Abstract
Functional constipation is a common public health problem which may reduce one’s level of productivity and quality of life. Chrononutrition profile involves the relationship between one’s circadian rhythm and the dietary pattern. The objective of this study is to explore the association between chrono nutrition profile and lifestyle pattern of constipated subjects. University teaching faculty (n = 364) was screened using a cross-sectional study design and purposive sampling technique. A pre-tested and validated structured questionnaire was administered to them bearing questions related to their constipation status, chrononutrition profile and lifestyle pattern including diet and physical activity. The data obtained was subjected to statistical analysis using JASP software 2022. The background information of the study participants revealed that most of the respondents were females (59.1%), married (73.1%) and stayed in nuclear families (62.1%) with a family income of > INR 123,322.00 (42.3%) and their age ranged between 35 and 64 years. Functional constipation was observed in 25% of the subjects (n = 90). Physical activity of the study subjects indicated that 83% and 17% were in the sedentary and mildly active categories respectively and it was significantly negatively correlated with presence of FC among the subjects (p < 0.05). No significant correlation was observed with constipation in terms of the working day profile, whereas in terms of a free day profile, chrono nutrition profile showed a significant association (p < 0.05). However, the type of diet consumed by the subjects did not show any significant association with the constipation profile. Functional constipation was observed in 1/4 of the study sample. The findings suggest an association with a poor chrono nutrition profile with the constipation status of the study population on a free day. Further advice can be given to subjects suffering from constipation to improve their lifestyle pattern consistently on both working and free days.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional constipation (FC) is a significant clinical and public health issue. It is a very common functional gastrointestinal condition that could have a major impact on both the cost and quality of life [1]. Constipation is not just a problem for the elderly; it may also affect people in their middle years and young adults. Hard stools or scybala (hard, inspissated stool), unsuccessful calls (wanting to but unable to), cylindrical and cracked or cylindrical and thick stools, frequency of bowel movements less than three times per week, and straining for more than 25% of the time are all considered to be objective and subjective indicators of constipation [2].
Constipation has a multifaceted pathogenesis, with particular emphasis on genetic predisposition, socioeconomic level, poor fiber intake, inadequate fluid intake, immobility, disruption of the hormone balance, drug side effects, or body structure [3]. An important requirement to consider when examining the eating habits and sleep schedule of constipation sufferers is their chrononutrition profile [4].
Based on the principles of chrononutrition principles, time restricted eating (TRE) is a practical and well-tolerated diet that has multiple beneficial health advantages [5]. However, more thorough research is required to verify these effects, comprehend their processes, and determine whether they have any bearing on human health [6]. Circadian rhythms control a large portion of the physiology of the gastrointestinal tract, including cell growth, motility, digestion, absorption, and electrolyte homeostasis [7].
The “chronotype” of a person influences chrononutrition. A person’s chronotype is an analysis of their circadian rhythm that is categorised based on whether they prefer the morning or the evening [8, 9]. An individual’s behavioural tendencies are impacted by chronotype [10]. An individual’s ‘morningness’ or ‘eveningness’ is determined by the time of day that they choose to sleep or perform their daily tasks. Individuals who exhibit eveningness are more likely to experience circadian misalignment between their internal circadian clock and their solitary behavioural rhythms, which could make them more likely to have an unhealthy eating pattern [11].
Chrononutrition is the study of how a person’s diet corresponds to their circadian rhythm, which includes their internal metabolism, including digestion and absorption, among others. It aligns with the principle of eating at the same times every day as your body. When dietary patterns are abnormal, the diet’s macronutrients, for example, may not be processed properly, which can result in weight gain and other metabolic issues. The chrono nutrition profile consists mostly of six questions, including the size of the largest meal consumed and the frequency and timing of meals, which have a significant impact on the circadian clock and circadian rhythm and ultimately lead to poor metabolism [12].
This significant study is the first to establish an association between constipation and chrononutrition. The study’s objective was to determine whether there existed any relationship between functional constipation and the chrononutrition profile and diet consumption pattern.
Materials and methods
Using a cross-sectional study design and purposive sampling technique, a university teaching faculty (n = 364) was screened. The subjects were given pre-tested, validated and structured questionnaires with questions regarding their physical activity profile, dietary habits and food frequency profile and their constipation status which included their stool frequency (times/week) and chrono nutrition profile. The dietary habits included questions on dietary practices and how frequently different food groups are consumed.
A subset of the population who were suffering from functional constipation (n = 40) as per the constipation screening procedure were subjected to a 24-h diet recall for 3 consecutive days to assess their dietary intake with respect to estimated average allowance (EAR) and recommended dietary intake (RDA) guidelines [13] and find the association between their nutritional profile with the presence of constipation.
