Abstract
Background
People in China and the countries in the Association of Southeast Asian Nations (ASEAN) are affected by neglected tropical diseases and malaria (NTDM). In this study, we aimed to assess the current status and trends of NTDM burden from 1990 to 2019 in China and ASEAN countries, and also explore the association of NTDM burden with socio-demographic index (SDI).
Methods
The data from the Global Burden of Diseases Study 2019 (GBD 2019) results were used. Absolute incidence and death number, and age-standardized incidence and mortality rate (ASIR and ASMR) of NTDM in China and ASEAN were extracted. The estimated annual percentage change (EAPC) and join-point regression in the rates quantified the trends. Nonlinear regression (second order polynomial) was used to explore the association between SDI and ASRs.
Results
The ASIR of NTDM increased in China, Philippines, Singapore and Brunei, at a speed of an average 4.15% (95% CI 3.83–4.47%), 2.15% (1.68–2.63%), 1.03% (0.63–1.43%), and 0.88% (0.60–1.17%) per year. Uptrends of ASIR of NTDM in recent years were found in China (2014–2017, APC = 10.4%), Laos (2005–2013, APC = 3.9%), Malaysia (2010–2015, APC = 4.3%), Philippines (2015–2019, APC = 4.2%), Thailand (2015–2019, APC = 2.4%), and Vietnam (2014–2017, APC = 3.2%, all P < 0.05). Children < 5 had relatively low incidences but unexpectedly high mortality rates of NTDM in most ASEAN countries. Both incidence and mortality rates of NTDM were higher in older people. ASIR and ASMR of NTDM had a U-shaped association with SDI.
Conclusions
The burden of NTDM in China and ASEAN countries was still huge and affects vulnerable and impoverished populations’ livelihoods, including children under the age of 5 and people aged 60 and older. Facing with the large burden and complex situation of NTDM in China and ASEAN countries, regional cooperating strategies are needed to reduce the burden of NTDM, so as to achieve the goal of elimination in the world.
Similar content being viewed by others
Introduction
The countries in the Association of Southeast Asian Nations (ASEAN), including Brunei, Cambodia, Indonesia, Laos, Malaysia, Myanmar, Philippines, Singapore, Thailand, and Vietnam, are economically and socially integrated. The coronavirus disease 2019 (COVID-19) pandemic has brought the need for regional collaboration on prevention and control of infectious diseases to the fore, and ASEAN countries have resolved to address cross-country management of infectious diseases in late 2020 [1]. However, with different types of political intuitions, different religions, various levels of economic development, and, the most important, different types of health systems, there remains challenges for ASEAN countries to achieve regional coordination for the prevention and control of infectious diseases [2]. China-ASEAN dialogue relations have been established over 30 years [3]. As the two largest economies in the Asia Pacific region, China and ASEAN could be well positioned to exert a significant influence on Asian and even global health.
Neglected tropical diseases mostly affect people living in extreme poverty, and almost 30% of the population in ASEAN countries were living in extreme poverty [4]. Previous study had shown great burden of neglected tropical diseases and malaria (NTDM), in China and certain ASEAN countries. An alarming 5.2 million dengue cases were reported in 2019, and Asia contributes 70% of the global dengue burden [5]. Additionally, dengue represents a major economic threat, according to previous study estimating that almost US$1 billion in annual economic losses for ASEAN countries [6]. The age-standardized incidence rate of malaria in Southeast Asia was 134.47 per 100,000 in 2019, higher than most other regions outside of the African regions [7]. As reported by World Malaria Report 2022, South-East Asia Region had nine malaria endemic countries in 2021, accounting for 5.4 million cases and contributing 2% of the burden of malaria cases globally. [8] Rabies, with high case fatality rate, also represents an important public health threat in ASEAN countries. Although rabies has been declared free in Singapore and Malaysia, rabies outbreaks occurred at few states in recent years [9, 10]. Meanwhile, the remainder of ASEAN countries and China, especially the poorest areas of countries such as Indonesia or the Philippines, continue to report rabies cases. [11] It was also shown that Southeast Asia and several other tropical regions were experiencing increasing trends in the incidence of neglected tropical diseases [12].
The Sustainable Development Goals (SDGs) aimed to end the epidemics of NTDM by 2030. [13] Despite the decrease in mortality and morbidity from major infectious diseases, the world is not on track to meet the 2020 milestones of SGDs of certain infectious diseases, such as malaria and Dengue [14,15,16]. To achieve the goals of SDGs, huge efforts need to be taken by countries all over the world, especially for China and ASEAN countries, the two largest economies in the Asia Pacific region. However, a comprehensive description of NTDM in China and ASEAN and their position compared with the global level is lacking and emergingly needed.
