Abstract
Background
Acute intracerebral hemorrhage (ICH) heterogeneity on NCCT, characterized by qualitative and quantitative methods, is predictive of hematoma expansion and mortality however association with the spot sign is not well-described. We sought to validate and determine the association between qualitative and quantitative hematoma heterogeneity with expansion and the spot sign, respectively.
Methods
We retrospectively studied 71 ICH patients presenting <24 h post-ictus with baseline NCCT, CTA and 24-hour follow-up CT available. Baseline NCCT was assessed qualitatively for presence of swirl sign or hematoma heterogeneity by two independent readers blinded to CTA findings and quantitatively using CT densitometry (CTD). Associations with 24-hour hematoma expansion ≥6 ml or ≥33 % and spot sign were assessed using logistic regression and diagnostic performance was assessed. Association between qualitative and quantitative densitometry parameters was also examined.
Results
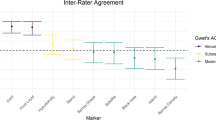
Swirl sign and quantitative CTD standard deviation were independently associated with expansion on multivariable analysis (p = 0.037 and p = 0.032, respectively). Swirl sign and hematoma heterogeneity were predictive of CTA spot sign (p = 0.020 and p = 0.035, respectively) while CTD standard deviation demonstrated only trend univariate association. CTD parameters were not significantly associated with swirl sign while only CTD skewness was associated with hematoma heterogeneity. Agreement for swirl sign and hematoma heterogeneity identification was nearly perfect (κ = 0.81) and substantial (κ = 0.79) respectively.
Conclusion
NCCT qualitative parameters predict hematoma expansion and CTA spot sign presence. Quantitative markers independently predict hematoma expansion but not CTA spot sign presence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Hematoma expansion occurs in up to 73 % of patients with primary intracerebral hemorrhage (ICH) and is independently associated with early neurological deterioration, death, and disability [1, 2]. Prevention of expansion is an attractive therapeutic target however improved means for expansion prediction are needed to guide potential acute interventions [3, 4]. Previous studies have identified heterogeneity or low-attenuation within a hematoma on hyperacute NCCT, coined the ‘swirl sign’, to be predictive of expansion and poor outcome [5–11]. Hematoma heterogeneity may partially reflect the presence of active extravasation within the hematoma in which uncoagulated blood appears iso- or hypodense relative to the brain parenchyma on CT [11]. Quantitative hematoma heterogeneity analysis using CT densitometry (CTD) is theoretically more robust, reproducible, and less prone to interpretation bias compared to qualitative techniques [5, 6]. CTD may also facilitate rapid and reliable expansion prediction in the acute setting using semi-automated techniques [12]. Recently CTD parameters, including the coefficient of variation (CV) and standard deviation (SD), were found be predictive of hematoma expansion independent of initial ICH volume and time from symptom onset [6]. These promising results however have yet to be validated. The association between qualitative and quantitative parameters of hematoma heterogeneity and the CTA spot sign, a potent marker of active hemorrhage expansion [13, 14], has also not been well-studied. NCCT predictors of hematoma expansion and the CTA spot sign could theoretically mitigate the need for CTA in patients at low risk of harboring vascular lesions or alert the clinician to the suspicion of underlying CTA spot sign and potentially facilitate earlier prothrombotic or hypotensive management thereby reducing the magnitude of expansion [15]. Importantly, many centers especially in the community do not or cannot perform emergent CTA in the setting of acute ICH. We therefore attempted to validate the association between quantitative and qualitative hematoma heterogeneity, hematoma expansion and the CTA spot sign in an acute ICH population. We further sought to determine the association between quantitative CTD parameters and qualitatively assessed hematoma heterogeneity.
