Abstract
Gulf War Illness (GWI) is characterized by a wide range of symptoms that manifests largely as gastrointestinal symptoms. Among these gastrointestinal symptoms, motility disorders are highly prevalent, presenting as chronic constipation, stomach pain, indigestion, diarrhea, and other conditions that severely impact the quality of life of GWI veterans. However, despite a high prevalence of gastrointestinal impairments among these veterans, most research attention has focused on neurological disturbances. This perspective provides a comprehensive overview of current in vivo research advancements elucidating the underlying mechanisms contributing to gastrointestinal disorders in GWI. Generally, these in vivo and in vitro models propose that neuroinflammation alters gut motility and drives the gastrointestinal symptoms reported in GWI. Additionally, this perspective highlights the potential and challenges of in vitro bioengineering models, which could be a crucial contributor to understanding and treating the pathology of gastrointestinal related-GWI.
Similar content being viewed by others
Background
From August 1990 to February 1991, the United States dispatched roughly 697,000 military personnel to the Persian Gulf for Operations Desert Shield and Desert Storm [1]. The war, despite its short duration of only 6 months, resulted in a lasting legacy of health issues for numerous soldiers who participated in the conflict. Approximately 25 – 35% of Gulf War combat veterans, in the months and years following the end of the war, began to exhibit a diverse array of symptoms of seemingly unknown origins [2,3,4]. This inexplicable disease was labeled broadly as Gulf War Illness (GWI) in reference to the shared experiences of Gulf War veterans afflicted by the disease. The increased complexity of GWI stems from various incursions into multiple body systems, including the central nervous system (CNS), the digestive, muscular, and respiratory systems, and largely the immune system, exacerbating physiological and psychological complications [4]. GWI is a multisymptomatic disorder encompassing fatigue, fibromyalgia, functional gastrointestinal disorders (FGIDs), neurological and psychological problems, sleep disturbances, and skin rashes [2, 5, 6]. Notably, FGIDs include symptoms of diarrhea, constipation, nausea, and irritable bowel disease (IBS) reported by GWI veterans [5, 7,8,9]. Neuroinflammation has been shown to be central to most of the reported symptoms [10,11,12,13,14,15] across multiple organ systems. Therefore, the gastrointestinal (GI) system and its connection to neuroinflammation via the enteric nervous system may play a pivotal role in GWI [15,16,17]. Gaining a comprehensive understanding of how neuroinflammation affects the GI tract and developing treatments that specifically target local enteric neuroinflammation could potentially lead to a significant breakthrough in effectively managing and treating GWI for our aging veterans.
GWI affects many biological systems of the body, but there is even greater complexity within the GI-related symptoms. The GI tract is comprised of multiple layers of control (including the central and peripheral nervous system, enteric nervous system, muscular system, and immune components) that work together to maintain physiological function. In GWI, GI dysfunction impacts these systems and leads to long-lasting effects on GI motility while driving enteric neuroinflammation [15, 16], even decades after the initial toxic exposure has been removed. Due to the intricate nature of both GI motility and GWI, there is currently no universally effective treatment available for all symptomatic manifestations. Treatments for general GI disorders encompass dietary and lifestyle modifications, probiotic supplementation, and fecal microbiota transplants. Despite these advancements, the exploration of treatment interventions specifically targeting gut health in veterans with GWI remains limited [18]. This review first explores potential GWI exposures, with an emphasis on prevalent GI symptoms in Gulf War veterans, and critically evaluates the effectiveness and limitations of existing therapeutic interventions aimed at alleviating specific GI symptoms. We provide a brief overview of the disparate systems within the GI tract that contribute to its essential function of GI motility, central to many symptomatic manifestations of GI dysfunction in GWI.
Much of the lagging therapeutic discovery in GI dysfunction related to GWI can be attributed to a limited understanding and lack of GI-specific model systems that provide deep cellular-level insights into multi-cellular physiology leading to GI motility or dysmotility. Bioengineering approaches aim to develop innovative models capable of conveying more accurate information about the cellular microenvironment. Bioengineering is a multidisciplinary field that combines principles and techniques from engineering, medicine, and biomedical sciences (such as cell and molecular biology, physiology, etc.). It focuses on solving intricate problems and developing innovative solutions to deepen our understanding of biological systems. Typical bioengineering strategies involve the combination of cells with biomaterials to create physiological functional tissue-engineered three-dimensional structures in vitro [19,20,21,22,23,24,25,26]. Nuances of GI bioengineering techniques including cell sources and scaffold compositions are reviewed comprehensively elsewhere [27]. Such in vitro bioengineering approaches enhance our understanding of cellular function in physiology and pathophysiology, complementing valuable insights gained from animal models and human clinical trials.
The goal of this review is to highlight in vivo models of GI dysfunction in GWI, as well as the emerging field of bioengineering within the GI domain. We conclude with thought-provoking future perspectives, challenges, and opportunities for bioengineered approaches specifically focused on studying GI dysfunction in GWI, with the hopes of moving therapeutics forward in GWI-related GI dysfunction.
Toxic exposures and the origin of GWI
Gulf War personnel were exposed to a wide range of chemicals, including but not limited to 5 major classes of pesticides such as organophosphates, carbamates, N,N-Diethyl-3-methylbenzamide (DEET), and pyrethroids (permethrin). Other potential toxic exposures include sarin gas, depleted uranium, and emissions from oil well fires; however, their contribution to GWI is less known [4]. The US military provided personal use pesticides like DEET, commonly applied topically, and permethrin, sprayed onto uniforms, to combat arthropod-borne infectious diseases. However, documentation of individual exposure was relatively inconsistent [4, 9]. Organophosphates were another subset of pesticides that were used as sprays, powders, foggers, pest strips, and fly baits [28]. Another Gulf War-related exposure involved pyridostigmine bromide administered orally as a pre-treatment for nerve agents, particularly sarin gas. These exposures have been implicated as a major causation for GWI [29,30,31]. Studies have shown that combined exposure to DEET and/or permethrin with pyridostigmine bromide is known to exhibit synergistic effects even at low doses [32, 33]. Individually, these chemicals demonstrably infiltrate the CNS and peripheral nerves [17]. Organophosphates and pyridostigmine bromide also act as acetylcholinesterase (AChE) enzyme inhibitors, which terminates the action of the neurotransmitter, acetylcholine (ACh) [34]. It has been well reported that AChE enzyme inhibitors are associated with neuroinflammation of the CNS, consequently leading to classic signs such as diarrhea, constipation, muscle weakness, and abdominal pain classified under gut motility dysfunction and FGIDs [35,36,37,38,39,40,41,42,43,44]. Acute toxic exposure to AChE enzyme inhibitors has a predictable systemic effect that depends on the hyperactivity of cholinergic nerve receptors. While chronic effects of AChE enzyme inhibitors have also been linked to negatively impact memory, attention, and long-term brain function within rat models, indicating their potential to inflict neurobehavioral dysfunction [45, 46]. However, the absence of acute toxicity resulting from AChE enzyme inhibition has suggested that GWI is related to an underlying chronic neuroinflammatory disorder rather than an acute response to the direct inhibition of AChE enzyme-receptors [47]. Regardless, the main symptoms arising from impaired central and peripheral cholinergic function due to AChE enzyme inhibition are similar to those reported by afflicted Gulf War veterans, such as fatigue, musculoskeletal, cognitive, GI, and sleep problems [48, 49].
GI dysfunction in the GWI clinic
Soon after the Gulf War, deployed veterans began experiencing chronic and unexplained conditions, as well as symptom clusters that defied conventional medical and psychiatric explanations, including standard laboratory tests. One of the challenges faced by clinicians during the post-Gulf War era was establishing criteria to diagnose Gulf War veterans due to these self-reported symptoms not representing any unique pattern of illness. Over time, there was an evolution in clinical definitions aimed at characterizing these predominantly unexplained symptoms, eventually referred to as GWI among Gulf War veterans. These clinical definitions include chronic multi-symptom illness (CMI) [8], the Kansas GWI definition [50], the Haley syndrome criteria [51, 52], and adaptations of these approaches. Most studies use the Kansas definition which encompasses symptoms falling into 3 out of 6 categories: fatigue and sleep problems, pain, neurologic and mood disorders, GI issues, respiratory problems, and skin symptoms categories [50].
GI complications are notably widespread and often co-occur with various other symptoms exhibited by veterans [53]. Intriguingly, while GI ailments are prevalent among veterans across different conflicts, they appear to be more frequent among Gulf War veterans and persist even after the cessation of war [54]. Findings from various cohort studies suggest that between 14 – 25% of Gulf War veterans report experiencing GI disturbances such as diarrhea, dyspepsia, abdominal pain and discomfort, constipation, nausea, IBS, and other functional GI disorders that originated during their deployment in the Gulf region and persisted upon return to the United States [8, 55,56,57,58,59].
The GI tract is a remarkable example of physiological complexity, encompassing many interactions and systems that are essential for proper functioning. Understanding the complexities of GI disorders has the potential to significantly advance the development of effective therapeutic approaches. In the subsequent sections, we provide an overview of the physiological mechanisms governing GI function in motility and their relevance to understanding GI disorders within GWI.
GI neuroimmune crosstalk in motility in homeostasis and GWI
Physiology at homeostasis
Normal intestinal function relies on the mechanics of GI motility to enable proper digestion, nutrient absorption or excretion, and water absorption [60]. Disruptions in intestinal motility can manifest as significant GI disorders including chronic constipation and diarrhea [61]. The intricacies of GI motility have been comprehensively reviewed by various experts in the field, and the interested reader is encouraged to refer to these reviews for a more profound understanding of GI physiology [62,63,64,65,66]. The gut-brain axis has also grown interested in its involvement in GWI reviewed by Slevin et al. [67], but in this review, we aim to introduce key cellular players and their roles in integrating neuro-immune communication that contributes to GI motility, highlighting how they are disconnected in GWI.