Therefore, in this study, we aimed to assess the current status and trends of NTDM burden from 1990 to 2019 in China and ASEAN countries, using the data from Global Burden of Disease Study 2019 (GBD 2019) results, which consisted of a systematic and scientific effort to quantify the comparative magnitude of health losses due to diseases by sex, age, and location over time [17]. Moreover, we also aimed to explore the association of NTDM burden in China and ASEAN countries with the development status of countries, using the socio-demographic index (SDI) of each country. The SDI is a composite indicator of development status strongly correlated with health outcomes. It is the geometric mean of 0 to 1 indices of total fertility rate under the age of 25, mean education for those ages 15 and older, and lag distributed income per capita. As a composite, a country with an SDI of 0 would have a theoretical minimum level of development relevant to health, while a country with an SDI of 1 would have a theoretical maximum level [18]. Our study can provide a comprehensive perspective for better understanding the long-term trends and national differences in incidence and mortality from NTDM among China and ASEAN countries, which could help make global strategies to eliminate NTDM more scientific and sounder.
Methods
Study design
This is an observational study using data obtained from the GBD 2019 result tools. Annual number of incident number, incidences, death number, and mortality rates of neglected tropical diseases and malaria (NTDM) were extracted, by chosen specified diseases (malaria, cystic echinococcosis, dengue, and rabies) and the overall category. The socio-demographic index (SDI) of China and ASEAN countries from 1990 to 2019 was also extracted from the GBD 2019 result tools.
Data collection and processing
Data were obtained from the GBD 2019 result tools, established by the GBD group [19]. The general methodological approaches to estimate the mortality were described elsewhere. [20] Briefly, all available data on causes of death or incidence were standardized and pooled into a single database used to generate cause-specific estimates by age, sex, year, and geography; then multiple models, such as cause of death ensemble modelling, disease model-Bayesian meta-regression, comorbidity correction and so on were used to estimate comparable data of different diseases across the world. [20]
We reported the incidence and death results of NTDM in China, ASEAN countries (Brunei, Cambodia, Indonesia, Laos, Malaysia, Myanmar, Philippines, Singapore, Thailand, and Vietnam) and the global total data from 1990 to 2019, and arranged incidence and death data into successive 5-year age intervals from < 5 years to 65–69 years, plus the 70 + years group.
Statistical analysis
Absolute incidence and death number represented the actual situation of NTDM in each country, and its relative change was defined as \(\frac{{Number}_{2019}-{Number}_{1990}}{{Number}_{1990}}\times 100\%\), which showed the overall change between 1990 and 2019. Age-standardized incidence rate (ASIR) and age-standardized mortality rate (ASMR), which were directly extracted from the GBD result tool, [19] were calculated by applying the age-specific rates to a GBD World Standard Population, and were used to compare populations with different age structures or for the same population over time in which the age profiles change accordingly.
Estimated annual percentage change (EAPC) was widely used to quantified the rate trend over a specific interval. A regression line was fitted to the natural logarithm of the rates (y = α + βx + ε, where y = ln(rate) and x = calendar year). EAPC was calculated as 100 × (eβ-1), with 95% confidence intervals (CIs) obtained from the linear regression model. In this study, overall EAPC was calculated by the annual ASIR and ASMR of each category of infectious diseases in China and ASEAN countries, and EAPC in different age groups was calculated by the age-specific incidence and mortality rate. The term “increase” was used to describe trends when the EAPC and its lower boundary of 95% CI were both > 0. In contrast, “decrease” was used when the EAPC and its upper boundary of 95% CI, were both < 0. Otherwise, the term “stable” was used.
Join-point regression model was conducted to evaluate the temporal trend in the ASIRs and ASMRs. The best-fitting points were identified by the slope of changing trend and connected a set of statistically linear models on a logarithmic scale, and the number of join points were determined with maximum of 5. The join-point regression model was listed as follow: \(E\left[y|x\right]={e}^{{\beta }_{0}+{\beta }_{1}x+{{\delta }_{1}\left(x-{\tau }_{1}\right)}^{+}+\dots +{{\delta }_{k}\left(x-{\tau }_{k}\right)}^{+}}\), where k denotes the number of turning points, τk denotes the unknown turning points, β0 denotes the invariant parameter, β1 denotes the regression coefficient, δk denotes the regression coefficient of the piecewise function of k. Annual percentage change (APC) and corresponding 95% CIs were obtained to quantify the piecewise trends of ASIR and ASMR.
