Abstract
Background
An idiopathic outflow tract premature ventricular complex (OT-PVC) is a common arrhythmia, and the accuracy of site of origin prediction using the 12-lead electrocardiogram (ECG) algorithm is not high. There are no studies about a systematic strategy that can provide practical help to electrophysiologists in OT-PVC mapping and ablation. This study aims to evaluate the efficacy and safety of the proposed ablation protocol and establish an optimal catheter ablation strategy by simultaneously investigating and synthesizing various indicators observed during the mapping procedure.
Methods and design
This study (ABOUT-PVC) was designed as a prospective multicenter study to enroll 210 patients from 11 tertiary university hospitals over an estimated 27 months. Patients with idiopathic OT-PVC requiring catheter ablation will receive the procedure through a proposed ablation strategy and will be followed up for at least 12 months. The primary outcome is the acute procedural success rate. The secondary outcomes are clinical success rate, procedure time, complication rate, symptom relief, and changes in echocardiographic parameters.
Conclusions
The ABOUT-PVC study was designed to investigate the efficacy and safety of the proposed ablation strategy and establish an optimal catheter ablation strategy. We expect this study to overcome the limitations of the ECG prediction algorithms and provide a practical guide to electrophysiologists, increasing the procedure’s success rate and reducing complications and procedure time.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Premature ventricular complexes (PVCs) are common arrhythmias in clinical practice and mainly originate from the outflow tract (OT) of both ventricles [1,2,3]. In outflow tract premature ventricular complexes (OT-PVC), catheter ablation has been established as a curative treatment option by demonstrating efficacy and safety in randomized controlled trials and observational studies [4,5,6,7,8,9]. An OT-PVC is a focal arrhythmia caused by triggered activity, and finding the site of origin (SOO) using activation mapping is pivotal to successful ablation [10]. The most important part prior to mapping is to determine whether the SOO is the right ventricular outflow tract (RVOT) or the left ventricular outflow tract (LVOT) using a 12-lead electrocardiogram (ECG). The precordial transition is widely accepted because it is simple and intuitive. If the R-/S-wave transition is ≥ V4, the SOO is likely to be the RVOT, whereas if it is V1-2, the origin is likely the LVOT [11]. However, there are several limitations to 12-lead ECG-based prediction algorithms. First, the position and degree of rotation of the heart vary from person to person [12, 13]. It has also been reported that subtle misplacement of ECG electrodes could markedly alter precordial transition, leading to an erroneous ablation procedure [14]. In addition, because the OT is a complex anatomic structure in which myocardial fibers are intertwined with each other, cases of LVOT origin with preferential conduction to the RVOT have also been reported [15]. Due to these limitations of ECG prediction algorithms, the mapping and ablation process may fail, which can confuse the operators and reduce the ablation success rate. Therefore, we propose a simple and practical ablation strategy to guide the electrophysiologist during the entire procedure while avoiding the limitations of the ECG prediction algorithms.
Because OT-PVC is a focal mechanism, finding the earliest activation site using mapping determines the procedure’s success [10]. According to two review articles, the earliest local activation time (from local electrogram to QRS onset) of the site of origin is approximately 20 ms or more [16, 17]. However, no prospective studies found the optimal cutoff value of the earliest local activation time (EAT) that could predict acute and clinical success. We previously reported the optimal cutoff value of the EAT at earlier than 30 ms to predict successful ablation in a single-center retrospective study involving 193 patients [18]. Through this prospective multicenter study, we tried to establish a practical OT-PVC ablation strategy while validating the cutoff value of the EAT suggested in the previous study.
Methods
Study design and population
This study (ABOUT-PVC) was designed as a prospective multicenter study to enroll 210 patients from 11 tertiary university hospitals over an estimated 27 months. All consecutive patients visiting each institution who meet the inclusion/exclusion criteria and agree to participate in this study will be enrolled. From October 2020 to December 2023, a total of 210 patients were finally enrolled. The trial will enroll OT-PVC patients who (1) are older than 18 years and (2) satisfy the following indications for catheter ablation: (a) symptomatic frequent PVCs with a burden of 15% or more on the 24-h Holter monitor despite continuing antiarrhythmic drugs for two months or (b) PVC-mediated cardiomyopathy, frequent PVCs causing left ventricular systolic dysfunction (left ventricular ejection fraction < 50%). Patients will be excluded if they have (1) valvular heart disease (more than a moderate amount of valve stenosis or regurgitation), (2) suspected or definitive cardiomyopathy, (3) prior cardiac surgery, (4) prior catheter ablation for any reason, or (5) congenital heart disease. As the institution in charge, the Samsung Medical Center Institutional Review Board first approved the research protocol on October 15, 2020 (IRB File No. 2020–09-090–002). The other participating centers' local institutional review boards have approved the study protocol. Written informed consent will be obtained from all patients. The study complies with the ethical guidelines of the 1975 Declaration of Helsinki.
