Abstract
Background
Among pediatric surgical procedures, hypospadias surgery is one of the most difficult. The most prevalent complication following hypospadias repair is urethrocutaneous fistula. Numerous procedures have been developed to prevent and resolve this issue. One such method is platelet-rich fibrin (PRF) membrane preparation, which is a straightforward process requiring only the patient’s serum. It has already been utilized successfully in plastic and reconstructive surgeries, where it significantly enhances the healing capacity and decreases the risk of infections. The purpose of this study is to assess the efficacy of an autologous PRF membrane in promoting healing and reducing fistula occurrence in cases of de novo distal hypospadias.
Methods
Forty patients with primary distal hypospadias underwent TIP repair, as a part of a prospective controlled randomized study from April 2017 to February 2018. The cases were randomly allocated into two categories. TIP repair done in all cases by the same surgeon. Twenty cases comprised group A, which utilized a preputial or local dartos flap as an additional protective layer over the urethroplasty. In contrast, group B comprised 20 cases in which the urethroplasty was covered with a PRF membrane. The initial follow-up duration was 6 months. Each group’s fistula incidence and other associated complications were documented.
Results
Two groups were compared during the initial 6-month follow-up period. There were seven cases of urethrocutaneous fistula in group A, representing a 35% incidence rate. In group B, there were two cases that had fistula with an incidence of 10% in the early postoperative period. Two patients (10%) in group A developed meatal stenosis and only one patient in group B (5%) developed meatal stenosis. Glandular dehiscence occurred in one patient (5%) in group B. There was no skin wound infection in both groups.
Conclusion
The PRF membrane may be a promising method as a coverage layer over the urethroplasty aiming to reduce the fistula rate after the repair. A larger comparative study is needed to evaluate the efficacy of PRF membranes in promoting wound healing.
Similar content being viewed by others
Background
Hypospadias occurs due to inadequate tubularization of the urethra during embryonic development, so the urethral meatus is improperly positioned on the under surface of the penis The incidence is approximately 1/300 live male births [1]. The anatomic presentation can be classified according to the position of the meatus. It is classified as anterior or distal (glandular, coronal, or subcoronal; 60–65% of cases), middle (midpenile; 20–30% of cases), or posterior or proximal (posterior penile, penoscrotal, scrotal, or perineal;10–15% of cases) [2]. Despite advancements in surgical techniques for the management of hypospadias, the principles of any surgery; to provide a child with a straight penis and a terminal or near terminal meatus, that is cosmetically and functionally acceptable with little morbidity have not changed [3]. The most popular method currently utilized for hypospadias repair is Snodgrass TIPU, which has significantly improved the outcome of hypospadias repair, particularly in distal cases [4].
Urethrocutenous fistula (UCF) is one the most common complications after hypospadias repair with a varying incidence of 4–20%. The success of repair depends on basic principles such as correction of distal urethral obstruction, tension-free anastomosis, closure with absorbable suture material, covering the urethral repair with a well-vascularized tissue and interposing a waterproofing layer between urethral and skin closures [5].
PRF is a new generation of platelet concentrate, that promotes angiogenesis and wound healing. It fights infections by promoting immune response. PRF stimulates fibroblast proliferation and collagen biosynthesis ability. It is commonly known that platelet-rich fibrin plays a significant role in oral, palatal, and maxillofacial surgery [6, 7]. In theory, platelets are caught within a fibrin mesh [8]. Vascular endothelial growth factor, platelet-derived growth factor, transforming growth factor, and epidermal growth factor are just a few of the beneficial growth factors found in the granules found inside platelets that help to accelerate the healing process [9].
The purpose of the current study was to assess the impact of incorporating PRF as a protective layer during distal hypospadias repair by measuring the incidence of fistulas following TIP repair.
Methods
This study was designed as a randomized control study during the period from April 2017 to February 2018. The study was done after approval from the Research Ethical Committee of Cairo University Teaching Hospitals. An informed written consent was obtained from the guardians of the patients.