Lastly, nonlinear regression (second order polynomial) was conducted to explore the association between SDI and ASRs in China and ASEAN countries throughout 1990 to 2019. A regression curve was fitted to the ASIR or ASMR (\(y=\alpha +\beta x+\gamma {x}^{2}\), where y = the value of ASRs and x = SDI).
All the statistical analyses were performed by the R program (version 4.4.1).
Results
Burden and temporal trends of NTDM in China and ASEAN countries from 1990 to 2019
The incidence and death number of NTDM in China and ASEAN together accounted for 4.40% and 4.12% of global cases in 1990, and 4.99% and 2.43% in 2019. In 2019, the largest incident number of NTDM was from China (6.11 million), followed by Indonesia (3.42 million) and Philippines (1.85 million). However, the largest death number of NTDM was from Indonesia (11,029), followed by Philippines (2870) and China (1860). (Table 1).
The overall NTDM ASIRs and ASMRs in China and ASEAN were lower than the global level in 2019. However, only two countries (Myanmar and China) had lower dengue ASIRs than the global level, and four countries (Indonesia, Philippines, Malaysia and Myanmar) had higher dengue ASMRs than the global level. As for the rabies, Myanmar had the highest ASIR (1.04 per 100,000) and ASMR (0.93 per 100,000) in 2019, followed by Philippines (ASIR = 0.37 per 100,000; ASMR = 0.36 per 100,000) and Laos (ASIR = 0.32 per 100,000; ASMR = 0.31 per 100,000). Indonesia had the third-highest ASIR (0.14 per 100,000) and the highest ASMR (0.02 per 100,000) of cystic echinococcosis in 2019. (Figs. 1 and 2).
While the ASIR decreased from 1990 to 2019 at global level and in most ASEAN countries, the ASIR of NTDM increased in China, Philippines, Singapore and Brunei, at a speed of an average 4.15% (95% CI 3.83–4.47%), 2.15% (1.68–2.63%), 1.03% (0.63–1.43%), and 0.88% (0.60–1.17%) per year. The ASIR of Dengue increased in most countries with the speediest in China (EAPC = 4.83%, 95% CI 4.57–5.09%), followed by Philippines (EAPC = 3.71%, 95% CI 3.40–4.03%). Additionally, the ASMR of dengue in Philippines also increased at a speed of an average 2.42% (95% CI 1.89–2.95%) per year from 1990 to 2019. (Table 1, Additional file 1: Tables S1 and S2, and Additional file 1: Fig. S1).
Although the NTDM ASIRs and ASMRs in most countries had overall downtrends from 1990 to 2019, there were some periods in which the ASIR and ASMR showed uptrends, according to the join-point regression results. The global ASIR of NTDM showed an uptrend from 2015 to 2019 (APC = 0.4%, 95% CI 0.1–0.7%). Same uptrends in recent years were also found in China (from 2014 to 2017, APC = 10.4%, 95% CI 6.1–14.9%), Laos (from 2005 to 2013, APC = 3.9%, 95% CI 2.5–5.3%), Malaysia (from 2010 to 2015, APC = 4.3%, 95% CI 3.6–5.1%), Philippines (from 2015 to 2019, APC = 4.2%, 95% CI 3.7–4.8%), Thailand (from 2015 to 2019, APC = 2.4%, 95% CI 1.9–2.8%), and Vietnam (from 2014 to 2017, APC = 3.2%, 95% CI 1.5–4.9%). The ASMR of NTDM in China and ASEAN countries had not shown uptrends in recent years except Brunei, which showed an uptrend of NTDM ASMR from 2008 to 2016 (APC = 1.3%, 95% CI 1.0–1.7%). (Table 2) Additionally, ASIR and ASMR of dengue also showed uptrends in recent years in most countries: ASIR in China (APC = 10.4% from 2014 to 2017), Cambodia (APC = 5.1% from 2017 to 2019), Philippines (APC = 5.2% from 2016 to 2019), Thailand (APC = 2.4% from 2015 to 2019) and Vietnam (APC = 4.4% from 2014 to 2017); and ASMR of dengue in Cambodia (APC = 1.2% from 2010 to 2019), Laos (APC = 13.1% from 2016 to 2019), Singapore (APC = 4.2% from 2004 to 2019) and Vietnam (APC = 1.1% from 2001 to 2019). Notably, ASMR of dengue in Philippines had an uptrend throughout 1990 to 2019 (APC = 2.5%, 95% CI 2.0–3.1%). Moreover, ASIR of malaria in Laos (APC = 10.5% from 2011 to 2015) and Malaysia (APC = 28.0% from 2015 to 2019) also showed uptrends in recent years. (Additional file 1: Table S3).