Methods
Study cohort
Sunnybrook Hospital Research ethics board approved study retrospectively reviewed all ICH patients entered into a departmental stroke database between September 2010 and December 2012. Study inclusion criteria were all patients presenting to our tertiary care hospital emergency department with stroke symptoms attributable to primary ICH demonstrated on non-contrast CT with follow-up 24-hour CT available. Patients with evidence of secondary ICH such as ICH from trauma, aneurysm, vascular malformation, hemorrhagic transformation of ischemic stroke, venous sinus thrombosis and tumor were excluded. Patients with isolated intraventricular hemorrhage (IVH) were also excluded. Of 106 eligible cases, 35 were excluded due to lack of 24-hour follow-up (n = 6), surgical intervention before follow-up (n = 12), administration of recombinant factor VIIa (n = 2), isolated IVH (n = 4), unknown time of onset (n = 4), and poor scan quality/motion artifact (n = 7). Seventy-one (67 %) patients were therefore included in final analysis.
Clinical data
Baseline variables were recorded in an ICH database at time of presentation and any missing data retrieved by chart review. Clinical variables included were: patient age, gender, history of anticoagulation or hypertension, baseline neurological status (NIHSS), mean arterial blood pressure (MABP), time from symptom onset to baseline CT and follow-up. Hemoglobin, platelet and white blood cell count, serum glucose, International Normalized Ratio (INR) and partial thromboplastin time (PTT) were also recorded.
Image acquisition
All patients underwent standard institutional acute ICH CT protocol, performed on a 64-slice CT scanner (LightSpeed Plus and VCT; GE Healthcare), including baseline head NCCT, CTA of the neck and intracranial circulation, and follow-up 24-hour NCCT. All NCCT was performed from the skull base to the vertex with the following parameters: 120 kVp, 340 mA, 4 × 5 mm collimation, 1 s/rotation, and table speed of 15 mm/rotation. CTA studies were acquired from the aortic arch to the vertex in helical half-scan mode with the following parameters: 0.7 mL/kg of iodinated contrast (maximum 90 mL via antecubital fossa through 18- or 20-G angiocatheter), 120 kVp, 280 mA, 1 s/rotation, 1.25-mm section thickness at 0.625-mm intervals, and table speed of 3.75 mm/rotation. CTA contrast bolus timing was performed using SmartPrep (GE Healthcare) semi-automated attenuation-triggered technique.
Imaging analysis
Individual patient hematoma volumes and quantitative CTD parameters were measured from three-dimensional ROIs on baseline and follow-up NCCT studies. Measured CTD parameters included mean hematoma density in HU, SD, CV, skewness, and kurtosis [6]. ROIs were generated using a semi-automated seeding algorithm coded in MATLAB (Version R2012b; MathWorks, Natick, Massachusetts). The ROI generation algorithm started with an operator selected seed ROI created within the confines of the hematoma and then was coded to expand into adjacent voxels meeting a minimum attenuation threshold set to 44 HU. A secondary ROI growth phase was used to expand up to 3 voxels further with minimum attenuation threshold of 38 HU in order to adequately capture the hematoma periphery and lower density details within the hematoma. Low-density voxels inside the hematoma not meeting minimum threshold attenuation, potentially representing swirl signs, were included in the ROI by a reverse growing algorithm which included all voxels not connected with the exterior of the hematoma on each axial slice. Manually defined ROI margin constraints were applied where the hematoma margins were contiguous with adjacent bone, dura, or intraventricular hemorrhage. Accuracy of all ROIs was validated by a staff neuroradiologist (XX) with 10 years of experience. Hematoma volumes were compared against the validated Quantomo technique [12, 14] for a subset of 28 cases to further ensure accuracy. Hematoma appearance on NCCT was qualitatively assessed and dichotomized into homogeneous and heterogeneous appearance. All hematomas demonstrating enclosed regions that were iso- or hypodense to brain parenchyma were classified as heterogeneous. Heterogeneous hematomas were further subdivided into swirl sign positive or negative according to Selariu [9]. Specifically, the swirl sign was defined as an intrahematoma region of hypo or isoattenuation compared to the attenuation of brain parenchyma and may be rounded, streak-like, or irregular. If the heterogeneity was inconsistent with the swirl sign definition the hematoma was considered heterogeneous but swirl negative. To facilitate classification, standard windowing settings were used (width 30, level 30). CTA was assessed by the staff neuroradiologist for presence and number of spot signs by identifying intrahematoma contrast density on CTA, having either a serpiginous and/or spot-like appearance, without connection to an outside vessel [14, 16]. ICH location (ie. deep, lobar, and infratentorial) and IVH presence was also recorded. Baseline CT review was performed 8 weeks prior to assessment of 24-hour follow-up imaging results to avoid bias.
