Abstract
Background
Nocturnal enuresis (NE) is a common voiding problem in pediatric populations. Relatively, few studies have investigated the 25-Hydroxyvitamin D and NE associations in children, which may open up a new research area on the effect of vitamin D as nutritional therapy in the treatment of NE. The aim of this study was to determine the level of 25-hydroxyl vitamin D among children and adolescents with nocturnal enuresis in comparison to non-enuretic Egyptian children.
Results
Fifty children (24 females, 26 males) who presented with primary mono-symptomatic nocturnal enuresis (PMNE) and 50 healthy children (23 females, 27 males) were recruited in this study. A structured questionnaire focusing on demographic, socioeconomic, and frequency of bed-wetting were collected, and vitamin D serum levels were assessed in all children. In the NE group, the mean value of serum vitamin D levels was lower than the control (19.0 ± 6.5 versus 23.89 ± 4.19; P < 0.0001). Serum 25-hydroxyvitamin D levels were abnormal (< 20 ng/mL) in 46% of children with NE and 16% of controls (P < 0.001). The higher bed-wetting frequencies were associated with lower levels of 25(OH) D (Every night: 7.0 ± 1.4, 3–5 time/week: 11.2 ± 1.7, 1–3 times/week: 17.6 ± 3.7, < 2times/week: 22.4 ± 2.9, Once/6 month: 24.1 ± 4.3 (ng/ml), P < 0.001).
Conclusion
A difference in serum 25-hydroxyvitamin D levels was found between the two study groups. There is a need for more studies to explain vitamin D deficiency in larger series so that this test can be used in regular enuretic child investigations.
Similar content being viewed by others
Background
Enuresis is a common pediatric condition that can cause psychological distress in children and their families. Enuresis refers to discrete urinary incontinence episodes in children of 5 years age and older who are asleep [1]. Enuresis, while the pathogenesis and evaluation of the two types overlap, is divided into mono-symptomatic and non-mono-symptomatic forms [2]. Enuresis without any other urological symptoms is known as mono-symptomatic NE. The term non-mono-symptomatic is for all other children who do not meet these criteria [1]. In children aged 5 years and above, the incidence of NE appears to be around 20 percent with a male predominance [3].
The prevalence of NE in Egyptian children was 15.5% in a study conducted in Benha. [4]. Data on recent studies indicate that 16.5% of Children suffered from NE Minia City, Egypt [5].
Nocturnal polyuria, decreased bladder capacity, detrusor over activity, global maturation delay, related sleep arousal disturbances, and genetics are the common underlying pathophysiology of NE. NE, mostly, is a multifactorial disorder caused by a mixture of these etiologies [6].
25-hydroxyvitamin D is a fat‐soluble vitamin with several functions and target organs. The influence of many genes can be affected by vitamin D and its receptor (VDR) following binding. VDR expression is usually in the bone cells, kidney, skin cells, and other cells [7]. Moreover, accumulating epidemiological and laboratory evidence documented that levels of 25-hydroxyvitamin D are closely related to the occurrence of many chronic conditions [8]. Although a little information about the effect of vitamin D deficiency and the risk of bed-wetting is known, an inverse association between 25(OH) D and NE in children was reported in a Chinese study for the first time [9]. They proposed that there is some link between 25-hydroxyvitamin D and NE based on the impact of 25-hydroxy vitamin D on different physiological mechanisms and suboptimal 25-hydroxyvitamin D concentrations may be the leading cause of excessive urine production [9]. As far as we know, no study has been conducted in Egypt in this respect. Thus, this study aimed to determine the level of vitamin D among Egyptian children with NE.
Methods
One hundred children and adolescents in the age group between five and 16 years old from December 2019 to May 2020 were recruited in this study. Of the 100 children under study, 50 children with Primary mono-symptomatic NE were consecutively selected from psychiatry Clinic, Pediatrics Hospital, as the case group in accordance to the Standardization Committee of the International Children’s Continence Society [1], and 50 age and sex matched healthy children without enuresis in the control group. The inclusion criteria is two or more enuretic episodes a week for at least three consecutive months in children aged 5 to 16; while the exclusion criteria included: supplemental vitamin D intake > 400 IU/d, daytime wetting, infection of the urinary tract during the past three months, polyuric diseases, abnormal urine test, abnormality of the urinary tract, history of genitourinary abnormality, associated neurological abnormalities, associated chronic illness and any significant drug intake.