With respect to the chrono nutrition profile [14], questions on six components (Fig. 1) were administered which included eating at night, time-restricted eating (TRE), eating patterns for breakfast, dinner, and the largest meal, as well as the interval between meals and sleep patterns on a free day, weekend, and weekday.
Parameters for assessing Chrono nutrition profile [14]
Statistical analysis
Statistical analysis was performed with JASP software (MAC version) 2022. Results were expressed in terms of mean values, number percent and standard deviation for the variables. Pearson correlation (r) was used to assess the associations between constipation status and type of diet consumed and their nutritional profile with respect to the macronutrients and fiber intake. Pearson correlation (r) was used to assess the associations between constipation status and physical activity. Chi square test (χ2) was used to assess the association between the constipation status chrono nutrition profiles on a free day, working day and holiday and food their frequency profile. The levels of significance (p) were assessed at values of 0.05, 0.01 and 0.001.
Results
A pre-tested validated semi-structured questionnaire was developed and 364 teaching staff from the University responded. The background information of the study participants revealed that most of the respondents were females (59.1%), married (73.1%) and stayed in nuclear families (62.1%) with a family monthly income of > INR 123,322.00 (42.3%) and their age ranged between 35 and 64 years (Table 1).
Table 2 depicts the exercise and physical activity patterns of the subjects, which revealed that 32% of the respondents were brisk walking > 30 min on a daily basis followed by 19% of the subjects who were following a daily yoga routine. Regular physical activity showed a significant negative correlation with the presence of FC among the teaching staff (p < 0.05). It also revealed that 70% of the subjects were sitting for more than 8 h in a day, which showed a positive significant association with the presence of functional constipation among the respondents (p < 0.01).
Table 3 reveals the dietary practises of the subjects. Fifty four percent of the subjects consumed less than 1 l of water each day, which was seen to have a strong significant negative association with the presence of FC (p < 0.01). Dietary practices such as chewing food also showed a significant negative association with the presence of FC (p < 0.05). Twenty five percent of the subjects used home remedies for relieving from FC. Among the natural treatments for constipation, warm water (42%) and isabgol or psyllium husk (32%) are frequently used by the subjects. The respondents said that milk (62%) and cereals (26%) were the top most foods of concern which might be a cause of FC for them. Most subjects didn’t practice eating out regularly and hence no significance was reported with presence of FC among the respondents.
Figure 2 revealed that 25% of the subjects (N = 90) were suffering from functional constipation as per the criterion < 3 stools/week and 23% subjects have a regular bowel movement.
The subjects were screened for chrononutrition profile on a working day and on a free day (Tables 4 and 5) which comprised of 6 questions. Appropriate marks were assigned as per the responses. Correlation with the constipation profile was assessed further to check for any associations. The results are expressed in terms of number percent.
According to the findings in Table 4, 17% of the subjects skipped their breakfast daily. The majority of respondents (50%) indicated that lunch is their largest meal of the day whereas 17% of the subjects stated breakfast to be their largest meal. No significant associations were recorded between any parameters with the presence of FC as well as the chrono nutrition profile on a working day with the presence of FC.
According to Table 5, 35% of the subjects skip their breakfast on a working day from which 23% was shown to have the presence of FC. Ninety five percent of the subjects considered lunch to be the largest meal of the day from which 45% was reported to have the presence of FC. Eighty three percent of the subjects reported a time gap of < 2 h between their last meal and sleep onset which showed a significant positive association with the presence of FC (p < 0.05).
Eighty five percent of the subjects who reported to have FC had their meals after 8 pm and this was seen to be significantly associated with the presence of FC among the subjects (p < 0.05). Mostly the subjects never woke up at night for snacking hence no significant association was reported with the presence of FC. However, the chrononutrition profile on a free day was shown to have a significant negative association with the presence of FC among the sedentary university teaching staff (p < 0.05) which suggested that the subjects tend to deviate from their working day lifestyle on a free day which result in poor chrono nutrition status or lifestyle pattern and can be a contributing factor for FC (Table 5).
The subjects were assessed for their dietary profile in terms of their type of diet consumed and macronutrients and dietary fiber measure. Figure 3 shows the % of subjects consuming different types of diets. Sixty two percent of the respondents followed a vegetarian diet, 26% adhered to a non-vegetarian diet, and 41% of the subjects followed other diets, which included Jain food, ovo-vegetarian food, or lacto-ovo vegetarian food.
Table 6 revealed 57% subjects suffering from FC were vegetarians, 21% were non-vegetarian and 11% followed other diets. No statistically significant association between the various types of diet consumed and the presence of FC.