Inclusion criteria were of children with primary distal penile hypospadias at ages of 6 months or more and with minimal or no chordee. Children with redo hypospadias, significant chordee (30% or more), circumcised patients, and proximal hypospadias were excluded.
Seventy-three patients were examined in the hypospadias clinic at Cairo University Specialized Pediatric Hospital. Forty-three patients met the inclusion criteria, 30 cases were excluded (11 patients with midpenile hypospadias, 9 patients with proximal hypospadias, 7 cases with recurrent hypospadias and 3 cases were circumcised). There were also 3 cases that met inclusion criteria however were lost during follow-up.
The study included 40 patients with primary distal type of hypospadias. Using computer-based randomization, eligible patients were randomized 1:1 to receive either dartos flap (group A) or PRF (group B) as a first covering layer over repair. The mean age at the time of surgery was 27.1 ± 17.7 (ranging from of 6 to 61) months in group A, while 24.8 ± 19.2 (range of 6 to 67) months in group B. All cases were performed by the same surgeon using TIP urethroplasty.
Operative procedure of TIP repair
Under general anaesthesia, with a caudal block, and using a magnifying loupe, a glandular stay suture was placed in the midline along the axis of the penis, and used for traction. A circumferential, subcoronal incision was started dorsally and extended ventrally to join the limbs of the U-shaped incision surrounding the hypospadiac meatus. The penis was degloved, with the creation of a well-vascularised dartos tissue flap extending proximally to the root of the penis. The flap was then separated from the overlying preputial and penile skin. An artificial erection was performed to assess any residual chordee. The urethral plate was then incised, starting from within the hypospadiac meatus to just proximal to the glans tip. The incised plate was then tubularised over a 6–8-F stent, with a one-layer running subepithelial suturing using 6–0 polyglactin (vicryl). Tubularisation was extended to the midglans to obtain a wide meatus. The glans wings were deeply dissected laterally to allow a tension-free closure.
Group A patients (the control group)
Twenty patients with preputial or local dartos flap over the urethroplasty.
Group B patients (the study group)
Twenty patients with application of PRF membrane as a second layer over the urethroplasty.
PRF preparation
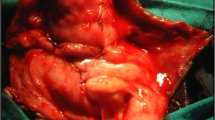
The PRF was prepared by withdrawing 5 ml of venous blood and transferring it to a sterilized plastic tube with no additives. The tube was placed in the centrifuge at a speed of 3500 rpm for 20 min (Fig. 1). After centrifugation, three layers were obtained from the serum. These layers were; red layer consists of red blood cells at the bottom; the uppermost layers consist of plasma without cells and the middle layer consists of PRF (Fig. 2).
After PRF preparation, it was separated from other attached layers and placed over a piece of gauzed then squeezed gently to obtain the flat layer that could be fixed over the repair. The final step was to fix the layer over the repair which was achieved by overlying the PRF extract directly over the repair and fixation in the four corners by Vicryl 6–0 sutures was applied (Fig. 3).
Direct skin closure was done. Simple gauze dressing is applied and the patients kept on oral antibiotics for the duration of the indwelling stent (7 days), dressing removed on the 3rd day.
Follow-up
The patients were examined at the time of catheter removal at the outpatient clinic and then weekly for 1 month. Follow-up was continued monthly for the next 5 months then every 6 months for 1 year. Followed by annual evaluation for 2 years.
On follow-up evaluation, we assessed the meatus (position, size, shape). Mothers or children were asked about the quality of the urine stream, its caliber, the presence of any voiding problem or leakage, and their satisfaction.
We recorded incidence and type of complications such as fistula, meatal stenosis, wound dehiscence, breakdown, or unfavorable cosmetic outcome.
Successful repair was considered when there was complete healing with no fistula, a meatus that appeared normal at the tip of the penis, normal-looking penile shaft skin without any deviations, and normal voiding force and diameter.