The required sample size was calculated using the Epitools program setting to detect the alpha error at 5% and power at 80%.
Ethical approval was obtained from the Research Ethics Committee at the Faculty of Medicine, (Ethical Committee No. FMASU R86 /2020).
Questionnaires
Using a structured questionnaire, demographic data were collected, and Socioeconomic Standard was assessed using the new version scale of the Arabic validated Socioeconomic Status Scale for research study in Egypt [10].
25-hydroxyvitamin D assessment
The Serum samples of collected blood from all children were separated, centrifuged, and preserved at − 20 °C until the laboratory assessments. We used the Cal biotech Vitamin D Kit, a solid phase enzyme-linked immunoassay (ELISA), to detect serum vitamin D levels. The cut-off value of 25-hydroxyvitamin D deficiency was < 20 ng/ml [11].
Statistical analysis
The collected data were revised, coded, and introduced using IBM SPSS Statistics version 23. Continuous variables were represented by the mean and standard deviation, while categorical variables were represented by percentages. Comparisons between the groups were made using an independent t test for continuous variables and a chi-squared test for categorical variables. The value of serum vitamin D level for discrimination between cases and controls was examined using receiver-operating characteristic (ROC) curve analysis. The Kruskal–Wallis test was used to determine the relationship between bed-wetting frequencies and 25(OH) D levels. P value of less than 0.05 was considered statistically significant.
Results
Of 100 children/adolescents included in the study, the mean age in the NE and control groups was 9.24 ± 2.54 and 9.20 ± 2.51 years, respectively. No significant differences were observed in both study groups in gender, height, weight, and birth order. In addition, no differences were found in the educational levels of the parents, per-capita income, and socioeconomic status between the two groups (Table 1).
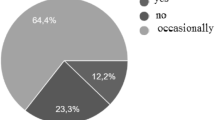
The mean value of serum vitamin D was statistically significantly lower in the NE group compared to controls (19.0 ± 6.5 versus 23.89 ± 4.19; P < 0.0001), 46.0% of the NE group had vitamin D deficiency compared to (16.0%) in controls (P < 0.001; Table 2). Receiver operating characteristics (ROC) curve was used to define the best cut-off value of vitamin D that was ≤ 19 ng/ml, with a sensitivity of 46% %, a specificity of 84%, the positive predictive value of 74.2%, negative predictive value of 60.9%, and area under the curve (AUC) of 0.616, P < 0.046; Fig. 1). The lower 25(OH) D concentrations were associated with higher frequencies of bed-wetting (Every night: 7.0 ± 1.4, 3–5 time/week: 11.2 ± 1.7, 1–3 times/week: 17.6 ± 3.7, < 2times/week: 22.4 ± 2.9, Once/6 month: 24.1 ± 4.3 (ng/ml), (P < 0.001; Table 3, Fig. 2).
Receiver operating characteristics (ROC) curve. Receiver operating characteristics (ROC) curve was used to define the best cut-off value of vitamin D that was ≤ 19 ng/ml, with sensitivity of 46% %, specificity of 84%, positive predictive value of 74.2% and negative predictive value of 60.9%, with an area under the curve (AUC) of 0.616, P < 0.046
The frequency of bed-wetting according to 25(OH) D concentrations. The lower mean 25(OH) D concentrations were associated with higher frequencies of bed wetting (Every night: 7.0 ± 1.4, 3–5 time/week: 11.2 ± 1.7, 1–3 times/week: 17.6, < 2times/week: 22.4 ± 2.9, Once/6 month: 24.1 ± 4.3 (ng/ml), P < 0.001
Discussion
Nocturnal enuresis, better known as bed-wetting, happens when at night, a sleeping child is unable to retain its urine. It is a common childhood problem with little more male predominance. To children, parents, and health care providers, this problem can be stressful. The mean age of the enuretic children was 9.24 ± 2.54 years. Several studies have shown that the NE level decreases as age increases [12]. According to Alhifthy et al. [13] the prevalence of NE was 63% at the age of 6–7 years and 4.5% at the age of 10–12 years old that is consistent with previous reports [5, 14]. In this study, the order of birth was not significantly different between both groups, and this agrees with a Turkish study that reported no association between birth order and the prevalence of NE [15]. However, Kamal et al. reported that birth order had a significant effect on the prevalence of enuresis as it occurs more frequently in the second child than in the first or third child [5]. The present study showed no differences in socioeconomic status between both groups. Similarly, Dolgun et al. [16] found that socioeconomic development did not affect the prevalence of enuresis. However, several studies mentioned that low socioeconomic status is a consistent risk factor for the incidence of wetting problems [3, 5, 17]. Although NE is a common childhood problem, the mechanism of this condition remains unclear. Also, several studies highlighted the impact of deficiency of some vitamins in nocturnal enuresis etiopathogenesis. Enuretic children, for example, have lower levels of serum vitamin B12 and folate than their non-enuretic counterparts [18, 19].
