Abstract
Background
A tongue abscess is a rare but serious condition marked by a localized accumulation of pus within the tongue’s tissues. Despite the tongue’s frequent exposure to trauma, bites, and foreign objects, it typically resists infections. However, an acute lingual abscess can be life-threatening due to the risk of airway obstruction from tongue swelling. Common symptoms include increasing pain, fever, swelling, immobility, edema, and redness of the tongue. The case report aimed to highlight the unusual clinical presentation and location of a deep-seated abscess in the anterior third of the tongue, as well as the radiographic approach to diagnosing the lesion.
Case presentation
A 30-year-old female patient presented with sudden onset tongue pain and swelling persisting for 4–5 days. Clinical examination revealed a solitary diffuse swelling in the anterior two-thirds of the tongue, approximately 3 × 2 cm in size. Diagnostic imaging, including a plain radiograph, ultrasound (USG), and MRI, was conducted. The patient was hospitalized for incision and drainage of the abscess, followed by a 5-day course of intravenous antibiotics.
Conclusions
A tongue abscess, though rare, is a serious condition indicated by tongue swelling, pain, fever, dysphagia, and dyspnea. Diagnosis involves physical examinations and imaging studies like ultrasound or MRI. Immediate treatment includes maintaining airway patency, draining the abscess, and administering broad-spectrum antibiotics. Prompt recognition and treatment are essential to prevent severe complications such as airway obstruction and sepsis. Regular follow-up ensures complete resolution and prevents recurrence.
Similar content being viewed by others
Background
An abscess of the tongue is a localized collection of pus that forms within the tissues of the tongue, while the tongue is frequently exposed to trauma, bites, and foreign objects; the occurrence of abscesses in the tongue is rare. This rarity can be attributed to several factors, including the presence of keratinized squamous epithelium, well-vascularized muscles, a rich lymphatic drainage system, and direct contact with saliva, which serves immune functions such as protection, lubrication, and continuous cleansing [1]. An acute lingual abscess is a potentially life-threatening condition because swelling of the tongue can quickly obstruct the airway. Symptoms typically include progressive pain, fever, tongue swelling and immobility, tongue edema, and redness [2]. Epidemiologically, lingual abscesses are more commonly associated with males, smokers, those who use dental prostheses, and individuals with poor oral hygiene. The underlying cause should be considered based on the location of the clinical presentation [3]. Abscesses in the anterior two-thirds of the tongue typically result from bites, local injuries, or foreign bodies, while those in the posterior third may be linked to lingual tonsils, remnants of the thyroglossal duct, or pathologies related to the first and second molars [1]. Despite its rarity and complexity, the management of this condition is relatively straightforward, with the primary treatment involving intravenous antibiotics and consideration given to surgical drainage as an adjunctive measure [4].
The case report aimed to highlight the unusual clinical presentation and location of a deep-seated abscess in the anterior third of the tongue, as well as the radiographic approach to diagnosing the lesion.
Case presentation
A 30-year-old female patient presented at the Department of Oral Medicine and Radiology, reporting a sudden onset of tongue pain and swelling persisting for 4 to 5 days. The swelling was initially small in size but noticeably increased over the last 2 days. Additionally, the patient mentioned experiencing difficulty swallowing (dysphagia) and impaired speech (dysarthria) for the past 3 days. The patient had sought medical attention at a local clinic, where she was subsequently admitted to the hospital. During her hospital stay, she received intravenous fluids (normal saline) and analgesics for the last 3 days before being referred to our department for further evaluation and treatment.