Baseline data was collected for the dietary intake of the constipated subjects using 24 h recall method for 3 days (n = 40). Macronutrients such as carbohydrate, protein, fats, total dietary fiber, soluble and insoluble fiber were measured before supplementation trial. Table 7 presented the amounts of the nutrients expressed as % Estimated Average Requirements (EAR) and % Recommended Daily Allowance (RDA) of females as that is the predominant gender among this population. The respondents were having 68%, 110% and 141% of their energy, protein and carbohydrate intake respectively as per EAR. Total dietary fiber and soluble fiber were shown to have significant negative correlation with the presence of FC (p < 0.05).
Table 8 shows the frequency of consumption of various food groups and its association with the presence of FC. Milk and milk products (68%) were the most commonly consumed food group on a daily basis followed by fruits (46%) and vegetables including carrots onions.
The other food groups consumed upto 55% 2–3 times/week was whole (55%) and spilt pulses (52%) and green leafy vegetables (55%). Least consumed food group by the subjects were processed foods and artificial sweeteners. The population under study was predominantly vegetarians hence they almost never took nonveg (63%).
Chi square test was applied to determine the association between consumption of various food groups on a daily basis, 2–3 times/week and weekly with the constipation status of the subjects. Significant negative association was recorded with the consumption of whole pulses (p < 0.05), split pulses (p < 0.05), natural sweeteners (jaggery) (p < 0.01) with the presence of FC.
Majority of respondents consumed sugar < 2 tsp (40%) which was seen to have a positive association with the presence of FC (p < 0.05). Low intake of salt was recorded in the subjects (55%). Intake of salt showed a significant negative correlation with the presence of constipation among the respondents which indicated a lower intake of salt benefits from FC (p < 0.05).
Discussion
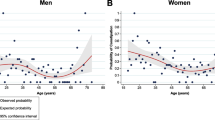
Functional constipation (FC) has a multifaceted pathogenesis, with particular emphasis on genetic history, socioeconomic level, poor fiber intake, inadequate fluid intake, immobility, disruption of the hormone balance, drug side effects, or body structure [15]. Literature review suggests that females are more prone to suffer from FC [16]. According to a study conducted by Verkuijl et al. [17], women experienced constipation substantially more frequently than males did (19.7% versus 10.6%, p < 0.001) which corroborated with the study’s findings where frequency of constipated female subjects was more than that of the male subjects (76% versus 25%, p < 0.0). Potential causes could be, for instance, women may have a slower intestinal transit and often report bowel function changes due to fluctuating amounts of progesterone and estrogen during their menstrual cycles, or it could be because they are more likely to report health issues than men.
These diagnostic criteria showed a presence of 20% of FC among the study population in the current study. However, if only Rome IV criteria was used, more number of subjects could have been diagnosed up to 94% (Rome IV). According to Dimidi et al. [18], there is little agreement between public perceptions of constipation and Rome IV criteria, and the opinions of general public on constipation varies noticeably from those of professional clinicians. These findings highlight the importance of educating medical professionals and the general public about constipation symptoms.
Studies indicate that bowel function can be improved with regular exercise [19]. Results observed in the current study shows that subjects with locomotor problems due to knee and joint pains were experiencing FC comparatively more than the others (p < 0.05) due to inactivity. A study by Yurtdas et al. [20] revealed that when compared to inactive participants, those who were moderately active (OR: 0.77, 95% CI: 0.62–0.91) and active (OR: 0.74, 95% CI: 0.59–0.90) had a reduced chance of constipation (p < 0.05).
A study by Almoosawi et al. [21] found that eating the largest meal earlier in the day or having a larger breakfast was more beneficial for improved body functions. A study by Yamada et al. [22] showed that during the 3-year period of research, missing breakfast and becoming sedentary, were linked to an increase in constipation status. Constipation and other digestive disorders have been linked to improper circadian rhythms in the gut [23]. A significant association (p < 0.05) was recorded for subjects for their sleeping pattern on a free day with constipation profile. As per Murakami and Tognini [24], delaying or skipping meals causes circadian misalignment which is observed among 10% of the subjects in case of breakfast as observed in the current study.
