an inhibitory effect on PTH release from parathyroid gland by binding to the calcium-sensing receptors, and both hypermagnesemia and severe hypomagnesemia can suppress PTH.
In our study, among proteinuric group, patients with hypomagnesemia were more anemic than patients with normal serum magnesium level. Consistent with these findings, Sakaguchi et al.’s [22] large cohort study from Japan on hemodialysis patients concluded that patients with hypomagnesemia were more anemic than normomagnesemia patients. In a cross-sectional study of Biyik et al. [23], they also found that low serum magnesium levels were significantly associated with anemia in non-dialysis CKD patients. Because serum magnesium is essential for many important enzymes included in energy metabolism and synthesis of cellular and nuclear proteins, hypomagnesemia might lead to reduction in energy production with subsequent low hemoglobin synthesis [24]. Also, hypomagnesemia is associated with a state of inflammation which is an important cause of anemia in CKD patients [25].
Magnesium has antioxidant and anti-inflammatory properties. Oxidative stress and inflammation accelerate the progression of CKD [26]. Hypomagnesemia triggers the synthesis of interleukin-1beta and tumor necrosis factor, as well as the expression of various proinflammatory factors [27, 28]. In our study, serum magnesium was negatively correlated with CRP. This agrees with a cross-sectional study involving 58 HD patients at the Sahraee Center of Shiraz, Iran; there was a significant negative correlation between serum magnesium levels and CRP [29]. Interestingly, hypomagnesemia in peritoneal dialysis patients were significantly associated with high CRP and malnutrition, all of which contributed to a higher risk of mortality through worsening cell health and increasing inflammation [30]. In a study of 98 HD patients, Liu et al [31] found a significant relationship between low serum magnesium levels and many cardiovascular risk factors, including inflammation as well as ischemic heart disease.
Our study has some limitations. The study only included 100 patients, which was a relatively small sample size. A large sample size would have further verified our findings. Our study was a cross-sectional in nature, with a single serum magnesium measurement that could change with time. We were also unable to investigate whether magnesium supplementation could improve inflammation, anemia, or hyperparathyroidism. For this, prospective randomized studies are required.
Conclusions
In conclusion, hypomagnesemia is a common electrolyte disorder in non-dialysis CKD population and is independently associated with proteinuria. Hypomagnesemia is a risk factor for inflammation, anemia, and hyperparathyroidism in pre-dialysis CKD population. It is not clear whether correcting hypomagnesemia in CKD population with diet or magnesium supplementations will help in retarding the progression of proteinuria and CKD. More prospective randomized studies with high number of patients are required.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CKD:
-
Chronic kidney disease
- eGFR:
-
Estimated glomerular filtration rate
- GFR:
-
Glomerular filtration rate
- iPTH:
-
Intact parathyroid hormone
- KDOQI:
-
Kidney Disease Outcomes Quality Initiative
- UACR:
-
Urine albumin creatinine ratio
References
Al Alawi AM, Majoni SW, Falhammar H (2018) Magnesium and human health: perspectives and research directions. Int J Endocrinol 2018:9041694
Laires MJ, Monteiro CP, Bicho M (2004) Role of cellular magnesium in health and human disease. Front Biosci 9(1-3):262–276
Byrd RP Jr, Roy TM, Byrd RP Jr et al (2003) Magnesium: its proven and potential clinical significance. South Med J 96(1):104. https://doi.org/10.1097/01.SMJ.0000049846.49028.8F
Volpe SL (2013) Magnesium in disease prevention and overall health. Adv Nutr 4(3):378S–383S
Shechter M (2010) Magnesium and cardiovascular system. Magnes Res 23(2):60–72
Kanbay M, Goldsmith D, Uyar ME, Turgut F, Covic A (2010) Magnesium in chronic kidney disease: challenges and opportunities. Blood Purif 29(3):280–292
van de Wal-Visscher ER, Kooman JP, van der Sande FM (2018) Magnesium in chronic kidney disease: should we care? Blood Purif 45:173–178. https://doi.org/10.1159/000485212
Massy ZA, Nistor I, Apetrii M, Brandenburg VM, Bover J, Evenepoel P, Goldsmith D, Mazzaferro S, Urena-Torres P, Vervloet MG, Cozzolino M, Covic A, Era-Edta OB (2016) Magnesium-based interventions for normal kidney function and chronic kidney disease. Magnes Res 29:126–140
Cunningham J, Rodríguez M, Messa P (2012) Magnesium in chronic kidney disease stages 3 and 4 and in dialysis patients. Clin Kidney J 5(Suppl 1):i39–i51. https://doi.org/10.1093/ndtplus/sfr166
Oka T, Hamano T, Sakaguchi Y (2019) Proteinuria-associated renal magnesium wasting leads to hypomagnesemia: a common electrolyte abnormality in chronic kidney disease. Nephrol Dial Transplant 34:1154–1162
Rao PP, Shariff MG (2015) Serum magnesium levels in type 2 diabetic patients with microalbuminuria and normoalbuminuria. Int J Sci Stud 3(4):11–15