Statistical analysis
Outcomes for the study were 1) hematoma expansion, 2) presence of the spot sign, and 3) swirl sign and hematoma heterogeneity presence. Hematoma expansion was defined as ICH growth of >6 ml or >33 % from baseline to 24-hour CT [14, 17, 18]. Univariate associations between clinical and NCCT radiographic variables with hematoma expansion were assessed using bivariate logistic regression. Variables demonstrating significant or trend association (p < 0.10) were included in a multivariable logistic regression model using backwards stepwise selection. Predictors of the CTA spot sign and heterogeneity were also examined using the same approach. Prior to multivariable modelling, multicollinearity was assessed with the variance inflation factor statistic. Diagnostic performance of the swirl sign was assessed for hematoma expansion prediction with and without spot sign presence. Diagnostic performance of the swirl sign for spot sign prediction was also examined. Interobserver agreement of the swirl sign and heterogeneity was assessed using the Cohen’s κ statistic. Values of κ from 0.21 to 0.4, 0.41 to 0.6, 0.61 to 0.8, and 0.81 to 1 were considered fair, moderate, substantial, and nearly perfect, respectively [19]. Pearson’s correlation coefficient and intraclass correlation coefficient (ICC) compared baseline volumes obtained by the semi-automated ROI generation algorithm and the validated Quantomo technique [12]. ICC values of <0.4, 0.4 to 0.75, and >0.75 were considered to demonstrate poor, fair to good, and excellent agreement. Differences between included and excluded patients were examined with the Wilcoxon rank sum and χ 2 tests for continuous and categorical/dichotomous variables respectively. Statistical significance was defined as p < 0.05 for all tests. Statistical analysis was performed using SAS 9.2 (SAS Institute Inc, Cary, NC) and R, version 2.13.2 (http://www.r-project.org).
Results
Patient characteristics are summarized in Table 1. In brief, mean (SD) patient age was 68.2 ± 15.6 years and 46 (65 %) patients were male respectively. Median (interquartile range [IQR]) time from onset to baseline CT was 1.9 (1.3–4.6) hours and median (IQR) NIHSS at presentation was 10 (6–16). Hypertension and anticoagulation history was present in 57 (80 %) and 9 (13 %) patients respectively. Median (IQR) baseline ICH volume was 18.1 (5.3–37.6). Thirty-six (51 %) patients had a deep ICH location and 36 (51 %) had IVH.
There were no significant differences in patient age, gender, time from symptom onset to baseline CT, anticoagulation history, or baseline ICH volume between included and excluded patients (all p > 0.05). Excluded patients however had a greater IVH frequency (71 % vs. 51 %; χ 2 p = 0.042) and higher baseline NIHSS (median [IQR] 18 [8–23] vs. 10 [6–16]; p = 0.020). Semi-automated hematoma volume measurements demonstrated near perfect correlation and high agreement with the previously validated Quantomo technique [12] for baseline hematoma volume measurements (ρ = 0.90, 95 % CI 0.80–0.95; ICC 0.84, 95 % CI 0.68–0.92 respectively). Thirty-three (46 %) and 35 (49 %) patients demonstrated a swirl sign and heterogeneous hematoma respectively. Interobserver agreement for the swirl sign and qualitatively assessed hematoma heterogeneity was nearly perfect (κ = 0.81, 95 % CI 0.67–0.96) and substantial respectively (κ = 0.79, 95 % CI 0.63–0.93).
Prediction of hematoma expansion
Hematoma expansion of >6 ml or >33 % occurred in 21 (30 %) patients. Univariate associations between clinical and radiographic predictors of hematoma expansion are summarized in Table 1.