Smooth muscle
Motility in the GI tract is achieved through peristalsis, a mechanism characterized by waves of contractions that propel food or waste forward. This crucial function involves the coordinated shortening of the longitudinal smooth muscle cells and relaxation of the circular smooth muscle cells, resulting in intestinal expansion [68]. These intestinal smooth muscle cells respond to rhythmic impulses from motor neurons within the enteric nervous system (ENS), which is located within the GI tract itself. Ultimately, the smooth muscle layers in the gut play a pivotal role in facilitating motility, mixing, and propelling intraluminal contents, thereby enabling efficient digestion of food, progressive absorption of nutrients, and eventual evacuation of waste [69].
ENS
The ENS is an intricate network that regulates motor function, mucosal permeability, immune function, and endocrine secretion [70]. This interconnected web of sensory, motor, and interneurons heavily relies on cholinergic stimulus primarily utilizing the neurotransmitter ACh.
Motor nerves within the gut innervate both the circular and longitudinal smooth muscle layers (muscularis externa) and are responsible for stimulating smooth muscle force production through neurotransmitters. The main subtypes of motor nerves directly involved in gut motility are excitatory and inhibitory motor nerves, which depend on neurotransmitters such as ACh, vasoactive intestinal peptide, nitric oxide, and substance P. These motor nerves are predominantly located within the myenteric plexus, a network of nerves and glia situated between the smooth muscle layers in the muscularis externa.
Complex regulatory signal processing occurs both independently as well as in coordination with the CNS via the gut-brain axis to maintain homeostasis in the gut and other bodily systems. Disruptions to this neurological regulation have detrimental effects on gut health [71]. Abnormal functioning of excitatory and inhibitory motor nerves has been implicated in GI motility dysfunction observed in animal models [72, 73].
Muscularis macrophages within the gut
Another aspect of the ENS is its ability to interact with the local immune system bidirectionally, maintaining homeostasis or contributing to pathological progression during infection and inflammation [74, 75]. From a perspective of gut motility, muscularis macrophages located within the smooth muscle layers and myenteric plexus of the gut, provide bidirectional support for the survival and differentiation of enteric motor nerves (Fig. 1). Enteric neurons closely interact with muscularis macrophages and produce colony stimulating factor-1 (CSF-1), which in turn promotes their survival. Similarly, muscularis macrophages support neuronal function through the secretion of bone morphogenetic protein 2 (BMP2), thereby ensuring proper neuronal function and gut motility under normal conditions [76]. Muscularis macrophages exhibit a fascinating response to ACh released from stimulated enteric neurons via the vagus nerve, leading to a reduction in the production of pro-inflammatory cytokines [77]. Furthermore, these macrophages play a role in maintaining ENS balance by engulfing apoptotic neurons, and supporting the turnover of neurons [78].
Muscularis macrophages interact with enteric neurons to maintain homeostasis within the gut. ① Muscularis macrophages become activated and release pro-inflammatory cytokines in response to inflammatory triggers ultimately leading to a loss of control of motility. ② The vagus nerve can stimulate enteric neurons and trigger an increased release of ACh. ③ This increase in ACh causes activated muscularis macrophages to return to a state of homeostasis where they offer bidirectional support and communicate directly with enteric neurons. ④ Muscularis macrophages even participate in the phagocytosis of surrounding apoptotic neurons. Ultimately with a balanced support of muscularis macrophages and enteric neurons, this improves the control of motility
GI dysmotility and associated pathophysiology in GWI
During the onset of symptoms associated with GWI within the gut, particularly involving motility dysfunction through functional GI disorders, there can be a synergetic effect on the cellular mechanisms responsible for coordinating gut movement. Research has shown that exposure to agents related to Gulf War activities plays a role in activating macrophages and causing neurodegeneration of the ENS [15,16,17].
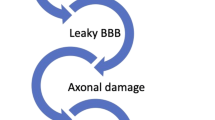
The Gulf War agents primarily belong to a class of AChE enzyme inhibitors, which function by inhibiting the breakdown of the neurotransmitter–ACh. This inhibition leads to an accumulation of ACh near cholinergic receptors. Acute toxic exposures result in decreased responsiveness to ACh due to cholinergic receptor desensitization seen in both muscarinic ACh receptors [79,80,81] and nicotinic ACh receptors [82,83,84], a phenomenon widely observed in nerves within the CNS [85,86,87,88,89]. Systemically, ACh plays a vital role in dampening inflammation by suppressing pro-inflammatory markers and regulating immune cell activity [90, 91]. Conditions such as chronic inflammation or neurodegenerative diseases exhibit decreased ACh activity [92], altering immune modulation and disrupting the balance between pro-inflammatory and anti-inflammatory processes in the gut [93, 94]. Similar neuroinflammatory phenomena are noted secondary to exposure to Gulf War agents within the ENS [12, 16, 17]. When neuroinflammation extends to both nervous and immune components of the enteric nervous system, it results in enteric neuroinflammation that affects the coordination of gut motility at all levels discussed in Sect. "Physiology at homeostasis" involving various cellular players [15,16,17]. Figure 2 illustrates the mechanism through which inflammation is caused by the inhibition of AChE. While this review primarily focuses on the pathophysiology of the cellular components responsible for GI motility, namely smooth muscle cells, enteric motor nerves, and muscularis macrophages, it is crucial to acknowledge the significant implications of the gut microbiome on overall GI tract health and function through its interaction with the gut-immune axis. The gut microbiota plays a pivotal role in regulating the neuro-immune axis by influencing GI barrier function, immunity, and host protection [95], which ultimately impacts gut motility. In inflammatory bowel diseases and other inflammatory conditions affecting the gut, dysbiosis in the gut microbiome impairs colonic motility and transit [96, 97], resulting in a reduction of microbial genes by 25% compared to healthy individuals [98]. Even in the context of GWI, veterans experiencing GI symptoms had an altered microbiome compared to those without GI manifestations [99]. Therefore, considering disruptions in gut motility necessitates careful consideration of alterations in the gut microbiome.
A summary of the effects of AChE inhibition on neuroimmune interactions. Once ingesting pyridostigmine bromide (PB), this incites an inhibition of ACh breakdown leading to a buildup of ACh. Tissue-resident muscularis macrophages become activated and trigger an inflammatory response leading to the release of pro-inflammatory cytokines. This inflammation present near enteric neurons can be classified as enteric neuroinflammation and leads to gut motility dysfunction, present in GWI. AChE acetylcholinesterase, ACh acetylcholine, GWI Gulf War Illness
A comprehensive investigation into the physiology/pathology of GI disorders in GWI lays the foundation for targeted therapeutic interventions. Understanding the intricacies of GI manifestations in GWI, including alterations in gut microbiota, inflammatory responses, gut motility dysfunction, and dysregulated neural signaling, is crucial for developing effective treatment strategies. Defined comprehensions of these manifestations are necessary to facilitate targeted and efficacious therapeutic interventions. Therefore, bridging the gap between the understanding of GWI-GI pathophysiology and conducting therapeutic intervention studies can improve the management of GI-related symptoms and enhance the overall quality of life for Gulf War veterans. This next section explores current therapeutic interventions and their challenges in treating GI-related symptoms among Gulf War veterans.
GI-related therapeutic intervention studies in GWI
GWI-related clinical trials have aimed to investigate the effectiveness of existing interventions in treating similar symptomatic manifestations in other conditions. A wide array of interventions including probiotics, supplements, cognitive behavioral therapy, exercise, medications, and anti-inflammatory drugs have been utilized to improve the overall quality of life for Gulf War veterans. Psychological and exercise interventions, including cognitive behavioral therapy and mindfulness techniques, focus on alleviating GWI symptoms such as pain, fatigue, and cognitive deficits without addressing underlying causes [100,101,102,103,104]. These methods provide moderate relief across various symptom domains. In contrast, medications like doxycycline [105], mifepristone [106, 107], and naltrexone [108] showed limited effectiveness while potentially causing adverse effects or showing no significant improvement. Nutritional interventions like Coenzyme Q10 [109, 110] yield mixed results, whereas ongoing studies explore brain stimulation [111,112,113,114,115], and botanical compounds [116,117,118,119] for managing GWI symptoms, encompassing cognitive deficits, chronic fatigue, and GI issues.
Although these interventions strive to improve the overall quality of life for Gulf War veterans, they fall short in addressing the specific targeting of GI symptoms associated with GWI. This presents a significant challenge in managing this aspect of the condition. The complex nature of these symptoms, including diarrhea, constipation, abdominal pain, and IBS, necessitates targeted interventions tailored to meet the unique needs of Gulf War veterans. Developing effective interventions for these symptoms remains a crucial yet unmet requirement in the comprehensive management of GWI.
Currently, there is a limited number of clinical interventions available for alleviating GI symptoms in Gulf War veterans. One study assessed the effects of Rifaximin, an antibiotic, on a subpopulation of Gulf War veterans diagnosed with IBS, aiming to restore gut microflora. However, this intervention did not demonstrate any in relieving symptoms such as abdominal pain, bloating, stool urgency/frequency/consistency [120]. Another study investigated carnosine, an endogenous antioxidant believed to aid in the elimination of prolonged reactive oxygen species (ROS). Baraniuk et al. [121] found some improvements in GI symptoms including diarrhea. Probiotics have also been examined as a treatment option for GI symptoms. Studies utilized Visbiome, which contains 8 strains of bacteria and has shown efficacy in improving ulcerative colitis [122, 123], however significant results were not observed when it came to alleviating IBS symptoms in comparison to control groups [124]. Dietary interventions involving low-FODMAP (Fermentable Oligo-, Di-, Mono-saccharides, and Polyols) diets for IBS management among Gulf War veterans have been explored; however, no published results are currently available [125]. Nevertheless, other studies using a low-FODMAP diet have demonstrated improvements in alleviating abdominal pain, bloating, and diarrhea [126]. While there are positive outcomes associated with low-FODMAP diets, there are concerns regarding the long-term impact on intestinal microbiome composition, metabolism, and nutritional status. A recent study has commenced investigating the effect of butyrate, a short-chain fatty acid, on alleviating GI symptoms (such as diarrhea, pain, and constipation) through modulation of the gut microbiome and anti-inflammatory effects. Although still in its early stages, this research is anticipated to yield similar benefits in managing GI symptoms to those seen in previous studies on IBS [127].
