Abstract
Background
Necrotizing fasciitis in neonates is a rare and life-threatening infection involving necrosis of the skin, subcutaneous tissues, deep fascia, and sometimes underlying muscles, with a fulminant course and high mortality rate. Necrotizing fasciitis with gas gangrene related to infection of a peripherally inserted central catheter is very rare.
Case presentation
The patient was a full-term female neonate born by vaginal delivery. Following diagnosis of patent ductus arteriosus, indomethacin was administered from a peripherally inserted central catheter for 3 days. Four days after the termination of medical treatment for the patent ductus arteriosus, the patient developed fever and a severely elevated inflammatory response was identified from blood testing. Around the right anterior chest wall, corresponding to the site of the catheter tip, redness was increased and gas crepitus was felt under the skin. Computed tomography revealed emphysema in the anterior chest, in subcutaneous areas and between muscles. Emergency surgical debridement was performed under a diagnosis of necrotizing fasciitis with gas gangrene. With antibiotic treatment, we started to fill the wound with a dialkyl carbamoyl chloride-coated dressing and povidone-iodine sugar ointment after washing with saline once a day. The patient survived and after 3 weeks of treatment with the dressing, the wound had successfully resolved without motor impairments.
Conclusions
In addition to medical treatment and prompt surgical debridement, we used dialkyl carbamoyl chloride-coated dressing and povidone-iodine sugar ointment for antiseptic dressings and successfully treated neonatal necrotizing fasciitis with gas gangrene caused by peripherally inserted central catheter infection with Citrobacter koseri.
Similar content being viewed by others
Background
Necrotizing fasciitis (NF) in neonates is a rare and life-threatening infection involving necrosis of the skin, subcutaneous tissues, deep fascia, and sometimes underlying muscles. The course of NF is fulminant and the mortality rate is high, so rapid and aggressive surgical debridement is essential for treatment [1, 2]. Determining the strategy for wound care for infant cases of NF with gas gangrene related to peripherally inserted central catheter (PICC) infection is difficult because such cases are also very rare [3].
Case presentation
A female neonate was born at a gestational age of 39 weeks 1 day with a birth weight of 2825 g by vaginal delivery. She had been diagnosed with patent ductus arteriosus (PDA). From 5 days old, she received indomethacin for 3 days from a PICC in the neonatal intensive care unit (Fig. 1).
Four days after the termination of medical treatment for PDA, fever of 38–39 °C was found and severely elevated inflammatory response was identified from laboratory data, suggesting sepsis (white blood cell count, 61 × 102/μl; platelet count, 8.7 × 104/mm3; C-reactive protein, 28.3 mg/dl) was detected. Contrast-enhanced computed tomography (CT) immediately after removal of the PICC revealed emphysema in the anterior chest, in the subcutaneous area and between muscles (Fig. 2).
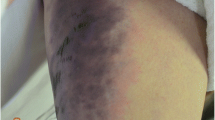
Around the right anterior chest wall, corresponding to the site of the catheter tip, redness was increased and gas crepitus was felt under the skin (Fig. 3a). At 12 days old, emergency surgery was performed under a diagnosis of NF with gas gangrene. A skin incision was made along the outer edge of the pectoralis major muscle from the ribcage to the point where the pectoralis major and biceps brachii muscles intersected. Deep emphysema was released by debridement of the necrotic fascia. No abscess was found inside the necrotic fascia (Fig. 3b). We filled the wound with dialkyl carbamoyl chloride (DACC)-coated dressing and povidone-iodine sugar ointment and changed these daily (Fig. 3c). She rarely cried due to pain during the procedure without medical pain control. The wound healing was rapid and there were no problems such as the residue of infections.
Intraoperative findings. Corresponding to the site of the catheter tip, marked redness of the skin was found (a). A pin-hole opening in the emphysema at the necrotic fascia is indicated by an arrow (b). Povidone-iodine sugar ointment is wrapped in a DACC-coated dressing and filled into the wound (c)
Carbapenem antibiotics and anti-methicillin-resistant Staphylococcus aureus glycopeptide antibiotics were administered until the pathogen was identified, then cephem antibiotics were administered after Citrobacter koseri was detected from blood culture and PICC tip culture tests. As a result of 3-week treatment with these dressing materials, the patient recovered well and the wound was successfully cured without motor impairments (Fig. 4).