Definitions and outcomes
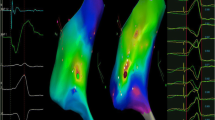
Idiopathic OT-PVC is defined as PVC with an inferior axis occurring in the absence of structural heart disease and identified by echocardiography and/or other imaging studies. Among patients with a PVC burden greater than 15% and LVEF less than 50%, patients without evidence of other cardiomyopathies on cardiac computed tomography (CT) and/or cardiac magnetic resonance imaging (MRI) were defined as possible PVC-induced cardiomyopathy. PVC-induced cardiomyopathy was confirmed by LVEF restoration (LVEF ≥ 50%) after successful clinical PVC ablation. The EAT is measured from initial deflection on distal bipolar electrogram (EGM) to the earliest onset of PVC-QRS on the 12-lead surface ECG. The characteristic shapes of bipolar (fractionated vs. non-fractionated potential) and unipolar (QS vs. rS) potentials are also investigated. Detailed measurements of the various electrocardiographic and electrophysiologic parameters are depicted in Fig. 1. Acute procedural success will be defined as complete absence of clinical PVC during a waiting period longer than 30 min after ablation with a programmed electrophysiologic stimulation. Clinical success is defined as complete elimination of clinical PVC or a PVC burden reduction ≥ 80% in 24-h Holter monitoring performed within 6–12 months after the index procedure. The primary outcome is acute procedural success rate, and the secondary outcomes are clinical success rate, procedure time, complication rate, symptom relief, and changes in echocardiographic parameters.
Specific measurements of echocardiographic and electrophysiologic parameters. The distal and proximal bipolar electrograms (EGM) are presented as MAP-d and MAP-p, respectively. The Uni-d refers to the distal unipolar EGM. PVC premature ventricular complex; QRSd QRS duration; RWd R-wave duration; RWa R-wave amplitude; SWd S-wave duration; SWa S-wave amplitude; EAT earliest local activation time; MDI maximum deflection index; EGM electrogram
Electrophysiologic study and OT-PVC ablation strategy
Before the procedure, all patients will discontinue antiarrhythmic drugs for at least five half-lives. A 12-lead surface ECG and intracardiac EGM will be displayed and recorded by an electrophysiology data acquisition system. A three-dimensional electroanatomic mapping (EAM) system will be guided by the CARTO3® navigation system (Biosense Webster, Diamond Bar, CA, USA) with a 3.5-mm irrigated tip catheter (ThermoCool® or ThermoCool® SmartTouch®, Biosense Webster). Before EAM, endocardial shells of both ventricles, especially the outflow tract, will be delineated by intracardiac echocardiography.
In a retrospective study involving 193 OT-PVC patients undergoing catheter ablation, we suggested the optimal cutoff value of EAT, which may predict successful ablation in the RVOT and LVOT.18 Importantly, 20% of patients with precordial transition in lead V2 had a successful ablation at the RVOT, and about 5% with precordial transition ≥ lead V4 had a successful ablation at the LVOT. Based on the above study, the following ablation strategy is devised (Fig. 2), and all patients enrolled in ABOUT-PVC will be mapped and ablated according to this protocol. With the exception of PVC with right bundle branch block (RBBB) morphology (R-/S-wave ratio > 1 in V1), mapping was first started in the RVOT. If different EAT criteria are satisfied at each position (EAT ≥ 30 ms in the RVOT and EAT ≥ 26 ms in the LVOT), ablation will be performed without mapping on the opposite side. If the EAT criteria are not all satisfied in both the RVOT and LVOT, ablation will be performed according to the operator’s discretion.