The present study showed that the NE group had a significantly lower mean vitamin D level than controls (19.0 ± 6.5 versus 23.89 ± 4.19). Moreover, 84% of controls had optimal vitamin D status, whereas in NE, 46% had vitamin D deficiency. In the present study, lower 25(OH) D concentrations were associated with higher frequencies of bed-wetting.
To the best of our knowledge, Li et al. reported for the first time in a study conducted on 247 Chinese children that one-third of children who suffering from NE had vitamin D deficiency [9]. They revealed that an increased frequency of bed-wetting was related to low 25(OH) D levels. Furthermore, as the level of 25(OH) D decreases, the severity of NE rises. They outlined their findings by analyzing the effect of low levels of vitamin D on the architecture of sleep which is considered as one of the main mechanisms of NE. Some studies have demonstrated that children who suffered from enuresis have disrupted sleep with several intermittent arousals that result in fragmentation of sleep and poor quality of sleep [20]. Some previous studies have shown an association between sleep disturbance and NE [21], which confirmed with Nevéus’ report stating that the sleep problem is closely related to the pathophysiology of nocturnal enuresis [22]. Children suffered from NE may have a high threshold of cortical arousability, so they will not wake up when the bladder reaches its maximum capacity. Several studies have demonstrated that vitamin D (VDR) receptors are expressed in brain regions that control sleep regulation, such as the hypothalamus [23, 24]. The higher vitamin D status was negatively linked to the risk of sleep disorders in these studies. Suboptimal vitamin D levels have been reported to correlate with poorer quality of sleep [25]. Interestingly, emerging evidence suggests that vitamin D may play an immunomodulatory function by changing immune regulation, reducing inflammatory substances release that control sleep, like tumor necrosis factor alpha, prostaglandin D2, and cytokine [26, 27]. The vitamin D deficiency-related spectrum of disease is likely to include immune dysregulation diseases that may be manifested by excessive sleepiness throughout the day induced by inflammatory cascade components. Thus, it is mechanistically possible that suboptimal vitamin D levels through modulation of immune-regulating substances will contribute to impaired sleep quality [28]. Together, these findings support the theory that vitamin D deficiency through its effect on sleep quality may lead to an increased risk of bed-wetting.
The function of vitamin D in the regulation of water channels was investigated in animal studies of mice kidneys. Polyuria has been shown to develop in VDR-null mice as a result of VDR inactivation leading to an increase in production of Angiotensin II, which plays the central role in the occurrence of polyuria [29, 30] The underlying relationship of Aquaporins (AQP), also known as water channel proteins involved in controlling water transport and Vitamin D/VDR mediated urinary development, was investigated in another animal study on both knockout and wild type mice and found that 1α (OH)ase knockout mouse developed polyuria, suggesting that vitamin D can control the urine production and excretion [31].
Another Iranian study revealed that supplementation with omega-3 and vitamin D may decrease the frequency of bed-wetting among children with NE. While there was still no specific mechanism for their operation to reduce bed-wetting in enuretic children, there was stronger evidence of improvement with vitamin D, researchers said [32].
Limitations
First, the sample size is small, so more prospective studies with larger series are needed to confirm our results. Also, there was no evaluation for sleep quality, habits, and sleep disorders, such as a structured comprehensive questionnaire or polysomnography, a gold standard method for sleep-disordered breathing. To understand the mechanisms of serum VD deficiency in NE patients, more studies should be conducted to focus on the effect of VD supplementation in children with NE and its impact on clinical symptoms, severity, and ameliorate the risk of NE.