Significant NCCT predictors of hematoma expansion included swirl sign (OR 3.3, 95 % CI 1.2–10; p = 0.031) and CTD SD (OR 0.65, 95 % CI 0.43–0.94; p = 0.029). Additionally CTD CV (p = 0.059), CTD mean density (p = 0.052), and hematoma heterogeneity (p = 0.062) trended to significance. No significant clinical predictors of expansion were detected, although time from onset to baseline CT of <3 h (p = 0.059), and baseline INR >1.5 (p = 0.057) trended towards significance. Collinearity was noted between the swirl sign and hematoma heterogeneity in addition to CTD SD and CTD CV and accordingly these variables were assessed in separate multivariable models. Multivariable analysis including swirl sign and CTD SD in addition to other NCCT and clinical predictors of expansion with trend association yielded a final model including swirl sign (OR 3.3, 95 % CI 1.1–10.6; p = 0.037) and CTD SD (OR 0.66, 95 % CI 0.43–0.94; p = 0.032). Substitution of CTD CV for CTD SD yielded a final model including swirl sign (OR 3.8, 95 % CI 1.3–12.8; p = 0.020) and CTD mean density (OR 0.8, 95 % CI 0.70–0.97; p = 0.033). Substitution of swirl sign with hematoma heterogeneity in the multivariable regression with CTD SD or CTD CV yielded final models that included CTD SD alone or hematoma heterogeneity (OR 3.4, 95 % CI 1.1–11.2; p = 0.040) and CTD mean density (OR 0.84, 95 % CI 0.70–0.97; p = 0.032), respectively.
Multivariable model area under the curve ranged from 0.64 for the model with swirl sign alone to 0.73 for a model with swirl sign and CTD SD. There was no statistically significant difference in expansion discrimination between multivariable models.
Diagnostic performance of swirl sign and hematoma heterogeneity for hematoma expansion prediction with and without the presence of a spot sign are listed in Table 2.
Predictors of CTA spot sign
A CTA spot sign was present in 26 (37 %) patients. Significant NCCT predictors of the spot sign on univariate analysis included the swirl sign (OR 4.5, 95 % CI 1.6–12.7; p = 0.005) and heterogeneous hematomas (OR 4.9, 95 % CI 1.7–15; p = 0.003). Trend associations were noted for CTD SD (OR 0.73, 95 % CI 0.51–1.0; p = 0.067) and CTD CV (OR 0.01, 95 % CI 0.00–10.7; p = 0.076). Significant clinical predictors of spot sign presence included time from onset to baseline CT <3 h (OR = 9.6; 95 % CI = 2.0–46; p = 0.004) and NIHSS (OR 1.1; 95 % CI 1.0–1.2; p = 0.009). Collinearity was noted between the swirl sign and hematoma heterogeneity in addition to CTD SD and CV. Multivariable analysis including swirl sign and CTD SD in addition to other NCCT and clinical predictors of the spot sign with trend association demonstrated a final model including swirl sign (OR 3.2; 95 % CI 1.1–10; p = 0.020) and time from symptom onset to baseline CT <3 h (OR 7.1; 95 % CI 1.7–48; p = 0.035). Substitution of CTD CV for CTD SD yielded the same final model. Substitution of swirl sign with hematoma heterogeneity in multivariable regression with CTD SD or CTD CV yielded final models that included hematoma heterogeneity (OR 3.4, 95 % CI 1.1–11; p = 0.035) and time from symptom onset to baseline CT <3 h (OR 6.7, 95 % CI 1.6–46; p = 0.020). Both multivariable models demonstrated a model area under the curve of 0.75. Diagnostic performance of the swirl sign and hematoma heterogeneity for spot sign presence is demonstrated in Table 3.
Association between CTD parameters and qualitative hematoma heterogeneity
Univariate analysis between CTD predictors and the swirl sign and hematoma heterogeneity separately demonstrated trend association between CTD skewness and swirl sign (p = 0.079) and significant association CTD skewness and hematoma heterogeneity (OR 0.1, 95 % CI 0.01–0.63; p = 0.021). The remaining CTD parameters, including CTD SD, CV, mean, and kurtosis were not significantly associated with either outcome (all p > 0.10).