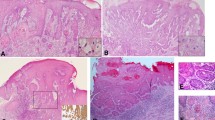
During the general examination, the patient appeared to be of thin build and malnourished. She was conscious, cooperative, and well-oriented with regard to time, place, and person. Upon clinical examination, a solitary diffuse swelling was observed in the anterior two-thirds of the tongue, measuring approximately 3 × 2 cm (Fig. 1). This swelling extended mediolaterally from the right lateral border of the tongue to the left lateral border and superior-inferiorly from 3 mm above the dorsum of the tongue to the base of the tongue, where it attaches to the floor of the mouth (Fig. 2). The overlying mucosa appeared to be of normal color with no signs of inflammation; it exhibited a slightly stretched and shiny surface, and there were no signs of depapillation on the dorsal aspect of the tongue. Upon palpation, all the observed findings regarding the site, size and extent were confirmed. The swelling was firm in consistency, tender on palpation, non-compressible, non-pulsatile, and non-fluctuant in nature.
For further evaluation, the patient underwent multiple examinations, including a plain radiograph, USG, and MRI. Occlusal mandibular cross-section radiograph reveals homogenous soft tissue density in the floor of the mouth. Ultrasonography revealed an irregular hypoechoic collection within an anechoic cavity measuring 2 × 2 cm in the intramuscular region of the tongue. There is no color uptake observed on color Doppler, giving the impression of a likely infection. Few subcentimetric lymph nodes in the bilateral submandibular regions noted with largest of size measuring 14 × 6 mm (Fig. 3).
MRI revealed a fairly defined peripherally enhancing collection measuring 2.2 × 1.6 × 3.1 cm noted involving the apex and part of body of ventral surface of the tongue (Fig. 4). Similar smaller pockets of collection are present adjacent to the larger collection. Perilesional significant STIR hyperintensity noted suggesting inflammatory changes and subcutaneous edema. Lesion appears isointense on T1WI and heterogeneous hyperintense on T2WI (Fig. 5). The collection was confined to the anterior half of the ventral surface of the tongue, giving the impression of abscess of the tongue. Few subcentimetric and enlarged lymphnodes are noted in bilateral level 1b with largest measures about 13 × 6 mm.
The patient was admitted to the hospital for incision and drainage followed by 5-day course of intravenous antibiotics, consisting of 1 g of Amoxicillin sodium + 200 mg of Clavulanate potassium administered via intravenous infusion three times a day for 5 days. Additionally, the patient received Metronidazole injections (5 mg/ml) of 100 ml twice a day for 5 days, along with analgesic IV Aceclofenac and Paracetamol injections (100 ml) twice a day for 5 days.
After 3 days, the patient noticed a progressive reduction in the size of the swelling, as well as an improvement in speech and the ability to swallow food. Consequently, the patient expressed a desire for an early discharge. After completing the full 5-day course, the patient was discharged from the hospital and scheduled for a follow-up appointment 10 days later.
The patient returned to our department for a follow-up visit after 15 days, reporting that the tongue swelling had completely subsided and there was a full recovery in swallowing and speech functions.
Discussion
A tongue abscess is an exceptionally rare condition due to the tongue’s remarkable resistance to infection, despite constant exposure to various potential pathogens. Several factors contribute to this resistance: the tongue’s continual mobility, which aids in producing a constant self-cleansing effect through saliva; its robust, keratinized mucosal covering, which acts as a barrier against microorganisms; the predominance of muscle tissue in its parenchyma, with a rich blood supply; an extensive network of lymphatic drainage; and the immunological properties of saliva [5]. When a person’s natural defense mechanisms are compromised, the likelihood of a tongue abscess increases. Factors such as compromised surface barriers, foreign objects, and immunodeficiency status make individuals more susceptible to tongue infections. The tongue’s mucosa can be compromised through pharmacological means, such as chemotherapeutic drugs, or through physical trauma. Once the initial line of defense is breached and the host’s immune system is compromised, tongue infections can become severe and challenging to treat. Even in healthy individuals, foreign objects can trigger an inflammatory response in the tongue, potentially leading to abscess formation. Recent literature reports have also highlighted a connection between tongue abscesses and body piercings [6].