These clinical interventions offer a significant advantage by directly engaging with the study population to improve patient care. However, they pose unique challenges due to the intricate nature of gut physiology and the multifactorial etiology of GI disorders, particularly in GWI. There is an evident disparity between GWI research and clinical trials as most studies focus on overall patient health, while only a fraction specifically addresses issues related to the GI tract. Emphasizing the importance of the GI tract in GWI is crucial for several reasons. Firstly, the GI tract serves as an important link between the external and internal environments. It plays a significant part in nutrient absorption, waste secretion, immune responses, and microbial balance, making it a key determinant of overall patient health and well-being. Furthermore, neglecting the GI tract may result in incomplete assessments of the illness, delaying the development of effective treatment approaches.
To address these challenges, researchers are increasingly turning to complementary approaches, including animal models and bioengineering techniques for both the discovery of therapeutic avenues and gaining better insights into pathophysiology. Animal models serve as invaluable tools for investigating disease pathogenesis, testing hypotheses, and evaluating therapeutic interventions within in vivo systems. Concurrently, bioengineering models provide controlled microenvironments to simulate complex physiological conditions ex vivo, facilitating targeted studies on specific aspects of GI function and therapeutic responses. Combining bioengineering models and animal studies with clinical trials can address the limitations intrinsic to human-based investigations, offering comprehensive and multi-faceted approaches to enhance our understanding of GWI-GI disorders and improve clinical outcomes. The following sections explore advancements in animal models and bioengineering in elucidating the complexities of GI physiology and pathology of GWI.
In vivo models of GI dysfunction in GWI
The assessment of the role of exposure factors in the development of GWI is challenging due to the limited availability of robust data regarding the precise dosages, frequencies, and durations of these exposures during combat. Furthermore, the complexity arises from the presence of multiple toxicants and unknown interactions between them in the war theater. Additionally, uncertainties remain regarding the effects of repeated exposures to the same toxicant under stressors associated with war and deployment.
The early comprehension of the multifactorial origins of GWI has been largely shaped by preclinical research, with rodent models playing a pivotal role. These models have been used to investigate mechanisms underlying GWI symptoms afflicting various bodily systems such as the brain, gut, muscles, and blood. Initial studies on toxic exposures leading to neuroinflammation in the CNS were instrumental in establishing routes and modes for studying GI dysfunction.
Recently, there has been an increased focus on the GI symptoms related to GWI (Table 1) [15,16,17, 128]. Although relatively new, a modified animal model has emerged that specifically targets the CNS and exposes 5-week-old male and female mice to oral pyridostigmine bromide (PB) for 7 d. This 7-day exposure led to acute alterations in colonic motility and structure in both male and female mice. These were followed by increases in enteric neuroinflammation, glial reactivity, and dysfunctional anatomy of the colon in a sex-dependent manner [16, 17]. Additionally, this study successfully identified key differences between male and female mice upon PB exposure. For example, while both sexes experienced alterations in colonic motility, males exhibited a greater increase whereas females initially displayed lower levels which then progressed into higher levels of colonic motility at day 7. Identifying sex-dependent differences related to GI symptoms can significantly contribute to the development of more effective and personalized treatments. These variations in GI symptoms may potentially arise from hormonal influences, genetic predispositions, or underlying physiological conditions [129]. Age also plays a significant role in gut health due to its substantial effects on immunity, gut motility, and microbial composition [130].
A study done by Gwini et al. [131], suggested that there is a need to consider the relationship between persistently increasing symptoms and long-term morbidity, particularly in aging veterans. Our research group has addressed this concern by subjecting 32- to 34-week-old male mice to PB for a duration of 7 d, evaluating the effect of PB exposure on the repair aspect of the colon of older mice [15]. The results revealed an increase in enteric neuroinflammation, reduced colonic motility, decreased population of enteric neuronal stem cells (ENSCs), and smooth muscle hypertrophy. ENSCs play a crucial role within the GI in maintaining and repairing normal functionality of mature neurons [132]. These findings highlight how PB exposure can exacerbate symptoms as patients get older and emphasize the diminished repair function of ENSCs as a contributing factor to the enduring effects of GWI after initial exposure. Another study has examined obesity as another contributing factor to the exacerbation of GI-related symptoms in GWI. Furthermore, this study examined how a Western-style diet can potentially aggravate GI-related GWI symptoms, considering the potential changes in patients’ diet and lifestyle as they age. Results indicated an elevated presence of persistent GI and neuronal inflammation within obese phenotype in individuals with GWI [128].
The complexity of the human GI system cannot fully be replicated by mouse models. Rudimentary differences between the human and mouse gut anatomy, microbial composition, and physiological responses lead to variations in the development of GWI symptoms [129]. Therefore, while rodent models have been crucial in understanding the complex mechanisms associated with the pathophysiology of diseases, caution must be practiced when applying these results to the etiology of human GWI. An emerging trend in mouse models involves humanizing mice with functional human immune systems through engraftment of human cells. Studies have successfully transplanted human gut microbiota and epithelial cells into mice to recreate aspects of human GI physiology and pathology within an animal model [133]. For instance, humanized mice have been instrumental in studying the role of gut microbiota in the development of diarrhea and constipation, allowing researchers to investigate the underlying mechanisms and identify potential therapeutic targets [134, 135]. Moreover, humanized mouse models can be used to test the efficacy of novel interventions, including probiotics, prebiotics, and dietary supplements, in alleviating GI symptoms [136,137,138]. In the context of GWI-GI, future studies could include incorporating humanized mice to assess immune alterations within the GI tract. Furthermore, elevated cytokines found in Gulf War clinical studies like tumor necrosis factor (TNF) [99] could be added to monitor symptom progression, evaluate treatment efficacy, and elucidate underlying mechanisms, ultimately enhancing relevance and translational potential in GWI-GI disorder research.
Ultimately, GWI has been shown to impact the normal functionality of the gut in both young and older animal models; however, there remains a dearth of research on numerous contributing factors that can exacerbate symptoms, thereby leading to significant concern regarding the treatment of aging patients and identification of specific biomarkers for GI symptoms to facilitate more clinical trials/interventions. In addition to age increase, animal models have reached limits of how in-depth researchers can understand sub-cellular mechanics. In the next section, we will explore how in vitro research can be used to dive deeper into the cellular interactions within the pathophysiology of GWI.
The potential of bioengineered models with GI focus for GWI
The field of in vitro models has undergone significant advancements over the years, enabling the study of a diverse range of diseases, including GI pathology. However, when it comes to GWI, there is a scarcity of in vitro studies specifically focused on GI symptoms. In this section, we will examine the existing in vitro models that concentrate on GWI and provide perspective on future ideas for in vitro models in the GWI-GI context.
Several in vitro models have focused on identifying neurotoxicity caused by Gulf War agents within CNS neurons of humans and rats [139,140,141,142,143]. While these studies have revealed associations between inflammation, increased apoptosis, and persistent neurodegeneration, shedding light on direct and indirect priming effects resulting from exposure to GW agents on specific cell types; they do not directly explore enteric nerves and their effect on GI motility and physiology.
Our research group has successfully isolated various cell types including colonic smooth muscle cells (cSMCs), ENSCs, and bone marrow-derived macrophages from mouse models with GWI. We conducted a study to investigate the effects of acute exposure to pyridostigmine bromide on these cell types after 7 d. Specifically, we explored how pyridostigmine bromide exposure affects the proliferation and characteristics of ENSCs. Our findings revealed that the ENSCs exhibited reduced proliferation rates and lower levels of stem cell markers (Sox2, Sox9, Ngfr) [15]. Additionally, hypertrophy was observed in the musculature of the colon. Notably, our group was the first to demonstrate that exposure to pyridostigmine bromide alters enteric neural stem cell proliferation and induces phenotypic changes in colonic smooth muscle cells [15].
The complexity of GWI, which involves a wide range of GI symptoms and cellular interactions, necessitates the use of more sophisticated in vitro models to evaluate functional outcomes resulting from cell–cell interactions. In related chronic inflammatory diseases with GI symptoms [144,145,146], various in vitro models such as co-culture organoids systems, gut-on-a-chips, and bioengineered tissues have been employed to investigate cellular interactions.