Sex and age differences of NTDM in China and ASEAN countries
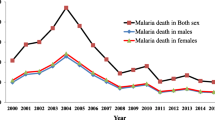
As shown in Fig. 3, the incident number of NTDM was close in the male and the female from 1990 to 2019, in China and ASEAN countries. In 2019, there were a total of 7.36 million women and 7.11 million men infected by NTDM in China and ASEAN countries. The death number of women was larger than men in 1990 (21,939 women vs 20,638 men), yet smaller in 2019 (7708 women vs 10,447 men). The cases and deaths of rabies of women were much less than men throughout 1990 to 2019. (Additional file 1: Fig.S2).
The global incidences of NTDM decreased with age, however, the incidence of NTDM in China and ASEAN countries were higher in 25–29 years group in 1990 and 15–29 years groups in 2019, both increasing in the oldest age group. The age distribution of global NTDM mortality rates was the same as that in China and ASEAN countries: higher in the youngest and oldest age groups, in 1990 and 2019. Philippines had the highest incidences of NTDM in most age groups, and Indonesia had the highest mortality rates of NTDM in most age groups. (Fig. 4) In China and ASEAN countries, cystic echinococcosis showed lower incidences of younger and older people, yet higher mortality rates of younger and older people. The age distribution of dengue and malaria was similar to cystic echinococcosis, with dengue mortality rates of children under the age of 5 much higher than other age groups, and malaria mortality rates of people aged 15–20 also relatively higher. Incidence and mortality rates of rabies were much higher in adolescence aged 10–15 than other age groups. (Additional file 1: Fig. S3).
Age-specific incidence and mortality rates of neglected tropical diseases and malaria in China and ASEAN countries, in 1990 and 2019. The global line fits the right Y axis, and other lines fit the left axis. a Incidence (per 100,000) in 1990; b Incidence (per 1990) in 2019; c Mortality rate (per 100,000) in 1990; d Mortality rate (per 100,000) in 2019
All the age groups in China and Philippines had uptrends in incidences of NTDM from 1990 to 2019, with the speediest increase in 20–24 years group in China (EAPC = 5.34%, 95% CI 5.05–5.63%) and 15–19 years group in Philippines (EAPC = 3.34%, 95% CI 2.77–3.92%). Most age groups in Brunei and Singapore also showed uptrends in incidences of NTDM from 1990 to 2019, with the speediest increase in 40–44 years group (EAPC = 1.39%, 95% CI 1.05–1.74%) and 35–39 years group in Singapore (EAPC = 1.67%, 95% CI 1.09–2.26%). Nevertheless, only a few age groups in certain countries had uptrends of NTDM mortality rates, such as 65–69 years group (EAPC = 5.42%, 95% CI 3.45–7.42%) and 70 + years group (EAPC = 5.37%, 95% CI 4.05–6.70%) in Singapore, 5–9 years group (EAPC = 1.81%, 95% CI 1.15–2.46%), 20–24 years group (EAPC = 0.81%, 95% CI 0.31–1.31%), 25–29 years group (EAPC = 0.74%, 95% CI 0.25–1.23%) and 70 + years group (EAPC = 0.74%, 95% CI 0.51–0.96%) in Brunei. (Fig. 5) The incidences of cystic echinococcosis increased in most age groups in China, with the speediest in children under the age of 5 (EAPC = 1.46%, 95% CI 1.17–1.75%); the mortality rates of dengue increased much speedier in Singapore than in other countries, with the speediest in 70 + years group (EAPC = 24.11%, 95% CI 20.30–28.04%); and both incidence (EAPC = 6.35%, 95% CI 4.23–8.52%) and mortality (EAPC = 7.14%, 95% CI 3.94–10.43%) rates of rabies increased in children under the age of 5 in Singapore. (Additional file 1: Fig. S4).