Results
In this study, a total of 40 patients with distal hypospadias underwent TIP repair. As regards the location of hypospadias meatus, coronal meatus in 8 patients (20%), sub-coronal meatus in 17 patients (42.5%), and anterior penile meatus in 15 patients (37.5%). The two groups underwent initial follow-up for an average of 6 months, with a range of 2 to 10 months.
In the early postoperative period, there were 7 cases of urethrocutaneous fistula (35%) in group A, while 2 patients (10%) were in group B (P value 0.127). After 6 months of follow up the two cases of fistula in group B closed spontaneously (0%) while not in group A (35%), (P value 0.008) which is statistically significant. The 7 cases of fistula in group A required surgical repair, there was no recurrence of fistula in all cases by follow-up.
Two patients (10%) in group A developed meatal stenosis and only one patient in group B (5%) developed meatal stenosis. Glandular dehiscence occurred in one patient (5%) in group B. No skin infections were encountered in either group.
Discussion
The aim of surgical correction is to restore the penis’s normal appearance and function. An appropriately directed urine stream and an erected penis should be the outcomes of surgical urethroplasty [10]. The Snodgrass tubularized incised plate (TIP) urethroplasty has become a primary technique for the repair of distal and midpenile hypospadias. Although many techniques have been introduced for the treatment of hypospadias, urethrocutaneous fistula (UCF) and meatal stenosis, which are the most frequent complications requiring reoperation [11]. Numerous methods for the covering of the urethroplasty have been reported, such as dartos, extragenital tissues, tunica vaginalis, and local subcutaneous penile tissue. Furthermore, fibrin sealants were developed to decrease the occurance of fistulas [12].
Additionally, fibrin sealant and other homologous fibrin materials are utilized to provide a sustaining layer over urethral repair. Fibrin sealants have been utilized as a topical agent for hemostasis and adhesive in tissue approximation during numerous surgical procedures [13]. Kinahan and Johnson were the first to document the application of fibrin sealant during hypospadias surgery [14]. Then, Ambriz-Gonzales et al. propose that fibrin sealant reduces the incidence of urethrocutaneous fistula following hypospadias repair [15]. Nevertheless, Gopal et al.’s largest series demonstrated that fibrin glue could reduce the incidence of fistula formation without completely eliminating the risk of recurrence [13]. Commercial sealants are extracted from the plasma derived from multiple donors so it carries a high risk of blood-borne infections [16]. Allergic reactions are reported after using this material, so the use of an autologous edition from this fibrin material emerged as a solution for these complications.
The utilization of single-donor fibrin sealant for urethrocutaneous fistula repair was suggested by Kajbafzadeh et al. [16]. In their study, they acquired fibrin sealant from a single donor using cryoprecipitation, centrifugation, and incubation.
PRF is utilized as an additive material for TIP repair in this study. PRF is an innovative platelet concentrate that facilitates wound healing and angiogenesis. It resists and combats infection while also contributing to the immune response to damage. PRF enhances the collagen biosynthetic capacity of normal human dermal fibroblasts and promotes their proliferation [17]. Fibrin comprises an assortment of growth factors, including platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), and fibroblast growth factor-basic (FGF-b) [18]. Choukroun et al. were the first to document PRF, and since then, it has been implemented in a number of reconstructive and oral surgical procedures [18].
In our current study, we evaluated the usage of the autologous platelets-rich fibrin membrane as a coverage layer in cases of primary distal hypospadias surgeries to decrease the incidence of fistula formation in comparison with the dartos flap coverage layer. The study included 40 patients with primary distal type of hypospadias. Eligible patients were divided into 2 groups to receive either dartos flap (group A) or PRF (group B) as a first covering layer over repair.
In the current study, there were 7 cases of urethrocutaneous fistula (35%) in group A, while 2 patients (10%) in group B. After 6 months of follow-up the two cases of fistula in group B closed spontaneously (0%) while not in group A (35%). The 7 cases of fistula in group A required surgical repair, there was no recurrence of fistula in all cases during the follow-up.