Corsonello A, Ientile R, Buemi M et al (2000) Serum ionized magnesium levels in type 2 diabetic patients with microalbuminuria or clinical proteinuria. Am J Nephrol 20(3):187–192
Arpaci D, Tocoglu AG, Ergenc H, Korkmaz S, Ucar A, Tamer A (2015) Associations of serum magnesium levels with diabetes mellitus and diabetic complications. Hippokratia 19:153–157
Corica F, Corsonello A, Ientile R, Cucinotta D, Di Benedetto A, Perticone F et al (2006) Serum ionized magnesium levels in relation to metabolic syndrome in type 2 diabetic patients. J Am Coll Nutr 25:210–215
Koulouridis I, Alfayez M, Tighiouart H et al (2013) Out-of-hospital use of proton pump inhibitors and hypomagnesemia at hospital admission: a nested case-control study. Am J Kidney Dis 62(4):730–737. https://doi.org/10.1053/j.ajkd.2013.02.373
Van Ende C, van Laecke S, Marechal C et al (2014) Proton-pump inhibitors do not influence serum magnesium levels in renal transplant recipients. J Nephrol 27(6):707–711. https://doi.org/10.1007/s40620-014-0105-9
Danziger J, William JH, Scott DJ et al (2013) Proton-pump inhibitor use is associated with low serum magnesium concentrations. Kidney Int 83(4):692–699. https://doi.org/10.1038/ki.2012.452
Kim S, Lee H, Park CH et al (2015) Clinical predictors associated with proton-pump Inhibitor-induced hypomagnesemia. Am J Therapeut 22:14–21 [PubMed] [Google Scholar]
Lindner G, Funk G-C, Leichtle AB et al (2014) Impact of proton pump inhibitor use on magnesium homoeostasis: a cross-sectional study in a tertiary emergency department. Int J Clin Pract 68(11):1352–1357. https://doi.org/10.1111/ijcp.12469
Ohya M, Negi S, Sakaguchi T, Koiwa F, Ando R, Komatsu Y et al (2014) Significance of serum magnesium as an independent correlative factor on the parathyroid hormone level in uremic patients. J Clin Endocrinol Metab 99:3873–3878
Mansour HH, Mohamed RR, Khaled MF, Khalil EM (2018) Serum magnesium level in maintenance hemodialysis and cardiovascular calcification. Sci J Al-Azhar Med Fac, Girls 2:26–31
Sakaguchi Y, Fujii N, Shoji T, Hayashi T, Rakugi H, Isaka Y (2014) Hypomagnesemia is a signifcant predictor of cardiovascular and non-cardiovascular mortality in patients undergoing hemodialysis. Kidney Int 85(1):174–181
Biyik Z, Yavuz YC, Altintepe L (2020) Association between serum magnesium and anemia in patients with chronic kidney disease. Int Urol Nephrol 52(10):1935–1941
Zhan Y, Chen R, Zheng W, Guo C, Lu L, Ji X et al (2014) Association between serum magnesium and anemia: China health and nutrition survey. Biol Trace Elem Res 159(1–3):39–45
Maier JA, Malpuech-Brugere C, Zimowska W, Rayssiguier Y, Mazur A (2004) Low magnesium promotes endothelial cell dysfunction: implications for atherosclerosis, infammation and thrombosis. Biochim Biophys Acta 1689(1):13–21
Bash LD, Erlinger TP, Coresh J, Marsh-Manzi J, Folsom AR, Astor BC (2009) Inflammation, hemostasis, and the risk of kidney function decline in the Atherosclerosis Risk in Communities (ARIC) Study. Am J Kidney Dis 53:596–605
Shogi T, Miyamoto A, Ishiguro S, Nishio A (2003) Enhanced release of IL-1beta and TNF-alpha following endotoxin challenge from rat alveolar macrophages cultured in low-mg(2+) medium. Magnes Res 16:111–119
Shogi T, Oono H, Nakagawa M, Miyamoto A, Ishiguro S, Nishio A (2002) Effects of a low extracellular magnesium concentration and endotoxin on IL-1beta and TNFalpha release from, and mRNA levels in, isolated rat alveolar macrophages. Magnes Res 15(3-4):153–160
Pakfetrat M, Malekmakan L, Roozbeh J, Haghpanah S (2008) S. Magnesium and its relationship to C-reactive protein among hemodialysis patients. Magnes Res 21:167–170
Fein P, Suda V, Borawsky C et al (2010) Relationship of serum magnesium to body composition and inflammation in peritoneal dialysis patients. Adv Perit Dial 26:112–115
Liu F, Zhang X, Qi H et al (2013) Correlation of serum magnesium with cardiovascular risk factors in maintenance hemodialysis patients—a cross-sectional study. Magnes Res 26:100–108 15:147–152
Acknowledgments
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
BMM performed the laboratory investigations of the study. FMA analyzed and interpreted the patient data. AAE was a major contributor in writing the manuscript. RAA shared in the data analysis and interpretation and wrote and revised the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Zagazig University Hospital institutional ethical committee (IRB#:6048-12-4-2020); date of approval: 12-4-2020.
Written informed consent was taken from the patient to participate in this study.
Consent for publication
This was taken from the patients.
Competing interests
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdel-Hameed, A.R., Ahmed, M.F., Elsantawy, A.A. et al. Prevalence, risk factors and impact of proteinuria-associated hypomagnesemia in chronic kidney disease patients: cross-sectional study. Egypt J Intern Med 34, 25 (2022). https://doi.org/10.1186/s43162-021-00083-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43162-021-00083-8