The association between SDI and ASRs of NTDM in China and ASEAN countries
Overall, the ASIR and ASMR of NTDM had a U-shaped association with SDI in China and ASEAN countries, with the peak point appearing SDI around 0.69 for ASIR and 0.91 for ASMR. (Fig. 6) The ASMR of cystic echinococcosis also had a U-shaped association with SDI, with the peak point appearing SDI around 0.70. The ASIR and ASMR of malaria had a U-shaped association with SDI, with the peak point appearing SDI around 0.70 for ASIR and 0.78 for ASMR. The ASIR and ASMR of rabies also had a U-shaped association with SDI, with the peak point appearing SDI around 0.75 for ASIR and 0.74 for ASMR. (Additional file 1: Fig. S5).
The correlation between age-standardized incidence and mortality rates of neglected tropical diseases and malaria and socio-demographic index in China and ASEAN countries. a association of Age-standardized incidence rate with socio-demographic index; b association of Age-standardized mortality rate with socio-demographic index
Discussion
To the best of our knowledge, this is the first comprehensive effort to describe the incidence and death of NTDM in China and ASEAN countries, also estimating their long-term trends throughout the past three decades, and accessing the association of the incidence and mortality rates of NTDM with the socio-demographic index. China, Indonesia and Philippines were countries with huge absolute incidence and death number of NTDM. Though the ASIRs and ASMRs of NTDM in China and ASEAN countries were lower than the global level, certain countries had higher ASIRs or ASMRs of dengue, rabies and cystic echinococcosis than the global level. ASIR of NTDM had an overall uptrend in China, Philippines, Singapore and Brunei from 1990 to 2019, while the NTDM ASIRs and ASMRs in most countries had overall downtrends from 1990 to 2019. However, there were some periods, especially recent years, in which the ASIR and ASMR showed uptrends, according to the join-point regression results. Sex disparity was not obvious in NTDM, but the incidence and death amount of rabies of women were much smaller than men throughout 1990 to 2019. The incidences of NTDM in China and ASEAN countries were higher in 25–29 years group in 1990 and 15–29 years group in 2019, both increasing in the oldest age groups; and the mortality rates were higher in both youngest and oldest groups. A U-shaped association of ASIR and ASMR of NTDM with SDI in China and ASEAN countries was also observed, indicating there were higher ASIR or ASMR in countries with the lowest and the highest SDI. Facing with the large burden and complex situation of NTDM in China and ASEAN countries, immediate and effective national cooperation are needed to reduce cases and deaths of NTDM and eliminate these diseases globally.
Our results, consistent with the findings of previous studies, [4, 16, 21,22,23] showed that the burden of dengue and rabies in China and ASEAN countries was above the world average level. Among China and ASEAN countries, Philippines and Indonesia had the highest ASIR (1619.95 per 100,000) and the highest ASMR (4.71 per 100,000) in 2019, respectively; and both ASIR and ASMR of rabies in Myanmar was the highest throughout 1990 to 2019. Meanwhile, the tremendous number of dengue cases in China also brought great concern. Furthermore, during the COVID-19 pandemic, the rate of dengue has continuously increased in ASEAN countries [21]. Climate change affects the survival and dispersion of Aedes aegypti and Aedes albopictus and transmission rates of viral pathogens of dengue [24], yet it was recommended to change vector control strategies during the epidemic wet seasons into a whole year to optimize the economic cost and burden of dengue and other arboviral diseases. [25] One of the effective ways to prevent the spread of dengue is the installation of water pipelines to residents in rural mountains to prevent mosquitoes from breeding in stored water [25, 26]. Besides, the dengue vaccine in Philippines, called Dengvaxia, which had a pooled efficacy amounting to 65.6% decrease in dengue with symptoms in people aged nine or older, could also serve as way of preventing dengue fever [27, 28]. Although Myanmar has made impressive progress against many infectious diseases, rabies was responsible for more deaths in Myanmar than malaria in recent years [22, 29]. In Myanmar, as well as in Cambodia, there was no national rabies program or coordinated canine vaccination campaign [23]. Therefore, appropriate fundings and integration of effective disease prevention strategies are necessary in Myanmar and other countries with rabies endemicity.
Despite the overall downtrends of NTDM burden from 1990 to 2019, certain diseases showed uptrends in recent years in China and ASEAN countries, according to the join-point regression results of our study. The increasing ASIR of NTDM in China (2014–2017), Malaysia (2010–2015), Philippines (2015–2019), Thailand (2015–2019), and Vietnam (2014–2017) addressed importance of taking more multifaceted and multisectoral actions to reduce the burden of NTDM in China and ASEAN countries to meet the global elimination goal [13]. One of the principles that WHO’s 2030 NTD elimination road map adopted is ‘leave no one behind’, which means taking explicit steps to end extreme poverty, curb inequalities, confront discrimination and fast track progress for the furthest behind [30]. Since almost 30% of the population in ASEAN countries were living in extreme poverty, the ‘leave no one behind’ principle could help reverse the uptrends of NTDM burden in China and ASEAN countries.