Organoid models
Organoids, also known as 3D cell clusters, have gained popularity due to their ability to mimic physiological properties and facilitate disease modeling [147]. Specifically, GI organoids have been successfully generated from adult human intestinal stem cells and pluripotent stem cells, forming tissue-like structures with multiple layers including the intestinal epithelium, mesenchymal and intestinal stem cells, enterocytes, and secretory cells [148]. With this approach, stem cells are embedded in extracellular matrix (ECM)-rich hydrogels such as Matrigel [149, 150]. The culture medium containing growth factors is critical for GI organoid expansion and may vary slightly between murine and human organoids, but generally include molecules like Wnt/R-spondin, Bone morphogenetic protein (BMP)/Noggin, and Epidermal growth factor (EGF). Moreover, GI organoids can be tailored towards distinct sections of the gut such as the small intestine [151, 152] or colon [153,154,155]. Additionally, these organoids have evolved to incorporate co-cultures with immune cells. For example, Kakni et al. [156] developed a microwell-based coculture system of intestinal organoids and RAW264.7 macrophages supplemented with 2% Matrigel. Upon treatment with TNF-α in these co-cultures of organoids and immune cells, cytokine secretion profiles associated with inflammatory responses [including interleukins, Regulated on Activation, Normal T Expressed and Secreted (RANTES), and interferon- γ (IFN-γ)] were observed resembling aspects of acute and chronic inflammation. Biton et al. [157], on the other hand, found that co-culturing intestinal organoids with polarized T helper cells or IL-17 increased differentiation of Lgr5+ ISCs into goblet cells, Paneth cells, and enteroendocrine cells. Other co-culture systems have investigated the impact of IL-22, IL-2, and IL-13 on the proliferation and differentiation of intestinal organoids, demonstrating that immune cell-derived cytokines and the microbiome can influence the differentiation of intestinal epithelial cells [157,158,159,160,161]. Additionally, these co-culture studies have been utilized to model host–pathogen interactions in response to bacteria [162, 163], viruses [164], and parasites [165]. Although modeling epithelial layers of the gut has been relatively straightforward using the organoid approach, comprehensive investigations often neglect to evaluate GI motility with these approaches. Nevertheless, patient-derived co-culture organoid models remain valuable for studying inflammatory responses in pathogenic conditions by incorporating GW toxic exposures, as well as relevant biomarkers associated with GWI. Remarkably, functional ENS components have been incorporated into organoids featuring a diverse population of neurons capable of inducing smooth muscle contractions through low voltage stimulation [166]. Additionally, Park et al. [167] successfully generated colonic organoids from human embryonic stem cells that contained enteric neural crest stem cells along with mature nerves and blood vessels. Functional enteric nerves and smooth muscle can also be incorporated into GI organoids using cells derived from the three primary germ layers (enteric neuroglial, mesenchymal, and epithelial precursors) stemmed from human pluripotent stem cells [168]. Eicher et al. [168] developed a 3-germ-layer human gastric organoid consisting of glandular epithelium surrounded by functional smooth muscle innervated by enteric neurons capable of regulating contractions. These advancements in intestinal organoids, which possess an intact enteric neuroimmune function, can be tailored to specific GI organs and a variety of diseases, including in the pathogenesis of GI-related GWI. They provide researchers with the opportunity to investigate functional and morphological changes occurring during human ENS-GWI development and progression, as well as explore neuroimmune interactions.
Gut-on-a-chip
Another emerging bioengineering model for studying complex GI diseases is the gut-on-a-chip system. These models can integrate living human cells with mechanical and biochemical cues to mimic the physiological conditions of the gut [169]. The gut-on-a-chip enables real-time monitoring of cellular responses, including barrier function, immune interactions, and peristalsis-like movements, offering a dynamic and physiologically relevant platform for toxicology, pharmacology, and drug studies [170, 171]. A majority of these microfluidic devices are able to replicate the epithelial layer with mucus production and microbiota, including a vascular component to mimic the absorption and distribution of nutrients [169, 172, 173]. Additionally, these systems have expanded beyond just the epithelial layer; they now encompass ‘muscle-on-a-chip’ models that incorporate skeletal and smooth muscle engineering to achieve functional muscle contraction [174,175,176,177]. By incorporating engineered intestinal smooth muscles on-a-chip, these models can be tailored to study GWI-GI dysfunction and screen for GW toxicants. Furthermore, co-culturing various cell types including immune cells and neurons, could enhance the predictive power of preclinical studies by more accurately mimicking human physiology.
Bioengineered intestines
Altered neural networks have been observed in pre-clinical models of GWI [178], as well as in aging individuals, which is also relevant for Gulf War veterans [179, 180]. Bioengineered intestines have been developed within a collagen gel that exhibits physiologically relevance and functional capability to contractile responses. These bioengineered intestines incorporate smooth muscle, neural progenitor cells, glial cells, and mature differentiated nerves [19, 20, 24,25,26]. Therefore, bioengineered muscle could be utilized as a therapeutic approach specifically targeting GI symptoms related to motility dysfunction. On a more fundamental level, these bioengineered intestine models can be employed to study pathological and physiological cellular interactions predominantly present in the outer layer of the colon (as opposed to organoids). Moreover, in the context of GWI, these models can be exposed to Gulf War toxicants; alternatively, tissues donated from Gulf War veterans can be incorporated into these models for drug screening and disease modeling.
Future directions and challenges for bioengineering within GWI
Bioengineering has the potential to revolutionize crucial aspects of medical research, disease pathophysiology, and drug screening development, thereby advancing clinical trials. The precision afforded by bioengineering in genetic manipulation, high-throughput screening, and personalized medicine enhances the efficiency of drug discovery and development processes. Furthermore, bioengineered platforms can significantly reduce reliance on animal testing, while providing more accurate representations of human biology. These innovations can accelerate the understanding of disease pathology and mechanisms, facilitate the identification of potential drug candidates, and enable the development of tailored treatments. Ultimately, this will enhance the effectiveness and safety of interventions tested in clinical trials.
Human patients exhibit significant variations in diet, lifestyle, and genetic makeup, among other criteria, all of which can be implicated in neurological or GI dysfunction. Animal models are important contributors to understanding human physiology by offering similar biological processes, disease modeling, genetic contributions and manipulations, immunological responses, as well as translational research opportunities. However, animal physiology does not fully replicate human physiology, which limits the capacity to effectively test current experimental treatments such as CRISPR-based editing that are specifically tailored to the human genome, or even to accurately predict human toxicity [181]. Controlling this intrinsic variability could provide more meaningful and significant results in the study of human diseases and evaluation of experimental, genetically derived treatment while also facilitating the investigation of novel solutions posited by ongoing research.
Moreover, the progression of clinical trials often entails extensive timelines, with only a fraction successfully overcoming initial checkpoints. This is where the implementation of bioengineering can enhance early-stage clinical trial advancement through genetic engineering, integration of biomaterials, utilization of biobanks, and a focus on personalized medicine (Fig. 3). For instance, within IBS models, bioengineering offers the exploration of genetic and epigenetic influences through whole genomic sequencing [182, 183], as well as transcriptomics for identifying biomarkers [184]. Epigenomic mechanisms influenced by intricate environmental factors may affect the genome, leading to potential implications for IBS [183]. Understanding the interactions between genetic, epigenetic, environmental, and peripheral factors in IBS provides valuable insights into potential treatment approaches. Such insights could be utilized for the parallel and multifaceted nature of GWI, offering promising avenues for clinical intervention.
Various applications of tissue engineering that can be employed through the use of genetic engineering, basic research, implementation of biomaterials, stem cell therapy for personalized medicine, and biobanks which serve to store clinical, demographic, and genetic data. Ultimately tissue engineering can be tailored to each patient and can offer multiple avenues of personalized therapy
Additionally, biobanks are being utilized to screen for biomarkers and omics but can also use comprehensive lifestyle and health-related information, biological measurements, and even brain imaging data to overcome extreme heterogeneity of phenotypes and allow for extensive data analysis on subpopulations [185]. Noteworthy examples of GWI biobanks include the Boston Biorepository, Recruitment, and Integrative Network (BBRAIN), Gulf War Era Cohort and Biorepository (GWECB), and Gulf War Veterans’ Illnesses Biorepository (GWVIB) [186,187,188,189,190]. Yates et al. [191] established a bank of human induced pluripotent stem cells (hiPSCs) from GWI veterans and unaffected individuals stored in BBRAIN. They further developed cerebral organoid cultures capable of differentiating into various cell types including neurons and glia. Another similar study found altered mitochondrial dynamics, decreased neuronal activity, and possible links between predispositions to GWI in some veterans [192]. The GWECB was specifically designed to investigate genetic and environmental associations with GWI by collecting blood samples from over 1000 Gulf War veterans for its repository [190]. Vahey et al. [193] analyzed single nucleotide polymorphisms (SNPs) near ACHE, BCHE, and PON1 genes using samples from GWECB, revealing associations between PON1 gene variants with pyridostigmine bromide exposure in severe cases of GWI and respiratory symptoms related to GWI. Ultimately, these biorepositories can help to advance research by providing biological samples from Gulf War veterans and future studies can be focused on exploring associations between GI symptoms related to GWI exposure variants.
Bioengineering models could also provide the capacity to study individual systems to assess their response to specific drugs or treatments in isolation, a feat that is currently unachievable in vivo. GWI contains a multitude of variables that simultaneously impact multiple organ systems, rendering it increasingly complex to identify precise interactions. Meanwhile, through bioengineering, it’s possible to control these variables, facilitating the sequential testing of individual factors (Fig. 3).
In this regard, the versatility of bioengineering is highly desirable. It enables the deliberate exclusion of confounding interactions commonly observed in biological subjects, such as the neuroimmune crosstalk in GWI. This facilitates more precise identification of vital receptor stimuli and thus leads to a more effective drug design. Also, the ability to use human-relevant tissues with reduced ethical concerns provides an opportunity to test a wider variety of potential treatments in a more relevant context than murine models can offer. In summary, bioengineering holds immense potential and promises extensive applicability in clinical and academic research, enhancing the utilization of human cells as experimental samples for obtaining more relevant, robust, and time-efficient results.
Bioengineering models, while essential for studying pathogenesis, exhibit limitations that warrant consideration in scientific endeavors. Notably, these models serve as a valuable tool for improving early-stage clinical studies, to evaluate treatment efficiency and possible adverse effects. However, these models cannot substitute phase 3 trials required for final drug approval. Phase 3 trials determine the effectiveness and safety of treatments in large patient populations with diverse genetic and biological factors. Additionally, bioengineering models are unable to fully mimic the intricate interactions and outcomes observed in the real-world environment on a larger scale, leading to disparities between observed behaviors and actual disease progression. The absence of systemic and genetic factors such as immune responses and hormonal regulation further hinders their ability to capture the complete spectrum of pathogenic mechanisms that are seen in sex-dependent differences. While bioengineering models can examine specific components like the immune system or enteric nervous stem within the GI tract, replicating the entire colon incorporating vast cellular interaction options becomes increasingly complex. Additionally, the translation of bioengineering techniques into human patients presents emerging challenges in ethics and policy. Central to these concerns is the notion of informed consent, whereby patients must fully comprehend the experimental nature of the treatment along with its potential risks, benefits, and long-term implications. A comprehensive regulatory plan is also necessary to evaluate any translational and transplantation potential of bioengineered human tissue equivalents, with an emphasis on safeguarding patient safety.