Discussion
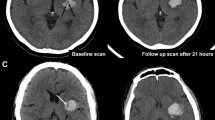
Previous studies of the swirl sign and hematoma heterogeneity in acute ICH, assessed both qualitatively and quantitatively on NCCT, demonstrated significant statistical associations with hematoma expansion [5, 6]. Our study findings are concordant with these findings demonstrating that both qualitative (swirl sign) and quantitative (CTD SD) measures independently predict hematoma expansion. Other quantitative predictors of expansion included CTD mean density and qualitative hematoma heterogeneity. For both CTD SD and CTD mean density, an inverse relationship with expansion was noted such that the risk of expansion was increased when either CTD SD or CTD mean density decreased as demonstrated in densitometry histograms from Fig. 1. The inverse relationship between CTD SD and greater hematoma expansion was also noted by Barras et al. in their previous CTD study of 81 acute ICH patients in the placebo arm of the Phase 2 recombinant Factor VIIa trial [6]. The same study identified CTD CV as the greatest individual predictor of expansion although this only demonstrated trend association in the present study (p = 0.059). The differences between the two studies remains unclear, but both studies confirm the potential for quantitative prediction of hematoma expansion.
a NCCT of deep right ICH (38 ml) with swirl sign (arrow). b Corresponding hematoma CT densitometry histogram (Mean HU 55.3, SD 9.7, CV 0.18, Skewness −0.26, Kurtosis 2.41). c CTA with multiple spot signs present (arrows). The patient subsequently underwent hematoma expansion of 41 ml. d NCCT of a different patient with right frontal lobar ICH (38 ml) and trace IVH. e Corresponding hematoma CT densitometry histogram (Mean HU 61.5, SD 12.2, CV 0.20, Skewness −0.64, Kurtosis 2.6). f CTA demonstrates no evidence of spot sign. The patient had a stable hematoma on 24-hour follow-up
To our knowledge, the association between the swirl sign, hematoma heterogeneity and the CTA spot sign is not previously studied. A significant association between the swirl sign and qualitative hematoma heterogeneity and the spot sign independent of time from symptom onset was demonstrated. These findings further support the importance of recognizing the swirl sign and hematoma heterogeneity for predicting spot sign presence. The inability of quantitative measures to predict the spot sign or the swirl sign but independent association with hematoma expansion suggests that qualitative and quantitative measures may be capturing different imaging features of potential for hematoma expansion. Therefore, optimal NCCT ICH expansion prediction, in the absence of CTA, may benefit from both qualitative and quantitative measures of hematoma heterogeneity. An important limitation of swirl sign recognition is that platelet-fibrin thrombi may mimic a swirl sign in vitro by reducing attenuation relative to retracted blood clot [20]. CTA may therefore be preferable, by facilitating direct contrast extravasation visualization. In the absence of CTA availability, the swirl sign and hematoma heterogeneity may however aide in hematoma expansion prediction.
Interobserver agreement of the swirl sign and hematoma heterogeneity was nearly perfect (κ = 0.81) and substantial (κ = 0.79), respectively, similar to results demonstrated by Selariu for the swirl sign (κ = 0.80). To facilitate high interobserver agreement, a pre-specified viewing window width and level of 30 and 30 respectively is recommended similar to strategies employed in NCCT evaluation for ischemic stroke and for CTA spot sign identification [17, 21]. Utilization of thin slice CT may further improve agreement or alter performance but requires further study [22]. Swirl sign prevalence was modestly higher in our study (46 %) compared to Selariu (30 %) and Kim (15 %). Previous radiological-surgical correlation studies in patients with traumatic extra-axial hematomas demonstrate that the swirl sign was associated with evidence of active bleeding at time of surgery evacuation, most commonly arterial hemorrhage [11, 23]. Extravasation of intravenous contrast both on post-contrast CT and conventional angiogram in epidural hematomas has also been shown and further support active bleeding in epidural hematomas [24, 25]. Recently in acute ICH patients, the spot sign was studied using a dynamic 60 s CTA acquisition and demonstrated evolving growth over time consistent with sites of active extravasation [13]. Our finding that swirl signs were associated both hematoma expansion and spot sign is consistent with these previous findings suggesting recent or on-going extravasation and potential risk for further expansion [20].