Our results showed that children under the age of five had relatively low incidences but unexpectedly high mortality rates of NTDM in most ASEAN countries, especially in Indonesia, Philippines and Myanmar. Additionally, both incidence and mortality rates of NTDM were higher in older people. On the one hand, NTDM affects children’s livelihoods in ASEAN countries. Helminthic infections with Trichuris trichiura or Ascaris lumbricoides were statistically associated with anemia and iron deficiency anemia, leading to incidences of low-birth-weight infants and inadequate growth and mental development in children, as well as high maternal mortality and low productivity in adults [31]. In Philippines in 2013, about 500,000 school-aged children required preventive chemotherapy for schistosomiasis [32]. Enterovirus 71 caused meningoencephalitis and Hand-Foot-and-Mouth disease in children, which could lead to fatal cases [33]. On the other hand, with decreased immunity and other underlying diseases, the prevention strategies of NTDM for elderly population were also in urgent needs.
This study also observed a U-shaped association of ASIR and ASMR of NTDM with SDI in China and ASEAN countries, with the peak point appearing SDI around 0.69 for ASIR and 0.91 for ASMR. The ASIR became higher when the SDI was over 0.69 might be because countries with the highest SDI, including Singapore and Brunei, had increased ASIR of NTDM over time. Unchecked urbanization without sanitation could promote the emergence of urban helminth infections [34]. It was reported that China, Malaysia and Singapore had mostly failed to shift their attention towards new innovations for the neglected tropical diseases, including new drugs, diagnostics, vaccines and vector control. This fact might lead these countries beset by widespread antimicrobial resistance, emerging arbovirus infections, and urban helminth infections [35]. Besides, political instability, conflict and human migrations in Myanmar and in and around the South China Sea could also make China and ASEAN countries important reservoirs for NTDM [36, 37]. Therefore, researchers have to look to the development of new or improved technologies for the prevention of vulnerable and impoverished populations.
Our study had some limitations. First, we described the overall situation of NTDM in China and ASEAN countries, but only four individual diseases were reported, due to the statistical characteristics of GBD results. Additionally, some important regional diseases such as melioidosis, chikungunya, and Japanese encephalitis have no estimation in the GBD [35]. Second, data from GBD results was estimated by several models, and the real burden of NTDM could be underestimated [20]. Nevertheless, our findings could alert the world that it was of vital importance to take regional cooperation to control NTDM, especially during the COVID-19 pandemic.
Conclusions
The burden of NTDM in China and ASEAN countries was still huge and affects vulnerable and impoverished populations’ livelihoods, including children under the age of 5 and people aged 60 and older. There was an urgent need of actions to reverse the uptrends of incidence and mortality rates of NTDM, including dengue, malaria, rabies and cystic echinococcosis in recent years, in certain countries. Despite the difficulties, immediate and effective actions need to be taken to make China and ASEAN countries—which have different types of political intuitions, different religions, various levels of economic development, and different types of health systems—establish a regional cooperating strategy to reduce the burden of NTDM, so as to achieve the goal of elimination of these diseases in the world.
Availability of data and materials
Data are available from the corresponding author by request.
References
JAIF Management Team. ASEAN Centre for Public Health Emergencies and Emerging Diseases (ACPHEED). 2022. https://jaif.asean.org/whats-new/asean-center-for-public-health-emergencies-and-emerging-diseases-acpheed/ (Accessed 2 October 2022).
Teerawattananon Y, Dabak SV, Isaranuwatchai W, et al. What can we learn from others to develop a regional centre for infectious diseases in ASEAN? Comment on “operationalising regional cooperation for infectious disease control: a scoping review of regional disease control bodies and networks.” Int J Health Policy Manag. 2022. https://doi.org/10.34172/ijhpm.2022.7281.
Lei XH. The 30th anniversary of the establishment of China-ASEAN dialogue relations: development, experiences and future. Asia-Pacific Security and Maritime Affairs 2022; 1: 61-82. https://doi.org/10.19780/j.cnki.ytaq.2022.1.5.