Our findings were consistent with Fouad et al., who enrolled 30 children ages varied from 1 to 6 years, and the success rate was 93.3%, with a complication rate of 6.7%. Our complications in group B using PRF were 10% fistula and 5% meatal stenosis. Foud et al. found that utilizing a platelet-rich fibrin membrane as an intermediate layer for hypospadias surgery in Tubularized Incised Plate Urethroplasty is a feasible and safe option, additionally, the procedure is simple and swift, with few postoperative complications; however, their cases were primary not redo [19].
In another study, Mahmoud et al. reported an overall success rate of 85.6%, which is higher than the current study, and could be attributed to the small number of patients in the current work. However, regarding the urethrocutaneous fistula [UCF] our study findings were similar to 10.0% of the PRF group [20].
Guinot et al. found that the PRF appears to be an effective and safe covering technique. It is a supplementary method to coverage for hypospadias repair surgery [21].
Hassouna et al. found that using Mathieu or Snodgrass procedures to control hypopadias resulted in a 20.0% complication risk. A fistula was the most frequent consequence, with wound breakdown recorded in 5.0%, meatal stenosis in 5.0%, and fistula in 10.0% of cases. Their study included patients as old as 15 years old. Although there were age differences and the absence of the second intermediate layer compared to the current study, our results were higher. This may be due to using different techniques [22].
Our study’s limitation was the relatively small number of patients. To validate our hypothesis, additional randomized comparative studies will be required to determine whether the autologous membrane is truly superior to other tissue-covering flaps or when used in conjunction with them. Furthermore, this method may be considered for re-do cases, circumcised hypospadias, debilitated cases with insufficient covering tissues, and cases lacking a healthy covering layer.
Conclusion
The PRF membrane may be a promising method as a coverage layer over the urethroplasty aiming to reduce the fistula rate after the repair. A larger comparative study is needed to evaluate the efficacy of PRF membrane in promoting wound healing.
Availability of data and materials
The raw data supporting the conclusion of this article will be made available by the authors, available upon request.
Abbreviations
- TIP:
-
Tabularized incised plate
- TIPU:
-
Tabularized incised plate urethroplasty
- PRF:
-
Platelet rich fibrin
- UCF:
-
Urethrocutaneous fistula
- RPM:
-
Round per minute
References
Yildiz T et al (2012) Age of patient is a risk factor for urethrocutaneous fistula in hypospadias surgery. J Pediatr Urol. 9:900–903
Leung ARC et al (2007) Hypospadias: an update. Asian J Androl 9:16–22
Steven L et al (2013) Current practice in paediatric hypospadias surgery: a specialist survey. J Pediatr Urol 9:1477–5131
Snodgrass WT (2012) Hypospadias. In: Wein AJ, Kavoussi LR, Novick AW, Partin AW, Peters CA (eds) Campbell-Walsh urology, 10th edn. Elsevier Saunders, Philadelphia, pp 3502–3605
Springer A (2014) Assessment of outcome in hypospadias surgery –a review. J Front Pediatr 2(2):1
Diss A, Dohan DM, Mouhyi J (2008) Osteotome sinus floor elevation using Choukroun’s platelet-rich fibrin as grafting material: a 1-year prospective pilotstudy with microthreaded implants. Oral Surg J 105:572–579
Eshghpour M, Dastmalchi P, Nekooei AH (2014) Effect of platelet-rich fibrin on frequency of alveolar osteitis following mandibular third molar surgery: a double-blinded randomized clinical trial. J Oral Maxillofac Surg 72:1463–1467
Dohan DM, Choukroun J, Diss A (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg J 101:37–44
