Abstract
Background
Recently, coronary artery bypass graft (CABG) techniques, both on-pump (ONCABG) and off-pump (OPCABG), were compared to seek the most effective approach to reduce the cost of prolonged intensive care unit length of stay (ICU LOS) and mortality. This study aims to compare ICU LOS and mortality in ONCABG and OPCABG.
Results
Demographic data of 1569 patients show the variance of characteristics. The analysis shows significant and longer ICU LOS in OPCABG than ONCABG (2.151 ± 0.100 vs. 1.573 ± 0.246 days; p = 0.028). Similar results were demonstrated after adjustment of covariates effects (3.146 ± 0.281 vs. 2.548 ± 0.245 days; p = 0,022). Logistic regression shows no significant difference in mortality in OPCABG and ONCABG, both in the unadjusted (OR [CI 95%] 1.133 [0.485–2.800]; p = 0.733) and the adjusted models (OR [CI 95%] 1.133 [0.482–2.817]; p = 0,735).
Conclusion
ICU LOS was significantly longer in OPCABG patients than in ONCABG patients in the author's centre. There was no significant difference in mortality between the two groups. This finding highlights a discrepancy between recently published theories and the practices observed in the author's centre.
Similar content being viewed by others
Background
Cardiovascular disease (CVD) has become the leading cause of death globally in developed and developing regions. Among various CVDs, coronary artery disease (CAD) has emerged as the most prevalent subtype, contributing significantly to the burden of CVD-related morbidity and mortality. To manage advanced CAD, coronary artery bypass graft (CABG) surgery has been widely adopted as a crucial therapeutic option aimed at improving survival rates and enhancing the quality of life for affected individuals.
Traditional CABG surgery involves cardiopulmonary bypass (on-pump CABG), temporarily stopping the heart and allowing surgeons to perform grafting procedures. At the same time, blood circulation is maintained through a heart–lung machine. However, in the early 1990s, an alternative technique called off-pump CABG (OPCABG) was introduced to reduce potential complications associated with on-pump CABG, such as systemic inflammatory response syndrome and neurocognitive deficits [1]. OPCABG allows surgeons to perform bypass grafting while the heart is still beating, thereby avoiding cardiopulmonary bypass and its associated risks.
The choice between on-pump and off-pump CABG remains controversial among cardiovascular surgeons and researchers. Numerous studies have investigated the outcomes and advantages of both techniques, leading to conflicting results. Some studies have reported comparable long-term survival rates, intensive care unit (ICU) length of stay, and perioperative mortality between on-pump and off-pump CABG [2, 3]. On the other hand, other studies have suggested potential benefits of one technique over the other regarding reduced complications and improved patient outcomes [4, 5].
In light of the existing controversies surrounding on-pump and off-pump CABG, our study aims to investigate and compare ICU length of stay and mortality outcomes between these two techniques in the Indonesian patient population. Our study distinguishes itself from previous publications by examining a specific patient population and providing contradictory findings to the commonly reported outcomes. Our results have the potential to significantly impact clinical decision-making by challenging the prevailing perceptions and guiding surgeons towards a more individualized approach in the management of advanced CAD.
Methods
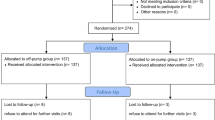
This is a retrospective observational study. Secondary data were collected from medical records of post-CABG patients from June 2010 until January 2014. Ethics approval and waiver of consent were granted by the Ethical Committee Board of National Cardiovascular Center Harapan Kita Hospital No.0449/UN2.F1/ETIK/2016. Consent was waivered because this study only used secondary data, which involved no risk to the subject.
Patients with a confirmed diagnosis of advanced CAD who underwent either on-pump or off-pump CABG surgery were included in the study. We excluded patients with the following condition: (1) cardiogenic shock, (2) on intra-aortic balloon pumps, (3) severe comorbidities that could significantly impact outcomes (malignancies, end-stage renal disease, advanced liver disease), and (4) incomplete medical records.
Descriptive statistics were reported for all variables of interest. Mean and standard deviation were reported for continuous outcomes. Frequency and percentages were reported for categorical outcomes. Logistic regression models were used to determine the death probability between on-pump coronary artery bypass graft (ONCABG) and off-pump coronary artery bypass graft (OPCABG) patients. The odds ratios were computed using the ONCABG group as the reference. Generalized linear models were fitted assuming gamma-distributed errors and a natural log link function to compare intensive care unit length of stay (ICU LOS) between the two groups. The distribution was chosen due to the skewness of the data. All models were fitted in bivariate and multivariate forms to account for the multiple factors that might affect the dependent variables. The factors considered in the adjusted models were age, sex, race, ejection fraction, and comorbidities such as high blood pressure, diabetes, and obesity. Statistical significance was determined at the level of 0.05.