Hotez PJ, Bottazzi ME, Strych U, et al. Neglected tropical diseases among the Association of Southeast Asian Nations (ASEAN): overview and update. PLoS Negl Trop Dis. 2015;9(4):e0003575. https://doi.org/10.1371/journal.pntd.0003575.
World Health Organization. Dengue and severe dengue. 2022. https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue (Accessed 2 October 2022).
Shepard DS, Undurraga EA, Halasa YA. Economic and disease burden of dengue in Southeast Asia. PLoS Negl Trop Dis. 2013;7(2):e2055. https://doi.org/10.1371/journal.pntd.0002055.
Liu Q, Jing W, Kang L, Liu J, Liu M. Trends of the global, regional and national incidence of malaria in 204 countries from 1990 to 2019 and implications for malaria prevention. J Travel Med. 2021;28(5):taab046. https://doi.org/10.1093/jtm/taab046.
World Health Organization. World Malaria Report 2022. 2022. https://www.who.int/publications/i/item/9789240064898 (Accessed 11 January 2023).
Leow BL, Khoo CK, Syamsiah AS, Roslina H, Faizah HMS. Phylogenetic analysis of nucleoprotein gene of Rabies virus in Malaysia from 2015 to 2018. Trop Biomed. 2021;38(2):72–8.
Fu ZF. The rabies situation in Far East Asia. Dev Biol. 2008;131:55–61. https://doi.org/10.47665/tb.38.2.043.
Dimaano EM, Scholand SJ, Alera MT, Belandres DB. Clinical and epidemiological features of human rabies cases in the Philippines: a review from 1987 to 2006. Int J Infect Dis. 2011;15(7):e495–9. https://doi.org/10.1016/j.ijid.2011.03.023.
Lin Y, Fang K, Zheng Y, Wang HL, Wu J. Global burden and trends of neglected tropical diseases from 1990 to 2019. J Travel Med. 2022;29(3):taac031. https://doi.org/10.1093/jtm/taac031.
United Nations. Transforming our world: the 2030 Agenda for Sustainable Development. 2015. https://sdgs.un.org/2030agenda (Accessed 2 October 2022).
Collaborators I-L. Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. Lancet. 2017;390(10111):2437–60. https://doi.org/10.1016/S0140-6736(17)32804-0.
World Health Organization. World malaria report 2019. 2019. https://apps.who.int/iris/rest/bitstreams/1262394/retrieve (Accessed 2 October 2022).
Du M, Jing W, Liu M, Liu J. The global trends and regional differences in incidence of dengue infection from 1990 to 2019: an analysis from the global burden of disease study 2019. Infect Dis Ther. 2021;10(3):1625–43. https://doi.org/10.1007/s40121-021-00470-2.
Institute for Health Metrics and Evaluation. The Global Burden of Disease: a critical resource for informed policymaking. 2018. https://www.healthdata.org/gbd/about (Accessed 2 October 2022).
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Socio-Demographic Index (SDI) 1950–2019. 2020. http://ghdx.healthdata.org/record/ihme-data/gbd-2019-socio-demographic-index-sdi-1950-2019 (Accessed 2 October 2022).
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. 2019. https://vizhub.healthdata.org/gbd-results/ (Accessed 2 October 2022).
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396(10258): 1204–22.
Wiyono L, Rocha ICN, Cedeño TDD, Miranda AV, Lucero-Prisno IDE. Dengue and COVID-19 infections in the ASEAN region: a concurrent outbreak of viral diseases. Epidemiol Health. 2021;43:e2021070. https://doi.org/10.4178/epih.e2021070.
Mu TT, Sein AA, Soe C, Phyu ANP, Kyi TT, Hanson J. Rabies in Myanmar: prevalent, preventable but not prioritized. Am J Trop Med Hyg. 2017;97(4):989–91. https://doi.org/10.4269/ajtmh.17-0198.
Fooks AR, Banyard AC, Horton DL, Johnson N, McElhinney LM, Jackson AC. Current status of rabies and prospects for elimination. Lancet. 2014;384(9951):1389–99. https://doi.org/10.1016/S0140-6736(13)62707-5.
Ryan SJ, Carlson CJ, Mordecai EA, Johnson LR. Global expansion and redistribution of Aedes-borne virus transmission risk with climate change. PLoS Negl Trop Dis. 2019;13(3):e0007213. https://doi.org/10.1371/journal.pntd.0007213.