Conclusion
There is a significant decrease in 25-Hydroxyvitamin D levels in children and adolescents with primary mono-symptomatic nocturnal enuresis comparing to children without enuresis. This test can be used in regular investigations of enuretic children if vitamin D deficiency is found in larger series. As a result, the effectiveness of vitamin D supplementation may be evaluated in children with low levels.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- NE:
-
Nocturnal enuresis
References
Austin PF, Bauer SB, Bower W, Chase J, Franco I, Hoebeke P et al (2016) (2016) The standardization of terminology of lower urinary tract function in children and adolescents: update report from the standardization Committee of the International Children’s continence society. Neurourol Urodyn 35(4):471–481. https://doi.org/10.1002/nau.22751
Neveus T, Eggert P, Evans J et al (2010) Evaluation of and treatment for monosymptomatic enuresis: a standardization document from the International Children’s Continence Society. J Urol 183:441. https://doi.org/10.1016/j.juro.2009.10.043
Hadinezhad Makrani A, Moosazadeh M, Nasehi M, Abedi G, Afshari M, Farshidi F et al (2015) Prevalence of enuresis and its related factors among children in Iran: a systematic review and meta-analysis. Int J Pediatr 3(61):995–1004. https://doi.org/10.22038/ijp.2015.5142
Mohammed AH, Saleh AG, Al ZI (2014) Frequency of bedwetting among primary school children in Benha city, Egypt. Egypt J Med Hum Genet 15:287–292. https://doi.org/10.1016/j.ejmhg.2014.01.005
Kamal NN, Mahrous MD (2019) The epidemiology and factors associated with nocturnal enuresis among primary school children in Minia City, Egypt. EJCM 37:63–71. https://doi.org/10.21608/ejcm.2019.28133
Neveus T (2017) Pathogenesis of enuresis: towards a new understanding. Int J Urol 24(3):174–182. https://doi.org/10.1111/iju.13310
Khammissa RAG, Fourie J, Motswaledi MH, Ballyram R, Lemmer J, Feller L (2018) The biological activities of vitamin D and its receptor in relation to calcium and bone homeostasis, cancer, immune and cardiovascular systems, skin biology, and oral health. Biomed Res Int 22:9276380. https://doi.org/10.1155/2018/9276380
Ahmed SZ, Jaleel A, Hameed K, Qazi S, Suleman A (2015) Does vitamin D deficiency contribute to the severity of asthma in children and adults? J Ayub Med Coll Abbottabad 27(2):458–463
Li L, Zhou H, Yang X et al (2014) Relationships between 25-hydroxyvitamin D and nocturnal enuresis in five to seven year old children. PLoS ONE 9(6):e99316. https://doi.org/10.1371/journal.pone.0099316
Fahmy SI, Nofal LM, Shehata SF, El Kady HM, Ibrahim HK (2015) Updating indicators for scaling the socioeconomic level of families for health research. J Egypt Public Health Assoc 90(1):1–7. https://doi.org/10.1097/01.EPX.0000461924.05829.93
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930. https://doi.org/10.1210/jc.2011-0385
Huang HM, Wei J, Sharma S, Bao Y, Li F, Song JW, Wu HB et al (2020) Prevalence and risk factors of nocturnal enuresis among children ages 5–12 years in Xi’an, China: a cross-sectional study. BMC Pediatr 20(1):305. https://doi.org/10.1186/s12887-020-02202-w
Alhifthy EH, Habib L, Abu Al-Makarem A, AlGhamdi M, Alsultan D et al (2020) Prevalence of nocturnal enuresis among Saudi children population. Cureus. 2(1):e6662. https://doi.org/10.7759/cureus.6662
Hamed A, Yousf F, Hussein MM (2017) Prevalence of nocturnal enuresis and related risk factors in school-age children in Egypt: an epidemiological study. World J Urol 35(3):459–465. https://doi.org/10.1007/s00345-016-1879-2
Gunes A, Gunes G, Acik Y, Akilli A (2009) The epidemiology and factors associated with nocturnal enuresis among boarding and daytime school children in Southeast of Turkey: a cross sectional study. BMC Public Health. https://doi.org/10.1186/1471-2458-9-357
Dolgun G, Savaser S, Balci S, Yazici S (2012) Prevalence of nocturnal enuresis and related factors in children aged 5–13 in istanbul. Iran J Pediatr 22(2):205
Bilal M, Haseeb A, Saeed A, Saeed A, Sarwar T, Ahmed S, Ishaque A, Raza M (2020) Prevalence of nocturnal enuresis among children dwelling in rural areas of Sindh. Cureus 12(8):e9590. https://doi.org/10.7759/cureus.9590