Despite its limitations, the future of bioengineering models in the GI tract holds promise for transformative advancements that can be applied to GWI-GI-related symptoms. Innovations in organoid models, organ-on-a-chip, and bioengineered intestine technologies will enable more physiologically relevant GI models by incorporating features like peristalsis and microbial interactions. The integration of microbiome and neuroimmune dynamics, personalized medicine approaches, and advanced biomaterials could enhance the anatomical accuracy and functionality of GI models. Additionally, the prospect of functional GI tissue engineering and multi-organ models signifies potential breakthroughs in therapeutic interventions and systemic understanding. Collectively, these bioengineering approaches aim to play a pivotal role in advancing research on drug development and assessment, disease modeling, as well as personalized treatments for GI disorders reported in GWI.
Through the application of techniques such as genetic engineering, biomaterials, biobanks, and personalized medicine, the integration of tissue engineering in GWI clinical trials could be a critical step forward in addressing this complex condition with multiple symptoms, offering valuable insights that may extend to similar conditions as well. Furthermore, bioengineering can be employed alongside animal models, which provide a controlled environment for studying disease pathways and evaluating potential therapies before progressing to clinical trials. On the other hand, clinical trials provide invaluable data about the safety and efficiency of the treatment in human populations. However, traditional models have limitations, including time expenditure, ethical and regulatory considerations, and patient availability. Tissue engineering techniques possess unique capabilities to bridge these gaps by creating in vitro models that mimic human or human-equivalent tissue structures and functions. This enables researchers to tailor treatments according to individual needs and predict patient responses more accurately while informing future study designs involving animals and humans.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- ACh:
-
Acetylcholine
- AChE:
-
Acetylcholinesterase
- BBRAIN:
-
Boston Biorepository, Recruitment and Integrative Network
- BCHE:
-
Butyrylcholinesterase
- BMP2:
-
Bone morphogenetic protein 2
- CMI:
-
Chronic multisymptom illness
- CNS:
-
Central nervous system
- CRISPR:
-
Clustered Regularly Interspaced Short Palindromic Repeats
- CSF-1:
-
Colony stimulating factor-1
- cSMCs:
-
Colonic smooth muscle cells
- DEET:
-
N,N-Diethyl-3-methylbenzamide
- ECM:
-
Extracellular matrix
- ENS:
-
Enteric nervous system
- ENSCs:
-
Enteric neural stem cells
- FGIDs:
-
Functional gastrointestinal disorders
- FODMAP:
-
Fermentable Oligo-, Di-, Mono-saccharides and Polyols
- GI:
-
Gastrointestinal
- GW:
-
Gulf War
- GWECB:
-
Gulf War Era Cohort and Biorepository
- GWI:
-
Gulf War Illness
- hiPSCs:
-
Human induced pluripotent stem cells
- IBS:
-
Irritable bowel syndrome
- IL:
-
Interleukin
- ISCs:
-
Intestinal stem cells
- MMs:
-
Muscularis macrophages
- Ngfr:
-
Nerve growth factor receptor
- PB:
-
Pyridostigmine bromide
- PON1:
-
Paraoxonase 1
- ROS:
-
Reactive oxygen species
- Sox2:
-
Sex determining region Y-box 2
- Sox9:
-
SRY-related HMG box gene 9
- SNPs:
-
Single nucleotide polymorphisms
- TNF:
-
Tumor necrosis factor
References
Institute of Medicine (US) Committee on Gulf War and Health. Health Effects of Serving in the Gulf War, Update 2009. Gulf War and Health: Volume 8: Update of Health Effects of Serving in the Gulf War. Washington (DC): National Academies Press (US); 2010.
Kates A, Keating J, Baubie K, Putman-Buehler N, Watson L, Godfrey J, et al. Examining the association between the gastrointestinal microbiota and Gulf War illness: a prospective cohort study. PLoS One. 2022;17(7):e0268479.
Mawson AR, Croft AM. Gulf war illness: unifying hypothesis for a continuing health problem. Int J Environ Res Public Health. 2019;16(1):111.
White RF, Steele L, O’Callaghan JP, Sullivan K, Binns JH, Golomb BA, et al. Recent research on Gulf war illness and other health problems in veterans of the 1991 Gulf War: effects of toxicant exposures during deployment. Cortex. 2016;74:449–75.
Maule AL, Janulewicz PA, Sullivan KA, Krengel MH, Yee MK, McClean M, et al. Meta-analysis of self-reported health symptoms in 1990–1991 Gulf War and Gulf War-era veterans. BMJ Open. 2018;8(2):e016086.
Fappiano CM, Baraniuk JN. Gulf war illness symptom severity and onset: a cross-sectional survey. Mil Med. 2020;185(7–8):e1120–7.
Kimono DA. Gastrointestinal problems, mechanisms and possible therapeutic directions in Gulf war illness: a mini review. Mil Med Res. 2021;8(1):1–8.
Fukuda K, Nisenbaum R, Stewart G, Thompson WW, Robin L, Washko RM, et al. Chronic multisymptom illness affecting Air Force veterans of the Gulf War. JAMA. 1998;280(11):981–8.
Janulewicz P, Krengel M, Quinn E, Heeren T, Toomey R, Killiany R, et al. The multiple hit hypothesis for gulf war illness: self-reported chemical/biological weapons exposure and mild traumatic brain injury. Brain Sci. 2018;8(11):198.
Madhu LN, Attaluri S, Kodali M, Shuai B, Upadhya R, Gitai D, et al. Neuroinflammation in Gulf War Illness is linked with HMGB1 and complement activation, which can be discerned from brain-derived extracellular vesicles in the blood. Brain Behav Immun. 2019;81:430–43.
Alshelh Z, Albrecht DS, Bergan C, Akeju O, Clauw DJ, Conboy L, et al. In vivo imaging of neuroinflammation in veterans with Gulf War illness. Brain Behav Immun. 2020;87:498–507.
Kimono D, Sarkar S, Albadrani M, Seth R, Bose D, Mondal A, et al. Dysbiosis-associated enteric glial cell immune-activation and redox imbalance modulate tight junction protein expression in gulf war illness pathology. Front Physiol. 2019;10:1229.
Macht V, Woodruff J, Grillo C, Wood C, Wilson M, Reagan L. Pathophysiology in a model of Gulf War Illness: contributions of pyridostigmine bromide and stress. Psychoneuroendocrinology. 2018;96:195–202.
Zhou Q, Verne ML, Zhang B, Verne GN. Evidence for somatic hypersensitivity in veterans with gulf war illness and gastrointestinal symptoms. Clin J Pain. 2018;34(10):944–9.
Collier CA, Foncerrada S, Clevenger AJ, Shetty A, Raghavan SA. Acute exposure to pyridostigmine bromide disrupts cholinergic myenteric neuroimmune function in mice. Adv Biol (Weinh). 2023;7(5):e2200254.
Hernandez S, Fried DE, Grubišić V, McClain JL, Gulbransen BD. Gastrointestinal neuroimmune disruption in a mouse model of Gulf War illness. FASEB J. 2019;33(5):6168–84.
Hernandez S, Morales-Soto W, Grubišić V, Fried D, Gulbransen BD. Pyridostigmine bromide exposure creates chronic, underlying neuroimmune disruption in the gastrointestinal tract and brain that alters responses to palmitoylethanolamide in a mouse model of Gulf War Illness. Neuropharmacology. 2020;179:108264.
Seth RK, Kimono D, Alhasson F, Sarkar S, Albadrani M, Lasley SK, et al. Increased butyrate priming in the gut stalls microbiome associated-gastrointestinal inflammation and hepatic metabolic reprogramming in a mouse model of Gulf War Illness. Toxicol Appl Pharmacol. 2018;350:64–77.
Gilmont RR, Raghavan S, Somara S, Bitar KN. Bioengineering of physiologically functional intrinsically innervated human internal anal sphincter constructs. Tissue Eng Part A. 2014;20(11–12):1603–11.
Raghavan S, Lam MT, Foster LL, Gilmont RR, Somara S, Takayama S, et al. Bioengineered three-dimensional physiological model of colonic longitudinal smooth muscle in vitro. Tissue Eng Part C Methods. 2010;16(5):999–1009.
Kitano K, Schwartz DM, Zhou H, Gilpin SE, Wojtkiewicz GR, Ren X, et al. Bioengineering of functional human induced pluripotent stem cell-derived intestinal grafts. Nat Commun. 2017;8(1):765.
Lee M, Wu BM, Stelzner M, Reichardt HM, Dunn JC. Intestinal smooth muscle cell maintenance by basic fibroblast growth factor. Tissue Eng Part A. 2008;14(8):1395–402.
Nakase Y, Hagiwara A, Nakamura T, Kin S, Nakashima S, Yoshikawa T, et al. Tissue engineering of small intestinal tissue using collagen sponge scaffolds seeded with smooth muscle cells. Tissue Eng. 2006;12(2):403–12.
Somara S, Gilmont RR, Dennis RG, Bitar KN. Bioengineered internal anal sphincter derived from isolated human internal anal sphincter smooth muscle cells. Gastroenterology. 2009;137(1):53–61.
Singh J, Rattan S. Bioengineered human IAS reconstructs with functional and molecular properties similar to intact IAS. Am J Physiol Gastrointest Liver Physiol. 2012;303(6):G713–22.
Raghavan S, Miyasaka EA, Gilmont RR, Somara S, Teitelbaum DH, Bitar KN. Perianal implantation of bioengineered human internal anal sphincter constructs intrinsically innervated with human neural progenitor cells. Surgery. 2014;155(4):668–74.
Collier CA, Mendiondo C, Raghavan S. Tissue engineering of the gastrointestinal tract: the historic path to translation. J Biol Eng. 2022;16(1):9.
Sullivan K, Krengel M, Bradford W, Stone C, Thompson TA, Heeren T, et al. Neuropsychological functioning in military pesticide applicators from the Gulf War: effects on information processing speed, attention and visual memory. Neurotoxicol Teratol. 2018;65:1–13.
Charatan F. Nerve gas antidote a possible cause of gulf war illness. BMJ. 1999;319(7218):1154.