Discussion
NF has multiple causes, risk factors, anatomical locations, and pathogenic mechanisms, but all infections in this disease involve a wide range of tissues that can extend from the epidermis to the deep musculature [4]. In adults, NF is common among patients such as those with diabetes, but healthy children can also be affected by initiating factors. Early and aggressive surgical debridement is the most important component of management, given the life-threatening nature of this infection, and delaying operation for more than 24 h reportedly doubles the mortality rate [5].
In neonatal NF, above all, early diagnosis and emergent surgical debridement are essential for patient survival because the mortality rate is high [1, 2]. Magnetic resonance imaging (MRI) is useful for diagnosing NF [6], but contrast-enhanced CT may be suitable for neonatal emergency cases because MRI imaging takes time. In this case, we tried using two materials, DACC-coated dressing and povidone-iodine sugar ointment, for wound care to treat this condition safely and effectively and obtain successful outcomes.
DACC-coated dressings reportedly show strongly hydrophobic properties and wound bacteria also have hydrophobic characteristics, so they become physically bound to the dressing fibers and are subsequently removed from the wound when the dressing is changed without charging the wound with a chemically active agent [7]. It is also described that the use of this product contributes to the improvement of the pain symptoms [7].
No previous reports appear to have described the use of DACC-coated dressings in neonatal NF cases.
Povidone-iodine sugar ointment is widely used for incurable infectious wounds, activating fibroblasts and promoting wound healing. The effectiveness of this ointment in improving wound healing has been proven in clinical surgical wounds [8].
From the results of blood culture testing and PICC tip culture test, we finally concluded the pathogen in this case was C. koseri, a Gram-negative rod known as a pathogen in neonatal meningitis. While non-central nervous system infections are rare [9, 10], we should be vigilant for C. koseri as a potential causative organism.
Conclusions
Accurate diagnosis, appropriate antibiotics, prompt and aggressive surgical debridement and effective wound management allowed successful management of this unusual case of neonatal NF with gas gangrene caused by PICC infection.
Availability of data and materials
Not applicable.
Abbreviations
- CT:
-
Computed tomography
- DACC:
-
Dialkyl carbamoyl chloride
- MRI:
-
Magnetic resonance imaging
- NF:
-
Necrotizing fasciitis
- PDA:
-
Patent ductus arteriosus
- PICC:
-
Peripherally inserted central catheter
References
Hsieh WS, Yang PH, Chao HC, Lai JY. Neonatal necrotizing fasciitis: a report of three cases and review of the literature. Pediatrics. 1999;103: e53.
Nazir Z. Necrotizing fasciitis in neonates. Pediatr Surg Int. 2005;21:641–4.
Inoue M, Miyazaki N, Suematsu H, Yamagishi Y, Mikamo H. Necrotizing fasciitis on a peripherally inserted central venous catheter site. Pediatr Int. 2020;62:1303–4.
Wilson B. Necrotizing fasciitis. Am Surg. 1952;18:416–31.
Barton LL, Jeck DT. Neonatal necrotizing fasciitis in children: report of two cases and review of literature. Arch Pediatr Adolesc Med. 1996;150:105–8.
Ali SZ, Srinivasan S, Peh WCG. MRI in necrotizing fasciitis of the extremities. Br J Radiol. 2014;87:20130560.
Kammerlander G, Locher E, Suess-Burghart A, von Hallern B, Wipplinger P. An investigation of Cutimed® Sorbact® as an antimicrobial alternative in wound management. Wounds UK. 2008;4:10–8.
Kuntson RA, Merbitz LA, Creekmore MA, Snipes HG. Use of sugar and povidone-iodine to enhance wound healing: five years’ experience. South Med J. 1981;74:1329–35.
Gross RJ, Rowe B, Easton A. Neonatal meningitis caused by Citrobacter koseri. J Clin Path. 1973;26:138–9.
Ribeiro CD, Davis P, Jones DM. Citrobacter koseri meningitis in a special care baby unit. J Clin Path. 1976;29:1094–6.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was carried out in accordance with the principles of the Declaration of Helsinki.
Consent for publication
The patient’s guardian consented to publication of the images in this article.
Competing interests
The authors declare no competing interests did not receive support for the submitted work from any organization.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Okamoto, M., Tsuruno, Y. & Fukuzawa, H. Neonatal necrotizing fasciitis with gas gangrene due to peripherally inserted central catheter-related infection. surg case rep 9, 105 (2023). https://doi.org/10.1186/s40792-023-01690-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-023-01690-z