Radiofrequency (RF) applications will be delivered initially at the earliest site of endocardial activation with a maximal power of 25–35 Watt (W) using an RF generator (Stockert, Biosense Webster). RF output will be upward titrated independently from 25 to 35 W according to impedance and an upper temperature limit of 50 °C. If clinical PVCs are suppressed within 20–30 s (sec), RF application will be maintained for 60–90 s. If the appearance of PVC during the procedure is insufficient to perform precise activation mapping, the procedure will be postponed. Since the ABOUT-PVC study is designed to evaluate the efficacy of the proposed mapping and ablation protocol, specific techniques and power settings are determined at the operator's discretion. Additionally, about 10% of outflow tract PVC may originate from unusual locations (such as intramural or LV summit) inaccessible by a conventional endocardial approach [19]. If EAT is not satisfied or ablation fails with the conventional endocardial approach, mapping the greater cardiac vein and its tributaries or epicardial approach is conducted at the operator's discretion [20]. In these cases, alcohol ablation or bipolar ablation was performed as needed [19].
All eleven tertiary medical centers only used the Carto3 navigation system for this study. For the bipolar electrogram, setting the high-pass filter at 25–30 Hz and a low-pass filter at 300–500 Hz was allowed. For the unipolar electrogram, setting the high-pass filter at 0.1–1 Hz and a low-pass filter at 500 Hz was accepted. A notch filter is generally not turned on but is sometimes turned on if needed.
Data collection and follow-up
Detailed information about variables to be collected in the study is presented in Table 1. The following 12-lead ECG-based algorithms will be analyzed to evaluate the accuracy of predicting the SOO: R-wave duration index, R-/S-wave amplitude index, R-wave deflection interval combined with R-wave amplitude index, V2S/V2R index, and V2 transition ratio. Two experienced electrophysiologists, unaware of the clinical endpoint, will measure all ECG parameters using a digital caliper with magnification.
Follow-up will be scheduled at the outpatient clinic at 1, 3, 6, and 12 months after the index ablation procedure. At each outpatient visit, a symptom check, 12-lead ECG, and 24-h Holter will be performed. Patients with LV systolic dysfunction before the procedure will undergo follow-up echocardiography within six months of the procedure. Antiarrhythmic drugs, including beta-blockers and calcium channel blockers, will be routinely discontinued after the procedure.
Sample size calculation and statistical analysis
Acute procedural success is estimated to be 86%, and a superiority margin of 5% is considered meaningful for the outcome [6, 9, 18]. For a power of 0.90 and an α error of 0.05 to detect superiority margin, 204 patients are needed after accounting for a 7% dropout rate. Sample size was calculated by PASS 15.0 (NCSS, LLC, Kaysville, UT, USA).
Quantitative variables will be expressed as mean ± standard deviation or median (interquartile range [IQR]) according to the normality test. Qualitative variables will be presented as numbers with percentages. To compare the means of two variables, the Student’s t-test and Mann–Whitney test will be performed for continuous variables and Pearson’s Chi-square and Fisher’s exact test for categorical variables. Receiving operating characteristic (ROC) analysis will be used to evaluate the optimal cutoff value of EAT for predicting acute and clinical success. Two ROC curves will be compared using DeLong’s test. Statistical significance is defined as a two-tailed P < 0.05. All statistical analyses will be performed using SPSS statistical software version 26.0 (IBM, Armonk, NY, USA).
Discussion
As catheter ablation is a safe and effective treatment option for idiopathic OT-PVC, recent guidelines recommend that catheter ablation be considered first in patients with frequent symptomatic PVC and suspected PVC-induced cardiomyopathy [21]. Predicting the location of PVC through standard 12-lead ECG is essential for effective catheter ablation. In particular, estimating whether the SOO is located in the RVOT or the LVOT is most important because the vascular approach might differ, and the procedure time could be reduced [11]. In patients without structural heart disease, the electrical activity of the ventricles by PVC is conducted through the normal myocardium, resulting in a characteristic ECG shape depending on the location of the SOO [12]. Various prediction algorithms based on 12-lead ECG have been introduced. Because the LVOT is located posteriorly to the RVOT, algorithms relying on the assumption that the R-wave in V1-2 (precordial transition, R-/S-wave duration index, and R-/S-wave amplitude ratio) will be larger and longer than the S-wave have been reported [22,23,24]. A transition zone index to overcome cardiac rotation has been suggested [25]. However, in the R/S transition in V3, the accuracy of various prediction algorithms using 12-lead ECG is particularly disappointing [13]. Thus, subsequent studies (V2 transition ratio and V2S/V3R index) should focus on the PVC with V3 transition [26, 27]. In a retrospective study, we evaluated the accuracy of five ECG prediction algorithms (R-wave duration index, R-/S-wave amplitude index, R-wave deflection interval combined with R-wave amplitude index, V2S/V2R index, and V2 transition ratio) in 40 patients with V3 transition OT-PVC.18 All five algorithms had an accuracy less than 80%, which did not meet expectations. Yosida et al. suggested clear evidence for the limitation of the ECG prediction algorithm [15]. They reported that PVCs originating from the LVOT often show preferential conduction to RVOT, and 20% of PVCs originating from the LVOT were late transition after V3. In summary, using ECG algorithms to predict the SOO is not sufficiently accurate and should not solely be relied upon.