Steele L, Lockridge O, Gerkovich MM, Cook MR, Sastre A. Butyrylcholinesterase genotype and enzyme activity in relation to Gulf War illness: preliminary evidence of gene-exposure interaction from a case-control study of 1991 Gulf War veterans. Environ Health. 2015;14(1):4.
Elhaj R, Reynolds JM. Chemical exposures and suspected impact on Gulf War Veterans. Mil Med Res. 2023;10(1):11.
Abou-Donia MB, Wilmarth KR, Jensen KF, Oehme FW, Kurt TL. Neurotoxicity resulting from coexposure to pyridostigmine bromide, deet, and permethrin: implications of Gulf War chemical exposures. J Toxicol Environ Health. 1996;48(1):35–56.
van Haaren F, Haworth SC, Bennett SM, Cody BA, Hoy JB, Karlix JL, et al. The effects of pyridostigmine bromide, permethrin, and DEET alone, or in combination, on fixed-ratio and fixed-interval behavior in male and female rats. Pharmacol Biochem Behav. 2001;69(1–2):23–33.
Gupta RC. CHAPTER 1 - Introduction. In: Gupta RC, editor. Toxicology of Organophosphate & Carbamate Compounds. Burlington: Academic Press; 2006. p. 3–4.
Palanisamy BN, Sarkar S, Malovic E, Samidurai M, Charli A, Zenitsky G, et al. Environmental neurotoxic pesticide exposure induces gut inflammation and enteric neuronal degeneration by impairing enteric glial mitochondrial function in pesticide models of Parkinson’s disease: potential relevance to gut-brain axis inflammation in Parkinson’s disease pathogenesis. Int J Biochem Cell Biol. 2022;147:106225.
Liu Q, Shao W, Zhang C, Xu C, Wang Q, Liu H, et al. Organochloride pesticides modulated gut microbiota and influenced bile acid metabolism in mice. Environ Pollut. 2017;226:268–76.
Halaris A. Neuroinflammation and neurotoxicity contribute to neuroprogression in neurological and psychiatric disorders. Future Neurol. 2018;13(2):59–69.
Zhao Y, Zhang Y, Wang G, Han R, Xie X. Effects of chlorpyrifos on the gut microbiome and urine metabolome in mouse (Mus musculus). Chemosphere. 2016;153:287–93.
Gama J, Neves B, Pereira A. Chronic effects of dietary pesticides on the gut microbiome and neurodevelopment. Front Microbiol. 2022;13:931440.
Ruíz-Arias MA, Medina-Díaz IM, Bernal-Hernández YY, Agraz-Cibrián JM, González-Arias CA, Barrón-Vivanco BS, et al. Hematological indices as indicators of inflammation induced by exposure to pesticides. Environ Sci Pollut Res Int. 2023;30(7):19466–76.
Das UN. Acetylcholinesterase and butyrylcholinesterase as possible markers of low-grade systemic inflammation. Med Sci Monit. 2007;13(12):RA214-21.
Gnatek Y, Zimmerman G, Goll Y, Najami N, Soreq H, Friedman A. Acetylcholinesterase loosens the brain’s cholinergic anti-inflammatory response and promotes epileptogenesis. Front Mol Neurosci. 2012;5:66.
Tyagi E, Agrawal R, Nath C, Shukla R. Influence of LPS-induced neuroinflammation on acetylcholinesterase activity in rat brain. J Neuroimmunol. 2008;205(1–2):51–6.
Li J, Chen Y, Zhang X, Ye S, Yi J, Chen Q, et al. Inhibition of acetylcholinesterase attenuated retinal inflammation via suppressing NF-κB activation. Exp Eye Res. 2020;195:108003.
Abou-Donia MB, Wilmarth KR, Abdel-Rahman AA, Jensen KF, Oehme FW, Kurt TL. Increased neurotoxicity following concurrent exposure to pyridostigmine bromide, DEET, and chlorpyrifos. Fundam Appl Toxicol. 1996;34(2):201–22.
Lange G, Tiersky LA, DeLuca J, Scharer JB, Policastro T, Fiedler N, et al. Cognitive functioning in Gulf War Illness. J Clin Exp Neuropsychol. 2001;23(2):240–9.
Michalovicz LT, Kelly KA, Sullivan K, O’Callaghan JP. Acetylcholinesterase inhibitor exposures as an initiating factor in the development of Gulf War Illness, a chronic neuroimmune disorder in deployed veterans. Neuropharmacology. 2020;171:108073.
Khan F, Kennedy G, Spence VA, Newton DJ, Belch JJ. Peripheral cholinergic function in humans with chronic fatigue syndrome, Gulf War syndrome and with illness following organophosphate exposure. Clin Sci (Lond). 2004;106(2):183–9.
Golomb BA. Acetylcholinesterase inhibitors and Gulf War illnesses. Proc Natl Acad Sci U S A. 2008;105(11):4295–300.
Steele L. Prevalence and patterns of Gulf War illness in Kansas veterans: association of symptoms with characteristics of person, place, and time of military service. Am J Epidemiol. 2000;152(10):992–1002.
Haley RW, Kurt TL, Hom J. Is there a Gulf war syndrome?: searching for syndromes by factor analysis of symptoms. JAMA. 1997;277(3):215–22.
Haley RW, Luk GD, Petty F. Use of structural equation modeling to test the construct validity of a case definition of Gulf War syndrome: invariance over developmental and validation samples, service branches and publicity. Psychiatry Res. 2001;102(2):175–200.
Koch TR, Emory TS. Evaluation of chronic gastrointestinal symptoms following Persian Gulf War exposure. Mil Med. 2005;170(8):696–700.
Dursa EK, Barth SK, Schneiderman AI, Bossarte RM. Physical and mental health status of Gulf war and gulf era veterans: results from a large population-based epidemiological study. J Occup Environ Med. 2016;58(1):41–6.
Hyams KC, Bourgeois AL, Merrell BR, Rozmajzl P, Escamilla J, Thornton SA, et al. Diarrheal disease during Operation Desert Shield. N Engl J Med. 1991;325(20):1423–8.
Proctor S, Heeren T, White R, Wolfe J, Borgos M, Davis J, et al. Health status of Persian Gulf War veterans: self-reported symptoms, environmental exposures and the effect of stress. Int J Epidemiol. 1998;27(6):1000–10.
Murphy FM, Kang H, Dalager NA, Lee KY, Allen RE, Mather SH, et al. The health status of Gulf war veterans: lessons learned from the department of veterans affairs health registry. Mil Med. 1999;164(5):327–31.
Joseph SC. A comprehensive clinical evaluation of 20,000 Persian Gulf War veterans. Comprehensive Clinical Evaluation Program Evaluation Team. Mil Med. 1997;162(3):149–55.
Sostek M, Jackson S, Linevsky J, Schimmel E, Fincke B. High prevalence of chronic gastrointestinal symptoms in a National Guard Unit of Persian Gulf veterans. Am J Gastroenterol. 1996;91(12):2494–7.
Ukleja A. Altered GI motility in critically ill patients: current understanding of pathophysiology, clinical impact, and diagnostic approach. Nutr Clin Pract. 2010;25(1):16–25.
Bassotti G, Antonelli E, Villanacci V, Nascimbeni R, Dore MP, Pes GM, et al. Abnormal gut motility in inflammatory bowel disease: an update. Tech Coloproctol. 2020;24(4):275–82.
De Schepper S, Stakenborg N, Matteoli G, Verheijden S, Boeckxstaens GE. Muscularis macrophages: key players in intestinal homeostasis and disease. Cell Immunol. 2018;330:142–50.
Yoo BB, Mazmanian SK. The enteric network: interactions between the immune and nervous systems of the gut. Immunity. 2017;46(6):910–26.
Sanders KM, Koh SD, Ro S, Ward SM. Regulation of gastrointestinal motility–insights from smooth muscle biology. Nat Rev Gastroenterol Hepatol. 2012;9(11):633–45.
Fleming MA 2nd, Ehsan L, Moore SR, Levin DE. The enteric nervous system and its emerging role as a therapeutic target. Gastroenterol Res Pract. 2020;2020:8024171.
Wang H, Foong JPP, Harris NL, Bornstein JC. Enteric neuroimmune interactions coordinate intestinal responses in health and disease. Mucosal Immunol. 2022;15(1):27–39.
Slevin E, Koyama S, Harrison K, Wan Y, Klaunig JE, Wu C, et al. Dysbiosis in gastrointestinal pathophysiology: role of the gut microbiome in Gulf War Illness. J Cell Mol Med. 2023;27(7):891–905.
Wood JD. Peristalsis. In: Johnson LR, editor. Encyclopedia of Gastroenterology. New York: Elsevier; 2004. p. 164–5.
Bitar KN. Function of gastrointestinal smooth muscle: from signaling to contractile proteins. Am J Med. 2003;115(Suppl 3A):15S-23S.
Goyal RK, Hirano I. The enteric nervous system. N Engl J Med. 1996;334(17):1106–15.
Abdullah N, Defaye M, Altier C. Neural control of gut homeostasis. Am J Physiol Gastrointest Liver Physiol. 2020;319(6):G718–32.
Luckey A, Livingston E, Taché Y. Mechanisms and treatment of postoperative ileus. Arch Surg. 2003;138(2):206–14.
Wood J, Alpers D, Andrews P. Fundamentals of neurogastroenterology. Gut. 1999;45(Suppl 2):II6–16.
Weihe E, Nohr D, Michel S, Müller S, Zentel H, Fink T, et al. Molecular anatomy of the neuro-immune connection. Int J Neurosci. 1991;59(1–3):1–23.
Verheijden S, Boeckxstaens GE. Neuroimmune interaction and the regulation of intestinal immune homeostasis. Am J Physiol Gastrointest Liver Physiol. 2018;314(1):G75-80.
Muller PA, Koscsó B, Rajani GM, Stevanovic K, Berres ML, Hashimoto D, et al. Crosstalk between muscularis macrophages and enteric neurons regulates gastrointestinal motility. Cell. 2014;158(2):300–13.