Our study was limited in sample size with a significant proportion of patients excluded due to surgical intervention, lack of adequate CT follow-up, or severe motion artifact at baseline. This limited our statistical power and number of variables allowable for multivariable analysis. This study was also performed retrospectively and further prospective study is required to determine whether these methods may be employed with high-interobserver agreement real-time in the acute setting. Variations in CT scanners may contribute to heterogeneity in CTD results and further validation in a multicenter setting with CT scanners from different models and manufacturers is needed [6]. The semi-automated ROI generation techniques used in this study demonstrated high correlation with the previously validated Quantomo technique but remains limited by the need for manual seed placement and tracing to prevent ROI extension into areas of IVH and dural or calvarial hematoma contact.
Conclusion
The NCCT swirl sign and hematoma heterogeneity are significantly associated with hematoma expansion and the CTA spot sign. CTD SD is the best CTD predictor of expansion however is not significantly associated with spot sign. In the absence of CTA availability, swirl sign and hematoma heterogeneity recognition may aide in hematoma expansion.
Abbreviations
- CTD:
-
CT densitometry
- CV:
-
Coefficient of variation
- ICC:
-
Intraclass correlation coefficient
- ICH:
-
Intracerebral hemorrhage
- INR:
-
International Normalized Ratio
- MABP:
-
Mean arterial blood pressure
- PTT:
-
Partial thromboplastin time
- IQR:
-
Interquartile range
- IVH:
-
Intraventricular hemorrhage
- SD:
-
Standard deviation
References
Davis SM, Broderick J, Hennerici M, Brun NC, Diringer MN, Mayer SA, et al. Hematoma growth is a determinant of mortality and poor outcome after intracerebral hemorrhage. Neurology. 2006;66:1175–81.
Brott T, Broderick J, Kothari R, Barsan W, Tomsick T, Sauerbeck L, et al. Early hemorrhage growth in patients with intracerebral hemorrhage. Stroke. 1997;28:1–5.
Huynh TJ, Symons SP, Aviv RI. Advances in CT for prediction of hematoma expansion in acute intracerebral hemorrhage. Imaging Med. 2013;5:539–51.
Mayer SA, Brun NC, Begtrup K, Broderick J, Davis S, Diringer MN, et al. Efficacy and safety of recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2008;358:2127–37.
Barras CD, Tress BM, Christensen S, MacGregor L, Collins M, Desmond PM, et al. Density and shape as CT predictors of intracerebral hemorrhage growth. Stroke. 2009;40:1325–31.
Barras CD, Tress BM, Christensen S, Collins M, Desmond PM, Skolnick BE, et al. Quantitative CT densitometry for predicting intracerebral hemorrhage growth. AJNR Am J Neuroradiol. 2013;34:1139–44.
Al-nakshabandi NA. The swirl sign. Radiology. 2001;218:433.
Kim J, Smith A, Hemphill JC, Smith WS, Lu Y, Dillon WP, et al. Contrast extravasation on CT predicts mortality in primary intracerebral hemorrhage. AJNR Am J Neuroradiol. 2008;29:520–5.
Selariu E, Zia E, Brizzi M, Abul-Kasim K. Swirl sign in intracerebral haemorrhage: definition, prevalence, reliability and prognostic value. BMC Neurol. 2012;12:109.
Smith SD, Eskey CJ. Hemorrhagic stroke. Radiol Clin North Am. 2011;49:27–45.
Zimmerman RA, Bilaniuk LT. Computed tomographic staging of traumatic epidural bleeding. Radiology. 1982;144:809–12.