Edillo F, Ymbong RR, Cabahug MM, et al. Yearly variations of the genetic structure of Aedes aegypti (Linnaeus) (Diptera: Culicidae) in the Philippines (2017–2019). Infect Genet Evol. 2022;102:105296. https://doi.org/10.1016/j.meegid.2022.105296.
Diniz DFA, de Albuquerque CMR, Oliva LO, de Melo-Santos MAV, Ayres CFJ. Diapause and quiescence: dormancy mechanisms that contribute to the geographical expansion of mosquitoes and their evolutionary success. Parasit Vectors. 2017;10(1):310. https://doi.org/10.1186/s13071-017-2235-0.
Dayrit MM, Mendoza RU, Valenzuela SA. The importance of effective risk communication and transparency: lessons from the dengue vaccine controversy in the Philippines. J Public Health Policy. 2020;41(3):252–67. https://doi.org/10.1057/s41271-020-00232-3.
Hadinegoro SR, Arredondo-García JL, Capeding MR, et al. Efficacy and long-term safety of a dengue vaccine in regions of endemic disease. N Engl J Med. 2015;373(13):1195–206. https://doi.org/10.1056/NEJMoa1506223.
Mu TT, Sein AA, Kyi TT, et al. Malaria incidence in Myanmar 2005–2014: steady but fragile progress towards elimination. Malar J. 2016;15(1):503.
Harvey D, Shu’aibu J, Debam MT, Aba AK, Torres-Vitolas CA. How can the neglected tropical disease community be inclusive and equitable in programme delivery? Reaching refugees and internally displaced persons through integrating a “leave no one behind” approach. Int Health. 2022;14(Suppl 2):ii33–7. https://doi.org/10.1093/inthealth/ihac010.
Ngui R, Lim YA, Chong KL, Sek CC, Jaffar S. Association between anaemia, iron deficiency anaemia, neglected parasitic infections and socioeconomic factors in rural children of West Malaysia. PLoS Negl Trop Dis. 2012;6(3):e1550. https://doi.org/10.1371/journal.pntd.0001550.
Leonardo L, Rivera P, Saniel O, et al. A national baseline prevalence survey of schistosomiasis in the Philippines using stratified two-step systematic cluster sampling design. J Trop Med. 2012;2012:936128. https://doi.org/10.1155/2012/936128.
AbuBakar S, Chee HY, Al-Kobaisi MF, Xiaoshan J, Chua KB, Lam SK. Identification of enterovirus 71 isolates from an outbreak of hand, foot and mouth disease (HFMD) with fatal cases of encephalomyelitis in Malaysia. Virus Res. 1999;61(1):1–9. https://doi.org/10.1016/s0168-1702(99)00019-2.
Hotez PJ. Global urbanization and the neglected tropical diseases. PLoS Negl Trop Dis. 2017;11(2):e0005308. https://doi.org/10.1371/journal.pntd.0005308.
Hotez PJ. The rise or fall of neglected tropical diseases in East Asia Pacific. Acta Trop. 2020;202:105182. https://doi.org/10.1016/j.actatropica.2019.105182.
Du RY, Stanaway JD, Hotez PJ. Could violent conflict derail the London declaration on NTDs? PLoS Negl Trop Dis. 2018;12(4):e0006136. https://doi.org/10.1371/journal.pntd.0006136.
Hotez PJ. The South China Sea and Its Neglected Tropical Diseases. PLoS Negl Trop Dis. 2016;10(3):e0004395. https://doi.org/10.1371/journal.pntd.0004395.
Acknowledgements
We appreciate the works by the GBD and international disaster database collaborators.
Funding
This work was supported by the National Science and Technology Project on Development Assistance for Technology, Developing China-ASEAN Public Health Research and Development Collaborating Center (grant number KY202101004). The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the paper.
Author information
Authors and Affiliations
Contributions
QL and WY searched the literature, CQ, MD, YW collected the data, QL analyzed the data, interpreted the results, and drafted the paper. JL conceived of the study, designed the study, supervised the study, and interpreted the results. QL, ML and JL revised the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
We declare no competing interests.
Supplementary Information
Additional file 1
. Supplementary tables and figures of Incidence and mortality trends of neglected tropical diseases and malaria in China and ASEAN countries from 1990 to 2019 and its association with the Socio-demographic Index.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, Q., Yan, W., Qin, C. et al. Incidence and mortality trends of neglected tropical diseases and malaria in China and ASEAN countries from 1990 to 2019 and its association with the socio-demographic index. glob health res policy 8, 22 (2023). https://doi.org/10.1186/s41256-023-00306-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41256-023-00306-1