Matteoli G, Gomez-Pinilla PJ, Nemethova A, Di Giovangiulio M, Cailotto C, van Bree SH, et al. A distinct vagal anti-inflammatory pathway modulates intestinal muscularis resident macrophages independent of the spleen. Gut. 2014;63(6):938–48.
Kulkarni S, Micci MA, Leser J, Shin C, Tang SC, Fu YY, et al. Adult enteric nervous system in health is maintained by a dynamic balance between neuronal apoptosis and neurogenesis. Proc Natl Acad Sci U S A. 2017;114(18):E3709–18.
Ward T, Ferris D, Tilson H, Mundy W. Correlation of the anticholinesterase activity of a series of organophosphates with their ability to compete with agonist binding to muscarinic receptors. Toxicol Appl Pharmacol. 1993;122(2):300–7.
Bakry NM, El-Rashidy AH, Eldefrawi AT, Eldefrawi ME. Direct actions of organophosphate anticholinesterases on nicotinic and muscarinic acetylcholine receptors. J Biochem Toxicol. 1988;3(4):235–59.
Liu J, Chakraborti T, Pope C. In vitro effects of organophosphorus anticholinesterases on muscarinic receptor-mediated inhibition of acetylcholine release in rat striatum. Toxicol Appl Pharmacol. 2002;178(2):102–8.
Katz EJ, Cortes VI, Eldefrawi ME, Eldefrawi AT. Chlorpyrifos, parathion, and their oxons bind to and desensitize a nicotinic acetylcholine receptor: relevance to their toxicities. Toxicol Appl Pharmacol. 1997;146(2):227–36.
Smulders CJGM, Bueters TJH, Vailati S, van Kleef RGDM, Vijverberg HPM. Block of neuronal nicotinic acetylcholine receptors by organophosphate insecticides. Toxicol Sci. 2004;82(2):545–54.
Albuquerque EX, Alkondon M, Pereira EF, Castro NG, Schrattenholz A, Barbosa CT, et al. Properties of neuronal nicotinic acetylcholine receptors: pharmacological characterization and modulation of synaptic function. J Pharmacol Exp Ther. 1997;280(3):1117–36.
Quick MW, Lester RAJ. Desensitization of neuronal nicotinic receptors. J Neurobiol. 2002;53(4):457–78.
Katz B, Thesleff S. A study of the desensitization produced by acetylcholine at the motor end-plate. J Physiol. 1957;138(1):63.
Giniatullin R, Nistri A, Yakel JL. Desensitization of nicotinic ACh receptors: shaping cholinergic signaling. Trends Neurosci. 2005;28(7):371–8.
Abou-Donia MB, Dechkovskaia AM, Goldstein LB, Abdel-Rahman A, Bullman SL, Khan WA. Co-exposure to pyridostigmine bromide, DEET, and/or permethrin causes sensorimotor deficit and alterations in brain acetylcholinesterase activity. Pharmacol Biochem Behav. 2004;77(2):253–62.
Zakirova Z, Tweed M, Crynen G, Reed J, Abdullah L, Nissanka N, et al. Gulf War agent exposure causes impairment of long-term memory formation and neuropathological changes in a mouse model of Gulf War Illness. PLoS One. 2015;10(3):e0119579.
Borovikova LV, Ivanova S, Zhang M, Yang H, Botchkina GI, Watkins LR, et al. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature. 2000;405(6785):458–62.
Tracey KJ. Physiology and immunology of the cholinergic antiinflammatory pathway. J Clin Invest. 2007;117(2):289–96.
Pavlov VA, Tracey KJ. The vagus nerve and the inflammatory reflex-linking immunity and metabolism. Nat Rev Endocrinol. 2012;8(12):743–54.
Wang H, Yu M, Ochani M, Amella CA, Tanovic M, Susarla S, et al. Nicotinic acetylcholine receptor α7 subunit is an essential regulator of inflammation. Nature. 2003;421(6921):384–8.
Saeed RW, Varma S, Peng-Nemeroff T, Sherry B, Balakhaneh D, Huston J, et al. Cholinergic stimulation blocks endothelial cell activation and leukocyte recruitment during inflammation. J Exp Med. 2005;201(7):1113–23.
Sittipo P, Choi J, Lee S, Lee YK. The function of gut microbiota in immune-related neurological disorders: a review. J Neuroinflammation. 2022;19(1):154.
Shukla R, Ghoshal U, Dhole TN, Ghoshal UC. Fecal microbiota in patients with irritable bowel syndrome compared with healthy controls using real-time polymerase chain reaction: an evidence of dysbiosis. Dig Dis Sci. 2015;60:2953–62.
Malinen E, Rinttilä T, Kajander K, Mättö J, Kassinen A, Krogius L, et al. Analysis of the fecal microbiota of irritable bowel syndrome patients and healthy controls with real-time PCR. Am J Gastroenterol. 2005;100(2):373–82.
Bernstein CN, Forbes JD. Gut microbiome in inflammatory bowel disease and other chronic immune-mediated inflammatory diseases. Inflamm Intest Dis. 2017;2(2):116–23.
Janulewicz PA, Seth RK, Carlson JM, Ajama J, Quinn E, Heeren T, et al. The gut-microbiome in Gulf War veterans: a preliminary report. Int J Environ Res Public Health. 2019;16(19):3751.
Donta ST, Clauw DJ, Engel CC Jr, Guarino P, Peduzzi P, Williams DA, et al. Cognitive behavioral therapy and aerobic exercise for Gulf War veterans’ illnesses: a randomized controlled trial. JAMA. 2003;289(11):1396–404.
Kearney DJ, Simpson TL, Malte CA, Felleman B, Martinez ME, Hunt SC. Mindfulness-based stress reduction in addition to usual care is associated with improvements in pain, fatigue, and cognitive failures among veterans with gulf war illness. Am J Med. 2016;129(2):204–14.
Nakamura Y, Lipschitz DL, Donaldson GW, Kida Y, Williams SL, Landward R, et al. Investigating clinical benefits of a novel sleep-focused mind-body program on Gulf War illness symptoms: a randomized controlled trial. Psychosom Med. 2017;79(6):706–18.
Kerr K, Morse G, Graves D, Zuo F, Lipowicz A, Carpenter DO. A detoxification intervention for Gulf War illness: a pilot randomized controlled trial. Int J Environ Res Public Health. 2019;16(21):4143.
Mathersul DC, Eising CM, DeSouza DD, Spiegel D, Bayley PJ. Brain and physiological markers of autonomic function are associated with treatment-related improvements in self-reported autonomic dysfunction in veterans with gulf war illness: an exploratory pilot study. Glob Adv Health Med. 2020;9:2164956120922812.
Donta ST, Engel CC Jr, Collins JF, Baseman JB, Dever LL, Taylor T, et al. Benefits and harms of doxycycline treatment for Gulf War veterans’ illnesses: a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2004;141(2):85–94.
Castinetti F, Conte-Devolx B, Brue T. Medical treatment of Cushing’s syndrome: glucocorticoid receptor antagonists and mifepristone. Neuroendocrinology. 2010;92(Suppl 1):125–30.
Golier JA, Caramanica K, Michaelides AC, Makotkine I, Schmeidler J, Harvey PD, et al. A randomized, double-blind, placebo-controlled, crossover trial of mifepristone in Gulf War veterans with chronic multisymptom illness. Psychoneuroendocrinology. 2016;64:22–30.
Brewer KL, Mainhart A, Meggs WJ. Double-blinded placebo-controlled cross-over pilot trial of naltrexone to treat Gulf War Illness. Fatigue Biomed Health Behav. 2018;6(3):132–40.
Golomb BA, Allison M, Koperski S, Koslik HJ, Devaraj S, Ritchie JB. Coenzyme Q10 benefits symptoms in Gulf War veterans: results of a randomized double-blind study. Neural Comput. 2014;26(11):2594–651.
Fletcher MA, Research SFVFf, States EIMU. Measurement of biomakers in samples collected in a coenzyme Q10 treatment trial in Gulf War Illness and control subjects. 2018. https://apps.dtic.mil/sti/citations/AD1168084.
Hart J, States TUoTaDRU. Treatment of memory disorders in Gulf War Illness with high-definition transcranial direct stimulation. 2019. https://clinicaltrials.gov/study/NCT03542383.
Lei K, Golshan S, DeBruin N, Wong A, Nguyen E, Doan B, et al. Alleviating headaches and pain in Gulf War Illness using neuronavigation-guided rTMS: a preliminary assessment. Brain Stimul. 2018;11(6):e17–8.
Kunnel A, Lei K, Metzger-Smith V, Golshan S, Javors J, Wei J, et al. Neuronavigation guided rTMS in alleviating Gulf War Illness symptoms. Brain Stimul. 2020;13(6):1843–4.
Natelson BH, States ISOMAMSNYU. Vagus nerve stimulation: a non invasive treatment to improve the health of Gulf veterans with Gulf war illness. 2017. https://clinicaltrials.gov/study/NCT02865460?cond=Gulf%20War%20Illness&term=Coenzyme%20Q10&rank=2#publications.
Natelson BH, Stegner AJ, Lange G, Khan S, Blate M, Sotolongo A, et al. Vagal nerve stimulation as a possible non-invasive treatment for chronic widespread pain in Gulf Veterans with Gulf War Illness. Life Sci. 2021;282: 119805.
Younger J, Donovan E, States UoAaBBU. Treating Gulf war illness with novel anti-inflammatories: a screening of botantical microglia modulators. 2016. https://clinicaltrials.gov/study/NCT02909686?term=NCT02909686&rank=1.
Younger J, Donovan EK, Hodgin KS, Ness TJ. A placebo-controlled, pseudo-randomized, crossover trial of botanical agents for Gulf war illness: Reishi mushroom (Ganoderma lucidum), Stinging nettle (Urtica dioica), and Epimedium (Epimedium sagittatum). Int J Environ Res Public Health. 2021;18(7):3671.