Results
Demographic characteristics
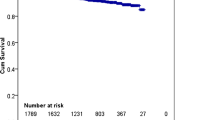
A total of 1569 subjects were included in this study. The demographic characteristics of the subjects are presented in Table 1. The majority of samples were males (87.00%). Age was classified into early adult (20–39 years old), middle adult (40–59 years old), late adult (60–65 years old), and old age (> 65 years old). The majority of the subject classified as middle adults was 875 (55.77%), followed by late adults at 358 (22.82%), old age at 316 (20.14%), and the last early adult at only 20 (1.27%). A total of 385 patients (24.54%) had diabetes. Total ONCABG procedures were 1278 (81.45%), and OPCABG was 291 (18.55%). Intensive care unit length of stay (ICU LOS) was classified into short (≤ 2 days) and prolonged (> 2 days). Short ICU LOS was observed in 1115 cases (71.06%), and only 454 cases (28.94%) had prolonged ICU LOS. Mortality among CABG patients was 44 (2.8%) from the 1569 data collected. Among the 44 patients who died, nine were in the OPCABG group, and 35 were in the ONCABG group (Table 2).
Analysis of ICU length of stay and mortality
We found a significantly longer ICU LOS in OPCABG patients (2.151 ± 0.100 days) compared to ONCABG patients (1.573 ± 0.246 days) with a p-value of 0.028. Similar results were found when the models were adjusted for the effects of covariates, with an adjusted mean of ICU LOS of 3.146 (SD = 0.281) for OPCABG patients and 2.548 (SD = 0.245) for ONCABG patients. Analysis results of the CABG technique and ICU LOS are presented in Table 3. The analysis of the CABG technique and mortality by using logistic regression models shows that there was no significant difference in mortality between OPCABG and ONCABG patients both in the unadjusted model (OR 1.133, CI 95% 0.485–2.8) and the adjusted model (OR 1.133, CI 95% 0.482–2.817). Analysis results of the CABG technique and mortality are presented in Table 4.
Discussion
Intensive care unit length of stay in OPCABG and ONCABG
Our study found that the length of stay in the intensive care unit was significantly longer for patients who underwent OPCABG than those who underwent ONCABG. This finding highlights a discrepancy between recently published theories and the practices observed in our study centre. We reviewed the literature to explain this phenomenon. We identified several problems associated with the CABG procedure regardless of the technique, including transient left ventricular dysfunction, capillary leak, warming from hypothermia, and emergence from anaesthesia [6].
Despite advancements in surgical procedures and myocardial protection measures, the prevalence of transient left ventricular systolic failure remained consistent over the years [6]. OPCABG was expected to mitigate myocardial damage by reducing the inflammatory response. However, it is important to note that it does not entirely eliminate inflammation caused by surgical trauma and anaesthetic drugs. The increased systemic vascular resistance observed after surgery is likely due to decreased ventricular function rather than the primary cause of decreased cardiac contractility. Inflammation-induced generation of oxygen-free radicals and release of proteolytic enzymes damage endothelial cells, leading to capillary leak syndrome. Hypothermia affects coagulation, increases systemic vascular resistance, and contributes to oxygen consumption and carbon dioxide generation.
The advantages of OPCABG over ONCABG, such as avoiding the inflammatory effects of cardiopulmonary bypass (CPB), minimizing transient left ventricular dysfunction, and reducing capillary leak, suggest that issues with the anaesthetic strategy may contribute to longer ICU treatment courses in OPCABG patients. Anaesthetic goals for OPCABG include safe induction and maintenance of anaesthesia, adequate hemodynamic stability throughout surgery, and early emergence and ambulation supported by postoperative analgesia [7]. The anaesthetic technique discussed by Hemmerling et al. emphasizes maintaining heart rate, mean arterial pressure, and SvO2 within specific ranges, ensuring adequate preload and using vasopressors or inotropes to treat hypotension [8]. Fast extubation can be challenging for OPCABG patients due to hemodynamic instability caused by ischemia prevention and heart position during the operation. Hypotension during surgery may require increased fluid administration and vasoconstrictor agents, potentially leading to volume overload and delayed extubation [9].