Kosior JC, Idris S, Dowlatshahi D, Alzawahmah M, Eesa M, Sharma P, et al. Quantomo: validation of a computer-assisted methodology for the volumetric analysis of intracerebral haemorrhage. Int J Stroke. 2011;6:302–5.
Dowlatshahi D, Wasserman JK, Momoli F, Petrcich W, Stotts G, Hogan M, et al. Evolution of computed tomography angiography spot sign is consistent with a site of active hemorrhage in acute intracerebral hemorrhage. Stroke. 2014;45:277–80.
Demchuk AM, Dowlatshahi D, Rodriguez-Luna D, Molina CA, Blas YS, Dzialowski I, et al. Prediction of haematoma growth and outcome in patients with intracerebral haemorrhage using the CT-angiography spot sign (PREDICT): a prospective observational study. Lancet Neurol. 2012;11:307–14.
Anderson CS, Heeley E, Huang Y, Wang J, Stapf C, Delcourt C, et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368:2355–65.
Thompson AL, Kosior JC, Gladstone DJ, Hopyan JJ, Symons SP, Romero F, et al. Defining the CT angiography “spot sign” in primary intracerebral hemorrhage. Can J Neurol Sci. 2009;36:456–61.
Wada R, Aviv RI, Fox AJ, Sahlas DJ, Gladstone DJ, Tomlinson G, et al. CT angiography “spot sign” predicts hematoma expansion in acute intracerebral hemorrhage. Stroke. 2007;38:1257–62.
Dowlatshahi D, Demchuk AM, Flaherty ML, Ali M, Lyden PL, Smith EE. Defining hematoma expansion in intracerebral hemorrhage: Relationship with patient outcomes. Neurology. 2011;76:1238–44.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
New PF, Aronow S. Attenuation measurements of whole blood and blood fractions in computed tomography. Radiology. 1976;121:635–40.
Lev MH, Farkas J, Gemmete JJ, Hossain ST, Hunter GJ, Koroshetz WJ, et al. Acute stroke: improved nonenhanced CT detection--benefits of soft-copy interpretation by using variable window width and center level settings. Radiology. 1999;213:150–5.
Riedel CH, Zoubie J, Ulmer S, Gierthmuehlen J, Jansen O. Thin-Slice Reconstructions of Nonenhanced CT Images Allow for Detection of Thrombus in Acute Stroke. Stroke. 2012;43:2319–23.
Greenberg J, Cohen WA, Cooper PR. The “hyperacute” extraaxial intracranial hematoma: computed tomographic findings and clinical significance. Neurosurgery. 1985;17:48–56.
Helmer FA, Sukoff MH, Plaut MR. Angiographic extravasation of contrast medium in an epidural hematoma. Case report. J Neurosurg. 1968;29:652–4.
Palmieri A. Extravasation of contrast-enhanced blood in an epidural hematoma. Neuroradiology. 1981;21:163–4.
Acknowledgements
ᅟ
Grant support
Dr. Huynh was supported by a Canadian Institutes of Health Research Masters Award.
Dr. Dowlatshahi was supported by a Canadian Institutes of Health Research Fellowship Award and a University of Ottawa Department of Medicine Research Salary Award.
All remaining authors report no relevant disclosures.
Presentation
Part content of this manuscript was presented at the 2014 American Society of Neuroradiology Annual Meeting.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
Conceived and designed the research RIA, acquired the data DC, AD, TH, SS, DD, DG, SPS. Analyzed and interpreted the data DC, TH, RIA. Performed statistical analysis DC, TH, RIA. Handled funding and supervision DD, AD, RIA. Drafted the manuscript all authors. Made critical revision of the manuscript for important intellectual content all authors. All Authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Connor, D., Huynh, T.J., Demchuk, A.M. et al. Swirls and spots: relationship between qualitative and quantitative hematoma heterogeneity, hematoma expansion, and the spot sign. Neurovascular Imaging 1, 8 (2015). https://doi.org/10.1186/s40809-015-0010-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40809-015-0010-1