In addition to other factors, dietary factors like eating habits, food preferences, and intake of macro- and micronutrients have most frequently been shown to affect the activity of the gastrointestinal system [25]. The study’s findings indicated that there is no significant association between the presence of FC with the diet consumed which has been in debate in recent years. A common cause of FC is lack of fiber and water intake [26]. Similar results were obtained in the study which indicated that intake of insufficient drinking water, total fiber and soluble fiber was negatively associated with the presence of FC. Daily consumption of fibrous foods has been positively associated with the presence of constipation which was similar to our study with respect to consumption of pulses. As per NIN-ICMR recommendations (2020), [27] a total of 40 g of dietary fiber is recommended for a 2000 kcal diet. A ratio of 1:3 of soluble fiber to insoluble fiber for daily wellbeing is suggested as a dietary reference for Indians [28]. The current study revealed that the ratio of fiber consumed by the respondents was not at par with the guidelines and hence a significant negative association was recorded between fiber intake and the presence of FC (p < 0.05).
Conclusion
Functional constipation was prevalent among the teaching faculty in the university setup. Chrono nutrition profile which is composed of 3 elements of time including regularity, frequency and clock timing is significantly associated with the presence of constipation among the subjects on a free day. Further advice can be given to subjects suffering from constipation to follow a consistent lifestyle pattern on both working and free days for a healthier wellbeing. The findings also suggested no significant association between consumption of different diets with the constipation status of the study population. However, inclusion of soluble fiber in the diets has been significantly associated with the stool frequency per week. Salt and sugar intake however was linked to the constipation status, hence it is highly recommended to consume as per the guidelines.
Data availability
Data sets will be available upon request.
References
Wald A, Scarpignato C, Kamm MA, Mueller-Lissner S, Helfrich I, Schuijt C, Bubeck J, Limoni C, Petrini O. The burden of constipation on quality of life: results of a multinational survey. Aliment Pharmacol Ther. 2007;26:227–36. https://doi.org/10.1111/J.1365-2036.2007.03376.X.
Hyams J, Colleti R, Faure C, Gabriel-Martinez E, Maffei HV, Morais MB, Vandenplas Y. Functional gastrointestinal disorders: working group report of the first world congress of pediatric gastroenterology, hepatology and nutrition. J Pediatr Gastroenterol Nutr. 2002;35(2):110–7. https://doi.org/10.1097/00005176-200208002-00008.
Rajindrajith S, Devanarayana NM. Constipation in children: novel insight into epidemiology, pathophysiology and management. J Neurogastroenterol Motil. 2011;17(1):35–47. https://doi.org/10.5056/jnm.2011.17.1.35.
Duboc H, Coffin B, Siproudhis L. Disruption of circadian rhythms and gut motility: an overview of underlying mechanisms and associated pathologies. J Clin Gastroenterol. 2020;54(5):405–14. https://doi.org/10.1097/MCG.0000000000001333.
Świątkiewicz I, Woźniak A, Taub PR. Time-restricted eating and metabolic syndrome: current status and future perspectives. Nutrients. 2021;13(1):221. https://doi.org/10.3390/nu13010221.
Adafer R, Messaadi W, Meddahi M, Patey A, Haderbache A, Bayen S, Messaadi N. Food timing, circadian rhythm and chrononutrition: a systematic review of time-restricted eating’s effects on human health. Nutrients. 2020;12(12):3770. https://doi.org/10.3390/nu12123770.
Voigt RM, Forsyth CB, Green SJ, Mutlu E, Engen P, Vitaterna MH. Circadian disorganization alters intestinal microbiota. Cermakian N, editor. PLoS One. 2014;9(5):e97500. https://doi.org/10.1371/journal.pone.0097500.
Toktas N, Erman A, Mert Z. Nutritional habits according to human chronotype and nutritional status of morningness and eveningness. J Educ Train Stud. 2018;6(3a):61–7. https://doi.org/10.11114/jets.v6i3a.3159.
Henry CJ, Kaur B, Quek RYC. Chrononutrition in the management of diabetes. Nutr Diabetes. 2020;10:6. https://doi.org/10.1038/s41387-020-0109-6.
Almoosawi S, Vingeliene S, Gachon F, Voortman T, Palla L, Johnston JD, Van Dam RM, Darimont C, Karagounis LG. Chronotype: implications for epidemiologic studies on chrono- nutrition and cardiometabolic health. Adv Nutr. 2019;10(1):30–42. https://doi.org/10.1093/advances/nmy070.
Eid B, Bou SM, Melki I, Torbey PH, Najem J, Saber M, El ON, Rabbaa KL. Evaluation of chronotype among children and associations with BMI, sleep, anxiety, and depression. Front Neurol. 2020;11:416. https://doi.org/10.3389/fneur.2020.00416.