While many studies have reported that OPCABG shortens hospital and ICU LOS [10,11,12,13], our findings contradicted this trend. The reasons behind the discrepancy in LOS were not discussed in previous articles. Our study suggests that the success of OPCABG in shortening LOS depends on various factors, including clinicians' preparedness, operator expertise, and the collaboration of supporting clinicians, such as anaesthesiologists and cardiologists, to achieve the desired outcomes. The aforementioned post-CABG problems and the consideration for extubation in OPCABG patients may explain the prolonged ICU LOS observed in our study, despite reports of shorter LOS in other centres. Further data from our centre are needed to provide a clearer understanding of this explanation. However, our study did not provide complete data on the mentioned problems, nor the data on hypotension, volume overload, vasopressor agent use, duration of intubation, and clinician's expertise due to the large amount of data that are not recorded completely. The specific factors influencing LOS in OPCABG require further investigation to improve outcomes and optimize patient care.
Mortality in OPCABG and ONCABG
Factors such as patient tolerance, disease progression, procedural complexity, and postoperative recovery influence mortality rates in CABG surgery [14]. Complications are more common with ONCABG, which may explain its lower death rate than OPCABG [15]. However, our study found no significant difference in mortality between the two techniques.
ONCABG is associated with perioperative complications due to using a CPB machine and manipulating the ascending aorta, including myonecrosis, neurological deficits, renal dysfunction, and systemic inflammation. Strategies to address these issues have been explored, such as measuring brain injury using S100 beta serum concentrations and reducing neurocognitive dysfunction. Lipid material and particle matter have been highlighted as possible causes of postoperative neurocognitive dysfunction in blood collected from the operating field after on-pump CABG [16].
A systemic inflammatory response (SIRS) occurs after on-pump surgery due to surgical trauma, nonphysiological surfaces, ischemia-reperfusion, and hypothermia. Surgical trauma, contact of blood with nonphysiological surfaces (e.g. pump tubing, oxygenator surfaces), myocardial ischemia and reperfusion, and hypothermia all combine to cause a dramatic release of cytokines (e.g. interleukin (IL-6 and IL-8) and other inflammatory mediators after on-pump cardiac surgery. SIRS has been observed in patients undergoing CPB, prompting the development of measures to avoid or reduce its recurrence [17]. Various interventions have been attempted to prevent or reduce SIRS, but their impact on outcomes is unclear [16].
OPCABG, unlike ONCABG, performed on a beating heart with stabilizing devices, aims to minimize complications by avoiding CPB. By avoiding cardiopulmonary bypass, which is linked with microemboli formation, increased blood–brain barrier permeability, and aortic manipulation during cross-clamping and cannulation, OPCABG could theoretically reduce morbidity, notably stroke, and mortality. According to Head et al., the off-pump method was superior to ONCABG in terms of mortality [14]. Another study by Khan et al. [10] mentions that the risk of mortality increases with the ONCABG technique as it increases SIRS incidence, which can cause mortality from septic shock. However, Gaudino et al. report the contrary as they found that OPCABG is associated with a higher incidence of incomplete revascularization, an increased need for repeated revascularization, and decreased midterm survival compared with ONCABG.
On the other hand, our study concludes no significant difference in mortality between OPCABG and ONCABG. A study conducted by Brewer et al. [11] supports our findings as they demonstrate no difference in operative mortality for OPCAB patients compared to ONCAB patients. Hillis et al. [16] mention in the ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery that around the year 2005, an AHA scientific statement comparing the two techniques concluded that regardless of some studies about the comparison of both procedures, both generally resulted in excellent outcomes and that neither method should be considered superior to the other. Because CPB maintains systemic circulation, surgeons often favour ONCABG in patients with hemodynamic impairment. OPCABG, on the other hand, is favoured by some surgeons who have substantial experience with it and are, therefore, familiar with its technical aspects. According to the explanations, ONCABG was better for mortality than OPCABG because of the impacts of the CPB machine, SIRS, and cerebrovascular accidents. However, our study suggests no significant difference in mortality in both techniques in the authors' centre.
The choice between techniques depends on surgeon preference and patient characteristics. Our study has limitations, being retrospective and single-centre. Future research should include prospective studies or randomized controlled trials with long-term survival data to eliminate confounding factors further. Furthermore, our study was a single-centre study; thus, the applicability of the results was worth discussing. Additionally, the lack of data, such as risk stratification and the use of inotropes, has prevented us from allocating the sample into sub-groups. Further research with these data is needed to better understand our findings.
Conclusions
Our study found that ICU LOS was significantly longer in OPCABG patients than in ONCABG patients, and there was no significant difference in mortality between the two groups. The results suggest that clinicians have to pay more attention to some suspected problems as the reasons behind OPCABG's prolonged ICU so that the goal of OPCABG application can be achieved. In addition, some improvements still need to significantly decrease mortality in applying the OPCABG procedure in the authors' centre.
Availability of data and materials
Data are not available for third-party use as the ethics approval does not cover this for this project.