The cause of a tongue abscess can vary depending on its location. The front two-thirds of the tongue, referred to as the “oral tongue,” is the mobile part situated in front of the circumvallate papillae. Glossal abscesses are more commonly found in the anterior part of the tongue and are typically unilateral. They are often linked to direct trauma, such as biting the tongue forcefully or injury from a sharp fish bone. On the other hand, the posterior area behind the circumvallate papillae is known as the "tongue base" and is considered part of the oropharynx. Abscesses in this region usually originate from lingual tonsillar lesions, infected thyroglossal duct cysts, or the spread of infections from the first or second molars [7].
Tongue abscesses come in two varieties: superficial and deep. Superficial abscesses manifest as inflammation just beneath the mucosal membrane, primarily occurring at the back of the tongue. These are characterized by tenderness, a dense and swollen appearance, and can be uncomfortable to touch. On the other hand, deep abscesses involve inflammation of the deeper tongue muscle tissue, resulting in a more severe clinical course. This typically includes symptoms like a body temperature of 38 to 39 degrees Celsius, general weakness, loss of appetite, and headaches. A thorough physical examination reveals a significant increase in tongue swelling, which can potentially interfere with speech and the ability to consume food [8].
In our case, the swelling of the anterior two-thirds of the tongue is attributed to an abscess collection in the deeper part of the ventral aspect of the tongue, likely involving the intrinsic muscle. The exact etiologic factor for this case is unknown based on the patient’s history and examination, although malnourishment can be considered as a predisposing factor.
Symptoms of an acute tongue abscess include deep tissue swelling or the presence of a lump in the tongue, pain that extends toward the ears, a throbbing localized pain, fever, challenges with swallowing, voluntary immobilization of the tongue due to pain, and, in advanced cases, difficulties in both breathing and swallowing [9].
The differential diagnosis encompasses various conditions that can present as tongue swelling, such as tumors, cysts, infarction, edema, infections, and hemorrhage. Additionally, metabolic macroglossia in conditions like hyperpituitarism or hypothyroidism, as well as developmental macroglossia in cases like lingual thyroid or ectopic lymphoid tissue, can also lead to tongue enlargement. It’s essential to include oral tubercular ulcers in the list of potential differentials for tongue abscess, especially considering that the tongue is a common site for oral tuberculosis involvement [10].
Ultrasonography, CT, and MR imaging are among the imaging techniques available for evaluating tongue swellings. However, using ultrasonography with a transducer in the mouth is challenging, even though it can effectively define and differentiate vascular lesions and abscesses. In ultrasonography, a lingual abscess typically appears as a hypoechoic lesion surrounded by a hyperechoic ring [8].
Computed tomography is particularly useful for precisely defining the anatomy of lesions located in the posterior part of the tongue and for distinguishing lesions that are external to the tongue’s musculature, such as those occurring in the sublingual spaces above or below the mylohyoid muscles [3].
MRI provides excellent soft tissue detail and multiplanar capability for visualizing the oral cavity, making it well suited for scanning the tongue and the floor of the mouth. Radiologic features of inflammatory processes can vary, with some appearing solid and others cystic [11]. In the case reported by Saro-Buendía et al. [5], which involved a lingual abscess located in the posterior part of the tongue, the T1WI images showed heterogeneous signal intensity, while the T2WI images exhibited hyperintense signal intensity. After the administration of intravenous contrast, the imaging revealed peripheral thick rim enhancement with surrounding edema and swelling.
In our study, USG and MRI were performed as the main diagnostic imaging modalities. USG revealed an irregular hypoechoic collection within an anechoic cavity in the intramuscular region of the tongue, while MRI showed perilesional significant STIR hyperintensity with isointensity on T1WI and heterogeneous hyperintensity on T2WI.
The management of tongue abscesses involves several key steps. Ensuring airway patency is a priority. Draining the abscess can be achieved through either needle aspiration or surgical incision. In cases where there is a suspicion of infected carcinoma, a biopsy of the abscess wall may be necessary to rule out this diagnosis. Administering antibiotic therapy should be guided by the results of gram staining and culture of the abscess drainage. Initially, empirical therapy should target streptococci and oral gram-negative anaerobes. Given the increasing resistance of oral Bacteroides species to penicillin, an appropriate choice would be a single antibiotic like clindamycin, or a combination of ampicillin/clavulanic acid, or penicillin along with metronidazole. Once the patient’s clinical condition stabilizes, it is important to conduct a dental evaluation [3].