Incorrect prediction can result in catheter ablation being performed in the wrong place and may increase the procedure time and complication rate, ultimately reducing the success of the procedure. Therefore, we thought that more effective catheter ablation could be achieved if there is a milestone that can help determine the next step during the mapping procedure, apart from the prediction algorithm using 12-lead ECG. Since more than two-thirds of OT-PVC cases originate from the RVOT[1], the biggest concern is how fast the EAT in the RVOT can be considered the SOO. Two review articles on OT-PVC ablation indicated that a successful ablation site is where a sharp bipolar signal is observed 20–30 ms ahead of the QRS complex [16, 17]. However, that opinion is based on experience rather than concrete evidence. There are several studies dealing with EAT of successful ablation sites in OT-PVC. Guodong et al. [28] showed that the EAT at successful ablation sites was significantly earlier compared to unsuccessful sites (− 40 ± 10 ms vs. − 28 ± 11 ms; p < 0.01). The proposed 30 ms is the optimal cutoff value for EAT to predict successful sites [28]. However, Yamada et al. suggested that there was no significant difference in EAT between the initial success group and the failure group [29]. We have reported a single-center retrospective study in which clinical success was achieved in 99% of patients when the EAT was earlier than 30 ms in RVOT PVC [18]. In LVOT PVC, clinical success was achieved in 97% of patients when the EAT was earlier than 26 ms. Based on the result of that study, the OT-PVC ablation strategy described in Fig. 1 will use a stepwise approach using EAT as a milestone for decision making. The purpose of this study is to evaluate the efficacy and safety of the proposed ablation protocol and to establish an optimal catheter ablation strategy by simultaneously investigating and synthesizing various indicators observed during the mapping procedure. Establishing an effective ablation strategy for OT-PVC is expected to increase clinical success, shorten the procedure time, and reduce complications.
Meanwhile, about 10% of idiopathic OT-PVC may originated from the intramural foci [19]. PVC originating from intramural foci requires unique mapping and ablation techniques because the conventional endocardial approach is inaccessible. The ABOUT-PVC study was designed with PVC originating from a common location where the conventional endocardial approach is accessible. Therefore, in challenging situations (intramural or LV summit PVC), mapping the greater cardiac vein and its tributaries or epicardium was performed at the operator’s discretion [20]. After non-conventional mapping, unique ablation techniques such as alcohol or bipolar ablation were also allowed [19].
In conclusion, the ABOUT-PVC study was designed to demonstrate the efficacy of the proposed ablation strategy and establish an optimal catheter ablation strategy by simultaneously investigating various indicators observed during OT-PVC RFCA. We expect this study to overcome the limitations of the 12-lead ECG algorithms and provide a practical guide to the operator, increasing the procedure’s success rate and reducing complications and procedure time.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Maury P, Rollin A, Mondoly P, Duparc A. Management of outflow tract ventricular arrhythmias. Curr Opin Cardiol. 2015;30:50–7. https://doi.org/10.1097/HCO.0000000000000122.
Ouyang F, Mathew S, Wu S, Kamioka M, Metzner A, Xue Y, et al. Ventricular arrhythmias arising from the left ventricular outflow tract below the aortic sinus cusps: mapping and catheter ablation via transseptal approach and electrocardiographic characteristics. Circ Arrhythm Electrophysiol. 2014;7:445–55. https://doi.org/10.1161/CIRCEP.114.001690.
Sirichand S, Killu AM, Padmanabhan D, Hodge DO, Chamberlain AM, Brady PA, et al. Incidence of idiopathic ventricular arrhythmias: a population-based study. Circ Arrhythm Electrophysiol. 2017. https://doi.org/10.1161/CIRCEP.116.004662.
Bogun F, Crawford T, Reich S, Koelling TM, Armstrong W, Good E, et al. Radiofrequency ablation of frequent, idiopathic premature ventricular complexes: comparison with a control group without intervention. Heart Rhythm. 2007;4:863–7. https://doi.org/10.1016/j.hrthm.2007.03.003.