Abbreviations
- CABG:
-
Coronary artery bypass graft
- CAD:
-
Coronary artery disease
- CVD:
-
Cardiovascular disease
- CPB:
-
Cardiopulmonary bypass
- ICU LOS:
-
Intensive care unit length of stay
- ONCABG:
-
On-pump coronary artery bypass graft
- OPCABG:
-
Off-pump coronary artery bypass graft surgery
- SIRS:
-
Systemic inflammatory response
References
Bakaeen F (2017) CABG: a continuing evolution. Cleve Clin J Med 84(12 Suppl 4):e15–e19
Diegeler A, Börgermann J, Kappert U et al (2013) Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med 368(13):1189–1198
Lamy A, Devereaux PJ, Prabhakaran D et al (2016) Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N Engl J Med 375(24):2359–2368
Gaudino M, Benedetto U, Bakaeen F, Rahouma M, Tam DY, Aouarab A et al (2018) Off- versus on-pump coronary surgery and the effect of follow-up length and surgeons’ experience: a meta-analysis. J Am Heart Assoc 7(21):e010034
Shaefi S, Mittel A, Loberman D, Ramakrishna H (2019) Off-pump versus on-pump coronary artery bypass grafting-a systematic review and analysis of clinical outcomes. J Cardiothorac Vasc Anesth 33(1):232–244
Fuster V, Walsh RA, Harrington RA (2011) Hurst’s the heart, 13th edn. McGraw-Hill Education
Trivedi K, Patel A, McMackin K, Highbloom R, Patel K, Desai R (2021) Anesthetic management for conventional myocardial revascularization. In: Awad AS (ed) Cardiac anesthesia. Springer, Cham
Hemmerling TM, Romano G, Terrasini N et al (2013) Anesthesia for off-pump coronary artery bypass surgery. Ann Card Anaesth 16:28–39
Green R, Hutton B, Lorette J, Bleskie D, McIntyre L, Fergusson D (2014) Incidence of postintubation hemodynamic instability associated with emergent intubations performed outside the operating room: a systematic review. CJEM 16(1):69–79
Khan MS, Islam MY, Ahmed MU et al (2014) On pump coronary artery bypass graft surgery versus off pump coronary artery bypass graft surgery: a review. Glob J Health Sci 6(3):186–193
Brewer R, Theurer PF, Cogan CM et al (2014) Morbidity but not mortality is decreased after off-pump coronary artery bypass surgery. Ann Thorac Surg 97:831–837
Sheikhy A, Fallahzadeh A, Sadeghian S et al (2021) Mid-term outcomes of off-pump versus on-pump coronary artery bypass graft surgery; statistical challenges in comparison. BMC Cardiovasc Disord 21:412
Carmona P, Paredes F, Mateo E, Mena-Durán AV, Hornero F, Martínez-León J (2016) Is off-pump technique a safer procedure for coronary revascularization? A propensity score analysis of 20 years of experience. Interact Cardiovasc Thorac Surg 22(5):612–618
Head SJ, Kieser TM, Falk V et al (2013) Coronary artery bypass grafting: Part 1—the evolution over the first 50 years. Eur Heart J 34:2862–2872
Sheikhy A, Fallahzadeh A, Forouzannia K et al (2022) Off-pump versus on-pump coronary artery bypass graft surgery outcomes in patients with severe left ventricle dysfunction: inverse probability weighted study. BMC Cardiovasc Disord 22:488
Hillis LD, Smith PK, Anderson JL et al (2011) 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: a report of the american college of cardiology foundation/american heart association task force on practice guidelines. Circulation 124(25):e957
Akar AR, İnan B, Punjabi KP, Dernek S (2022) Systemic inflammatory response and cardiopulmonary bypass. In: Punjabi PP, Kyriazis PG (eds) Essentials of operative cardiac surgery. Springer, Cham
Acknowledgements
Not applicable.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
RZI contributed substantially in the conception and design of the study, acquisition of data, interpretation of data, and finalization of the article. EOJ contributed substantially in data analysis, interpretation of data, and drafting the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval and waiver of consent were granted by the Ethical Committee Board of National Cardiovascular Center Harapan Kita Hospital and have therefore been performed following the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Consent was waivered because this study only involves the use of secondary data, which involves no risk to the subject.
Consent for publication
Not applicable.
Competing interests
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial or non-financial interest in this manuscript's subject matter or materials.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ibrahim, R.Z., Joyo, E.O. Intensive care unit length of stay and mortality comparison between on-pump and off-pump coronary artery bypass graft: a retrospective study. Egypt Heart J 75, 48 (2023). https://doi.org/10.1186/s43044-023-00374-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-023-00374-1