Su CY, Kuo YP, Tseng YH (2009) In vitro release of growth factors from platelet-rich fibrin (PRF): a proposal to optimize the clinical applications of PRF. Oral Surg J 108:56–61
González R, Lingnau A, Ludwikowski BM (2018) Results of onlay preputial flap urethroplasty for the single-stage repair of mid- and proximal hypospadias. Front Pediatr 8(6):19
Snodgrass W, Bush N (2014) Recent advances in understanding/management of hypospadias. F1000Prime Rep 6:101. https://doi.org/10.12703/P6-101
Hosseini J, Kaviani A, Mohammadhosseini M, Rezaei A, Rezaei I, Javanmard B (2009) Fistula repair after hypospadias surgery using buccal mucosal graft. Urol J 6(1):19–22
Gopal SC, Gangopadhyay AN, Mohan TV, Upadhyaya VD, Pandey A, Upadhyaya A, Gupta DK (2008) Use of fibrin glue in preventing urethrocutaneous fistula after hypospadias repair. J Pediatr Surg 43:1869–1872
Kinahan TJ (1992) Tisseel in hypospadias repair. Can J Surg 35:75–77. PMID: 1739899
Ambiriz Gonzalez G, Velazquez-Ramirez GA, Gracia-Gonzalez JL, de León-Gómez JM, Muciño- Hernández MI, González-Ojeda A, Basterra JV (2007) Use of fibrin sealant in hypospadias repair reduces the frequency of postoperative complications. Urol Int 78:37–41
Kajbafzadeh A, Abolghasemi H, Eshghi P, Alizadeh F, Elmi A, Shafaattalab S, Dianat S, Amirizadeh N, Mohseni MJ (2010) Single-donor fibrin sealant for repair of urethrocutaneous fistulae following multiple hypospadias and epispadias repairs. J Pediatr Urol 7:422–427
Lundquist R, Dziegiel MH, Agren MS (2008) Bioactivity and stability of endogenous fibrogenic factors in platelet-rich fibrin. Wound Repair Regen 16:356–63
Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J, Dohan DM (2006) Platelet rich fibrin (PRF): a second generation platelet concentrate. Part IV: clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e56-60
Fouad Al-Awadi AS, Megahed HA, Ahmed Shahin MM, Abdul Aziz FA (2021) The use of autologous platelet rich fibrin membrane as a second layer in snodgrass repair of distal hypospadias. Int J Med Arts 3(2):1377–1383
Mahmoud AY, Gouda S, Gamaan I, Baky Fahmy MA (2019) Autologous platelet-rich plasma covering urethroplasty versus dartos flap in distal hypospadias repair: a prospective randomized study. Int J Urol 26(4):475–480
Guinot A, Arnaud A, Azzis O, Habonimana E, Jasienski S, Frémond B (2014) Preliminary experience with the use of an autologous platelet-rich fibrin membrane for urethroplasty coverage in distal hypospadias surgery. J Pediatr Urol 10(2):300–305
Hassouna AA, Arnous AA, Taman EA, Elsayaad IM (2020) Comparative study between Mathieu repair and Snodgrass repair in distal hypospadias. IJMA 2(3):508–518
Acknowledgements
The authors greatly appreciate the input of the professors at Cairo University Specialized Pediatric Hospital for their experience and guidance which served as the basis for the procedures presented in this research.
Funding
The authors declare there are no funding resources for this research.
Author information
Authors and Affiliations
Contributions
MT contributed to the conception and design of the study. KS and OA organized the database. MT and SK wrote the first draft of the manuscript. OA wrote sections of the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by Cairo University ethical committee. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Consent for publication
Written informed consent was obtained from the patient for publication of this research and accompanying images. A copy of the written consent is available for review upon request.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdelazim, O., Abdullateef, K.S., Khedr, E. et al. The use of an autologous platelet-rich fibrin membrane in urethroplasty for cases of distal hypospadias. Egypt Pediatric Association Gaz 72, 58 (2024). https://doi.org/10.1186/s43054-024-00304-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-024-00304-z