Liao Z, Zhan X, Wu S, Xue Y, Fang X, Liao H, et al. Idiopathic ventricular arrhythmias originating from the pulmonary sinus cusp: prevalence, electrocardiographic/electrophysiological characteristics, and catheter ablation. J Am Coll Cardiol. 2015;66:2633–44. https://doi.org/10.1016/j.jacc.2015.09.094.
Latchamsetty R, Yokokawa M, Morady F, Kim HM, Mathew S, Tilz R, et al. Multicenter outcomes for catheter ablation of idiopathic premature ventricular complexes. JACC Clin Electrophysiol. 2015;1:116–23. https://doi.org/10.1016/j.jacep.2015.04.005.
Lamba J, Redfearn DP, Michael KA, Simpson CS, Abdollah H, Baranchuk A. Radiofrequency catheter ablation for the treatment of idiopathic premature ventricular contractions originating from the right ventricular outflow tract: a systematic review and meta-analysis. Pacing Clin Electrophysiol. 2014;37:73–8. https://doi.org/10.1111/pace.12243.
Ling Z, Liu Z, Su L, Zipunnikov V, Wu J, Du H, et al. Radiofrequency ablation versus antiarrhythmic medication for treatment of ventricular premature beats from the right ventricular outflow tract: prospective randomized study. Circ Arrhythm Electrophysiol. 2014;7:237–43. https://doi.org/10.1161/CIRCEP.113.000805.
Hayashi T, Liang JJ, Shirai Y, Kuo L, Muser D, Kubala M, et al. Trends in successful ablation sites and outcomes of ablation for idiopathic outflow tract ventricular arrhythmias. JACC Clin Electrophysiol. 2020;6:221–30. https://doi.org/10.1016/j.jacep.2019.10.004.
Lerman BB. Mechanism, diagnosis, and treatment of outflow tract tachycardia. Nat Rev Cardiol. 2015;12:597–608. https://doi.org/10.1038/nrcardio.2015.121.
Anderson RD, Kumar S, Parameswaran R, Wong G, Voskoboinik A, Sugumar H, et al. Differentiating right- and left-sided outflow tract ventricular arrhythmias: classical ECG signatures and prediction algorithms. Circ Arrhythm Electrophysiol. 2019;12:e007392. https://doi.org/10.1161/CIRCEP.119.007392.
Yamada T. Idiopathic ventricular arrhythmias: Relevance to the anatomy, diagnosis and treatment. J Cardiol. 2016;68:463–71. https://doi.org/10.1016/j.jjcc.2016.06.001.
Yamada T. Twelve-lead electrocardiographic localization of idiopathic premature ventricular contraction origins. J Cardiovasc Electrophysiol. 2019;30:2603–17. https://doi.org/10.1111/jce.14152.
Anter E, Frankel DS, Marchlinski FE, Dixit S. Effect of electrocardiographic lead placement on localization of outflow tract tachycardias. Heart Rhythm. 2012;9:697–703. https://doi.org/10.1016/j.hrthm.2011.12.007.
Yamada T, Murakami Y, Yoshida N, Okada T, Shimizu T, Toyama J, et al. Preferential conduction across the ventricular outflow septum in ventricular arrhythmias originating from the aortic sinus cusp. J Am Coll Cardiol. 2007;50:884–91. https://doi.org/10.1016/j.jacc.2007.05.021.
Liang JJ, Shirai Y, Lin A, Dixit S. Idiopathic outflow tract ventricular arrhythmia ablation: pearls and pitfalls. Arrhythm Electrophysiol Rev. 2019;8:116–21. https://doi.org/10.15420/aer.2019.6.2.
Hutchinson MD, Garcia FC. An organized approach to the localization, mapping, and ablation of outflow tract ventricular arrhythmias. J Cardiovasc Electrophysiol. 2013;24:1189–97. https://doi.org/10.1111/jce.12237.
Choi J-H, Kwon H-J, Kim HR, Park S-J, Kim JS, On YK, et al. Earliest activation time is a good predictor of successful ablation of idiopathic outflow tract ventricular arrhythmias. Clin Cardiol. 2021;44:573–9. https://doi.org/10.1002/clc.23578.
Neira V, Santangeli P, Futyma P, Sapp J, Valderrabano M, Garcia F, et al. Ablation strategies for intramural ventricular arrhythmias. Heart Rhythm. 2020;17:1176–84. https://doi.org/10.1016/j.hrthm.2020.02.010.