Conclusions
Tongue abscess is a rare but serious condition that must be considered when there is tongue swelling. Symptoms include pain, fever, dysphagia, and dyspnea. Diagnosis involves physical examination and imaging studies like ultrasound or MRI scans. Immediate management includes ensuring airway patency, incision and drainage of the abscess, and administering broad-spectrum antibiotics targeting both gram-positive and gram-negative anaerobes. Prompt recognition and treatment are crucial, as a tongue abscess can lead to severe complications such as airway obstruction and sepsis. Regular follow-up is necessary to ensure complete resolution and prevent recurrence.
Availability of data and materials
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- CT:
-
Computed tomography
- USG:
-
Ultrasonography
- MRI:
-
Magnetic resonance imaging
References
Carvalho TBO, Fernandes AM, Sanches RA (2012) Tongue abscess: case report. Int Arch Otorhinolaryngol 16(1):126–129. https://doi.org/10.7162/S1809-48722012000100019
Bertolini G, Bruschi A, Meraviglia I, Gazzano G, Avigo C, Luzzago F (2016) Abscess of the tongue evolution and treatment of an emergency. Clin Surg. https://doi.org/10.25107/2474-1647.1143
Sanders JL, Houck RC (2024) Dental abscess. (2023) In: StatPearls. StatPearls Publishing, Treasure Island
Pallagatti S, Sheikh S, Kaur A, Puri N, Singh R, Arya S (2012) Tongue abscess: a rare clinical entity. J Investig Clin Dent 3(3):240–243. https://doi.org/10.1111/j.2041-1626.2011.00101.x
Saro-Buendía M, Suarez Urquiza P, Amigo González J, Lesmas Navarro MJ, Mazón M, Armengot Carceller M (2023) Posterior lingual abscess: report of two cases. Arch Acad Emerg Med. 11(1):e18. https://doi.org/10.22037/aaem.v11i1.1860
Olsen JC (2001) Lingual abscess secondary to body piercing. J Emerg Med 20(4):409. https://doi.org/10.1016/s0736-4679(01)00307-9
Ozturk M, Mavili E, Erdogan N, Cagli S, Guney E (2006) Tongue abscesses: MR imaging findings. AJNR Am J Neuroradiol 27(6):1300–1303
Mesfin T, Debele G, Seyoum K, Dadi S, Tsegaye M, Gomora D, Kene C, Tolosa G (2022) Tongue abscess: a case report. Int Med Case Rep J. 15:769–772. https://doi.org/10.2147/IMCRJ.S399020
Antoniades K, Hadjipetrou L, Antoniades V (2004) Acute tongue abscess. Report of three cases. Oral Surg 97(5):570–573. https://doi.org/10.1016/j.tripleo.2003.11.011
Byahatti SM, Ingafou MSH (2011) Lingual abscess—a rarity. J Clin Exp Dent 3(2):e162-165
Mesolella M, Allosso S, Iorio B, Motta G (2021) Clinical and diagnostic aspect of tongue abscess. Ear Nose Throat J 100(10):1012S-1014S. https://doi.org/10.1177/0145561320933961
Acknowledgements
Not applicable.
Funding
The role of funding body in the design of the study and collection, analysis and interpretation of data and in writing the manuscript done by corresponding author Dr. Anusha Rudrakshi.
Author information
Authors and Affiliations
Contributions
AR collected data for study and wrote majority of the main draft, PR did data analyzing and designing of the study, PR finallized the deseign and NS completed writing the paper and helped in analysing the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Consent from the patient has been obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rudrakshi, A., Ramdurg, P. & Naveen, S. Swollen speech: a case study of tongue abscess detected via imaging technology. Egypt J Radiol Nucl Med 55, 158 (2024). https://doi.org/10.1186/s43055-024-01325-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01325-9