Albayrak S, Zengin K, Tanik S, Daar G, Ozdamar MY et al (2014) Vitamin B12, folate and iron levels in primary nocturnal enuresis. Pak J Med Sci 31:87–90. https://doi.org/10.12669/pjms.311.6424
Altunoluk B, Davutoglu M, Garipardic M, Bakan V (2012) Decreased vitamin B12 levels in children with nocturnal enuresis. ISRN Urol. https://doi.org/10.5402/2012/789706
Dhondt K, Baert E, Van Herzeele C, Raes A, Groen LA, Hoebeke P et al (2014) Sleep fragmentation and increased periodic limb movements are more common in children with nocturnal enuresis. Acta Paediatr 103(6):e268e72. https://doi.org/10.1111/apa.12610
Gu Y-M, Kwon JE, Lee G, Lee SJ, Suh HR, Min S, Cho MH (2016) Sleep problems and daytime sleepiness in children with nocturnal enuresis. Childhood Kidney Dis 20(2):50–56. https://doi.org/10.3339/jkspn.2016.20.2.50
Neveus T (2008) Enuretic sleep: deep, disturbed or just wet? Pediatr Nephrol 23:1201–1202. https://doi.org/10.1007/s00467-008-0859-1
Eyles DW, Liu PY, Josh P, Cui X (2014) Intracellular distribution of the vitamin d receptor in the brain: comparison with classic target tissues and redistribution with development. Neuroscience 268:1. https://doi.org/10.1016/j.neuroscience.2014.02.042
Stumpf WE, O’Brien LP (1987) 1, 25(OH) 2 vitamin D 3 sites of action in the brain. Histochemistry 87:393–406. https://doi.org/10.1007/bf00496810
Massa J, Stone KL, Wei EK, Harrison SL, Barrett-Connor E et al (2015) Vitamin D and actigraphic sleep outcomes in older community-dwelling men: the MROS sleep study. Sleep 38:251–257. https://doi.org/10.5665/sleep.4408
Jablonski KL, Chonchol M, Pierce GL, Walker AE, Seals DR (2011) 25-hydroxyvitamin d deficiency is associated with inflammation-linked vascular endothelial dysfunction in middle-aged and older adults. Hypertension 57:63. https://doi.org/10.1161/HYPERTENSIONAHA.110.160929
Martens PJ, Gysemans C, Verstuyf A, Mathieu AC (2020) Vitamin D’s effect on immune function. Nutrients 12(5):1248. https://doi.org/10.3390/nu12051248
McCarty DE, Reddy A, Keigley Q, Kim PY, Marino AA (2012) Vitamin D, race, and excessive daytime sleepiness. J Clin Sleep Med 8:693–697. https://doi.org/10.5664/jcsm.2266
Li YC, Kong J, Wei M, Chen ZF, Liu SQ, Cao LP (2002) 1,25-Dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest 110:229–238. https://doi.org/10.1172/JCI15219
Kong J, Li YC (2003) Effect of angiotensin II type I receptor antagonist and angiotensin-converting enzyme inhibitor on vitamin D receptor null mice. Am J Physiol Regul Integr Comp Physiol 285(1):R255–R261. https://doi.org/10.1152/ajpregu.00517.2002
Fu Y, Zhu J, Zhang Y, Liu Z, Su H, Kong J (2019) Vitamin D regulates the expressions of AQP-1 and AQP-4 in mice kidneys. Biomed Res Int 27:3027036. https://doi.org/10.1155/2019/3027036
Rahmani E, Eftekhari MH, Fallahzadeh MH, Fararouei M, Massoumi SJ (2018) Effect of vitamin D and omega-3 on nocturnal enuresis of 7–15-year-old children. J Pediatr Urol 14(3):257–257. https://doi.org/10.1016/j.jpurol.2018.01.007
Acknowledgements
We thank the staff of Pediatric psychiatry Clinic in Ain-Shams University hospitals for their collaboration in sampling as well as the children who participated in the study.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
FM, RI, MG and AS contributed to the study conception and design. RI, MG and AS contributed to material preparation, data collection and analysis. RI wrote the first draft of the manuscript and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Participation in the study was voluntary, and written consent was obtained from the parents of all the children participating in the study and the approval from the Ain Shams University Ethics committee was obtained FMASU R86 /2020.
Consent for publication
Not applicable.
Competing interest
No competing interest is declared by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Baz, F.M., Abdelsayed, M.G.R., Abdel-Hafeez, A.S. et al. Decreased vitamin D levels in children with primary mono-symptomatic nocturnal enuresis. Egypt J Med Hum Genet 22, 71 (2021). https://doi.org/10.1186/s43042-021-00191-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-021-00191-8