Bjelajac D, Đerčan B. Artificial light at night as an unrecognized threat to protected areas of autonomous province of Vojvodina (North Serbia). Zbornik radova Departmana za geografiju, turizam i hotelijerstvo. 2019;46–56. https://doi.org/10.5937/ZbDght1901046B
Nutrient requirements for Indians, recommended dietary allowances, estimated average requirements- a report of the expert group, 2020, ICMR NIN, Govt of India
Allison CE. Development, validation and reliability of the chrononutrition profile. North Dakota State University of Agriculture and Applied Sciences. 2018 (Dissertation)
Chen Z, Peng Y, Shi Q, Chen Y, Cao L, Jia J, Liu C, Zhang J. Prevalence and risk factors of functional constipation according to the Rome criteria in China: a systematic review and meta-analysis. Front Med. 2022;9:815156. https://doi.org/10.3389/fmed.2022.815156.
Forootan M, Bagheri N, Darvishi M. Chronic constipation: a review of literature. Medicine. 2018;97(20):e10631. https://doi.org/10.1097/MD.0000000000010631.
Verkuijl SJ, Meinds RJ, Trzpis M, Broens PMA. The influence of demographic characteristics on constipation symptoms: a detailed overview. BMC Gastroenterol. 2020;20:168. https://doi.org/10.1186/s12876-020-01306-y.
Dimidi E, Cox C, Grant R, Scott SM, Whelan K. Perceptions of constipation among the general public and people with constipation differ strikingly from those of general and specialist doctors and the Rome IV Criteria: perceptions of constipation diagnosis. Am J Gastroenterol. 2019;114(7):1116–29. https://doi.org/10.14309/ajg.0000000000000267.
Silveira EA, Santos ASEAC, Ribeiro JN, Noll M, Dos Santos Rodrigues AP, de Oliveira
C. Prevalence of constipation in adults with obesity class II and III and associated factors. BMC Gastroenterol. 2021;21(1):217. https://doi.org/10.1186/s12876-021-01806-5.
Almoosawi S, Vingeliene S, Karagounis LG, Pot GK. Chrono-nutrition: a review of current evidence from observational studies on global trends in time-of-day of energy intake and its association with obesity. Proc Nutr Soc. 2016;75(4):487–500. https://doi.org/10.1017/S0029665116000306.
Yamada M, Sekine M, Tatsuse T, Fujimura Y. Lifestyle, psychological stress, and incidence of adolescent constipation: results from the Toyama birth cohort study. BMC Public Health. 2021;21(1):47. https://doi.org/10.1186/s12889-020-10044-5.
Duboc H, Coffin B, Siproudhis L. Disruption of circadian rhythms and gut motility: an overview of underlying mechanisms and associated pathologies. J Clin Gastroenterol. 2020;54(5):405–14. https://doi.org/10.1097/MCG.0000000000001333.
Lee Y, Field JM, Sehgal A. Circadian rhythms, disease and chronotherapy. J Biol Rhythms. 2021;36(6):503–31. https://doi.org/10.1177/07487304211044301.
Mazri FH, Manaf ZA, Shahar S, Mat Ludin AF. The association between chronotype and dietary pattern among adults: a scoping review. Int J Environl Res Public Health. 2019;17(1):68. https://doi.org/10.3390/ijerph17010068.
Schneeman B. Food factors and gastrointestinal function: a critical interface. BioFactors. 2004;21(1–4):85–8. https://doi.org/10.1002/biof.552210116.
Corsetti M, Brown S, Chiarioni G, Dimidi E, Dudding T, Emmanuel A, Fox M, Ford AC, Giordano P, Grossi U, Henderson M, Knowles CH, O’Connell PR, Quigley EMM, Simren M, Spiller R, Whelan K, Whitehead WE, Williams AB, Scott SM. Chronic constipation in adults: contemporary perspectives and clinical challenges. 2: conservative, behavioural, medical and surgical treatment. Neurogastroenterol Motil. 2021;33(7):e14070. https://doi.org/10.1111/nmo.14070.
Nutrient requirements for Indians, recommended dietary allowances, estimated average requirements- a report of the expert group, 2020, ICMR NIN, Govt of India.
Funding
Self-funded.
Author information
Authors and Affiliations
Contributions
K.D. wrote the main manuscript and performed the research. M.S. guided the entire process and reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Institutional Ethics Committee for Human Research (IECHR), Faculty of Family and Community Sciences, The Maharaja Sayajirao University of Baroda. The ethical approval number of the study is IECHR/FCSc/PhD/2021/3. Written informed consent was obtained to participate in the study.
Competing interests
The authors declare no competing interests.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sheth, M., Dey, K. Role of chrononutrition and lifestyle factors in functional constipation. Nutrire 49, 7 (2024). https://doi.org/10.1186/s41110-024-00253-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41110-024-00253-y