Hanson M, Futyma P, Bode W, Liang JJ, Tapia C, Adams C, et al. Catheter ablation of intramural outflow tract premature ventricular complexes: a multicentre study. EP Europace. 2023;25:100. https://doi.org/10.1093/europace/euad100.
Cronin EM, Bogun FM, Maury P, Peichl P, Chen M, Namboodiri N, et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Europace. 2019;21:1143–4. https://doi.org/10.1093/europace/euz132.
Ito S, Tada H, Naito S, Kurosaki K, Ueda M, Hoshizaki H, et al. Development and validation of an ECG algorithm for identifying the optimal ablation site for idiopathic ventricular outflow tract tachycardia. J Cardiovasc Electrophysiol. 2003;14:1280–6. https://doi.org/10.1046/j.1540-8167.2003.03211.x.
Zhang F, Chen M, Yang B, Ju W, Chen H, Yu J, et al. Electrocardiographic algorithm to identify the optimal target ablation site for idiopathic right ventricular outflow tract ventricular premature contraction. Europace. 2009;11:1214–20. https://doi.org/10.1093/europace/eup231.
Ouyang F, Fotuhi P, Ho SY, Hebe J, Volkmer M, Goya M, et al. Repetitive monomorphic ventricular tachycardia originating from the aortic sinus cusp. J Am Coll Cardiol. 2002;39:500–8. https://doi.org/10.1016/s0735-1097(01)01767-3.
Yoshida N, Inden Y, Uchikawa T, Kamiya H, Kitamura K, Shimano M, et al. Novel transitional zone index allows more accurate differentiation between idiopathic right ventricular outflow tract and aortic sinus cusp ventricular arrhythmias. Heart Rhythm. 2011;8:349–56. https://doi.org/10.1016/j.hrthm.2010.11.023.
Betensky BP, Park RE, Marchlinski FE, Hutchinson MD, Garcia FC, Dixit S, et al. The V(2) transition ratio: a new electrocardiographic criterion for distinguishing left from right ventricular outflow tract tachycardia origin. J Am Coll Cardiol. 2011;57:2255–62. https://doi.org/10.1016/j.jacc.2011.01.035.
Yoshida N, Yamada T, McElderry HT, Inden Y, Shimano M, Murohara T, et al. A novel electrocardiographic criterion for differentiating a left from right ventricular outflow tract tachycardia origin: the V2S/V3R index. J Cardiovasc Electrophysiol. 2014;25:747–53. https://doi.org/10.1111/jce.12392.
Niu G, Feng T, Jiang C, Suo N, Lin J, Qu F, et al. Predictive value of unipolar and bipolar electrograms in idiopathic outflow tract ventricular arrhythmia mapping and ablation. J Cardiovasc Electrophysiol. 2018;29:900–7. https://doi.org/10.1111/jce.13491.
Yamada S, Chung FP, Lin YJ, Chang SL, Lo LW, Hu YF, et al. Electrocardiographic features of failed and recurrent right ventricular outflow tract catheter ablation of idiopathic ventricular arrhythmias. J Cardiovasc Electrophysiol. 2018;29:127–37. https://doi.org/10.1111/jce.13359.
Acknowledgements
None reported.
Funding
This study is supported by a grant of the Korean Heart Rhythm Society.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the papers as follows: Kyoung-Min Park and Ji-Hoon Choi conceived and designed the study; Ji-Hoon Choi, Kyoung-Min Park, Chang Hee Kwon, Sung-Hwan Kim, Yoo Ri Kim, Jin-Bae Kime, Ki-Byung Nam, Jaemin Shim, Jae-Sun Uhm, Hee Tae Yui, Ki Hong Lee, Eue-Keun Choi, and Seongwook Han collected the data; Ji-Hoon Choi and Kyoung-Min Park analyzed and interpreted the result; and Ji-Hoon Choi, Kyoung-Min Park, and Ki-Byung Nam prepared the draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Samsung Medical Center Institutional Review Board first approved the research protocol on October 15, 2020 (IRB File No. 2020-09-090-002). The other participating centers' local institutional review boards have approved the study protocol. The study complies with the ethical guidelines of the 1975 Declaration of Helsinki.
Consent for publication
Written informed consent will be obtained from all patients.
Competing interests
None reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choi, JH., Park, KM., Kwon, C.H. et al. Ablation strategy for idiopathic outflow tract premature ventricular complexes: rationale and design of the ABOUT-PVC study, a prospective multicenter study. Int J Arrhythm 25, 16 (2024). https://doi.org/10.1186/s42444-024-00123-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42444-024-00123-8