Donovan EK, Kekes-Szabo S, Lin JC, Massey RL, Cobb JD, Hodgin KS, et al. A placebo-controlled, pseudo-randomized, crossover trial of botanical agents for Gulf war illness: curcumin (Curcuma longa), Boswellia (Boswellia serrata), and French maritime pine bark (Pinus pinaster). Int J Environ Res Public Health. 2021;18(5):2468.
Hodgin KS, Donovan EK, Kekes-Szabo S, Lin JC, Feick J, Massey RL, et al. A placebo-controlled, pseudo-randomized, crossover trial of botanical agents for gulf war illness: resveratrol (Polygonum cuspidatum), luteolin, and fisetin (Rhus succedanea). Int J Environ Res Public Health. 2021;18(5):2483.
Tuteja AK, Talley NJ, Stoddard GJ, Verne GN. Double-blind placebo-controlled study of rifaximin and lactulose hydrogen breath test in gulf war veterans with irritable bowel syndrome. Dig Dis Sci. 2019;64(3):838–45.
Baraniuk JN, El-Amin S, Corey R, Rayhan RU, Timbol CR. Carnosine treatment for Gulf War Illness: a randomized controlled trial. Glob J Health Sci. 2013;5(3):69–81.
Dang X, Xu M, Liu D, Zhou D, Yang W. Assessing the efficacy and safety of fecal microbiota transplantation and probiotic VSL# 3 for active ulcerative colitis: a systematic review and meta-analysis. PLoS One. 2020;15(3): e0228846.
Ford AC, Quigley EMM, Lacy BE, Lembo AJ, Saito YA, Schiller LR, et al. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. Am J Gastroenterol. 2014;109(10):1547–61.
Tuteja AK, Talley NJ, Murtaugh MA, Loc-Carrillo CM, Stoddard GJ, Anderson GL. Randomized, double-blind placebo-controlled trial to assess the effect of probiotics on irritable bowel syndrome in veterans with Gulf war illness. Fed Pract. 2022;39(10):410–7.
Tuteja A, States WIfBRSLCU. Effect of diet on Gulf war illness: a pilot study. 2016. https://clinicaltrials.gov/study/NCT02881944?lead=Ashok%20Tuteja&rank=2.
Altobelli E, del Negro V, Angeletti PM, Latella G. Low-FODMAP diet improves irritable bowel syndrome symptoms: a meta-analysis. Nutrients. 2017;9(9):940.
Scarpellini E, Lauritano E, Lupascu A, Petruzzellis C, Novi M, Roccarina D, et al. Efficacy of butyrate in the treatment of diarrhoea-predominant irritable bowel syndrome. Dig Liver Dis Sup. 2007;1(1):19–22.
Bose D, Saha P, Mondal A, Fanelli B, Seth RK, Janulewicz P, et al. Obesity worsens Gulf War Illness symptom persistence pathology by linking altered gut microbiome species to long-term gastrointestinal, hepatic, and neuronal inflammation in a mouse model. Nutrients. 2020;12(9):2764.
Narayanan SP, Anderson B, Bharucha AE. Sex- and gender-related differences in common functional gastroenterologic disorders. Mayo Clin Proc. 2021;96(4):1071–89.
Merchant HA, Liu F, Orlu Gul M, Basit AW. Age-mediated changes in the gastrointestinal tract. Int J Pharm. 2016;512(2):382–95.
Gwini SM, Forbes AB, Kelsall HL, Ikin JF, Sim MR. Increased symptom reporting persists in 1990–1991 Gulf War veterans 20 years post deployment. Am J Ind Med. 2015;58(12):1246–54.
Raghavan S, Gilmont RR, Bitar KN. Neuroglial differentiation of adult enteric neuronal progenitor cells as a function of extracellular matrix composition. Biomaterials. 2013;34(28):6649–58.
Kashyap PC, Marcobal A, Ursell LK, Larauche M, Duboc H, Earle KA, et al. Complex interactions among diet, gastrointestinal transit, and gut microbiota in humanized mice. Gastroenterology. 2013;144(5):967–77.
Yu Y, Lu L, Sun J, Petrof EO, Claud EC. Preterm infant gut microbiota affects intestinal epithelial development in a humanized microbiome gnotobiotic mouse model. Am J Physiol Gastrointest Liver Physiol. 2016;311(3):G521–32.
Oozeer R, Furet J, Goupil-Feuillerat N, Anba J, Mengaud J, Corthier G. Differential activities of four Lactobacillus casei promoters during bacterial transit through the gastrointestinal tracts of human-microbiota-associated mice. Appl Environ Microbiol. 2005;71(3):1356–63.
Constante M, de Palma G, Lu J, Jury J, Collins S, Bercik P, et al. A53 Saccharomyces boulardii CNCM I-745 improves anxiety-like behavior and rescues dysmotility in a humanized mouse model of irritable bowel syndrome with co-morbid anxiety. J Can Assoc Gastroenterol. 2020;3(Supplement_1):62–3.
Constante M, de Palma G, Lu J, Jury J, Rondeau L, Caminero A, et al. Saccharomyces boulardii CNCM I-745 modulates the microbiota-gut-brain axis in a humanized mouse model of Irritable Bowel Syndrome. Neurogastroenterol Motil. 2021;33(3):e13985.
Negi S, Saini S, Tandel N, Sahu K, Mishra RP, Tyagi RK. Translating Treg therapy for inflammatory bowel disease in humanized mice. Cells. 2021;10(8):1847.
Qiang L, Rao AN, Mostoslavsky G, James MF, Comfort N, Sullivan K, et al. Reprogramming cells from Gulf War veterans into neurons to study Gulf War Illness. Neurology. 2017;88(20):1968–75.
Georgopoulos AP, Tsilibary EC, Souto EP, James LM, Engdahl BE, Georgopoulos A. Adverse effects of Gulf War Illness (GWI) serum on neural cultures and their prevention by healthy serum. J Neurol Neuromedicine. 2018;3(2):19–27.
Azzolin VF, Barbisan F, Lenz LS, Teixeira CF, Fortuna M, Duarte T, et al. Effects of Pyridostigmine bromide on SH-SY5Y cells: an in vitro neuroblastoma neurotoxicity model. Mutat Res Genet Toxicol Environ Mutagen. 2017;823:1–10.
Li L, Gunasekar PG, Borowitz JL, Isom GE. Muscarinic receptor-mediated pyridostigmine-induced neuronal apoptosis. Neurotoxicology. 2000;21(4):541–52.
Goodyear AA. Direct and indirect effects of Gulf War Illness-related chemicals on microglia activation: in vitro and ex vivo studies: University of Georgia; 2023. https://esploro.libs.uga.edu/esploro/outputs/graduate/DIRECT-AND-INDIRECT-EFFECTS-OF-GULF/9949618028302959?institution=01GALI_UGA.
Donohoe CL, Reynolds JV. Short bowel syndrome. Surgeon. 2010;8(5):270–9.
Park KT, Bass D. Inflammatory bowel disease-attributable costs and cost-effective strategies in the United States: a review. Inflamm Bowel Dis. 2011;17(7):1603–9.
Talley NJ. Functional gastrointestinal disorders as a public health problem. Neurogastroenterol Motil. 2008;20(Suppl 1):121–9.
Kretzschmar K, Clevers H. Organoids: modeling development and the stem cell niche in a dish. Dev Cell. 2016;38(6):590–600.
Min S, Kim S, Cho SW. Gastrointestinal tract modeling using organoids engineered with cellular and microbiota niches. Exp Mol Med. 2020;52(2):227–37.
Feng J, van der Zwaag M, Stokman MA, van Os R, Coppes RP. Isolation and characterization of human salivary gland cells for stem cell transplantation to reduce radiation-induced hyposalivation. Radiother Oncol. 2009;92(3):466–71.
Sato T, Vries RG, Snippert HJ, Van De Wetering M, Barker N, Stange DE, et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009;459(7244):262–5.
Sato T, Stange DE, Ferrante M, Vries RG, Van Es JH, Van Den Brink S, et al. Long-term expansion of epithelial organoids from human colon, adenoma, adenocarcinoma, and Barrett’s epithelium. Gastroenterology. 2011;141(5):1762–72.
Fujii M, Matano M, Toshimitsu K, Takano A, Mikami Y, Nishikori S, et al. Human intestinal organoids maintain self-renewal capacity and cellular diversity in niche-inspired culture condition. Cell Stem Cell. 2018;23(6):787-93.e6.
Jung P, Sato T, Merlos-Suárez A, Barriga FM, Iglesias M, Rossell D, et al. Isolation and in vitro expansion of human colonic stem cells. Nat Med. 2011;17(10):1225–7.
Fujii M, Clevers H, Sato T. Modeling human digestive diseases with CRISPR-Cas9-modified organoids. Gastroenterology. 2019;156(3):562–76.
Ootani A, Li X, Sangiorgi E, Ho QT, Ueno H, Toda S, et al. Sustained in vitro intestinal epithelial culture within a Wnt-dependent stem cell niche. Nat Med. 2009;15(6):701–6.
Kakni P, Truckenmüller R, Habibović P, van Griensven M, Giselbrecht S. A microwell-based intestinal organoid-macrophage co-culture system to study intestinal inflammation. Int J Mol Sci. 2022;23(23):15364.
Biton M, Haber AL, Rogel N, Burgin G, Beyaz S, Schnell A, et al. T helper cell cytokines modulate intestinal stem cell renewal and differentiation. Cell. 2018;175(5):1307-20.e22.
de Lau W, Kujala P, Schneeberger K, Middendorp S, Li VS, Barker N, et al. Peyer’s patch M cells derived from Lgr5+ stem cells require SpiB and are induced by RankL in cultured “miniguts.” Mol Cell Biol. 2012;32(18):3639–47.
Waddell A, Vallance JE, Hummel A, Alenghat T, Rosen MJ. IL-33 induces murine intestinal goblet cell differentiation indirectly via innate lymphoid cell IL-13 secretion. J Immunol. 2019;202(2):598–607.
Lindemans CA, Calafiore M, Mertelsmann AM, O’Connor MH, Dudakov JA, Jenq RR, et al. Interleukin-22 promotes intestinal-stem-cell-mediated epithelial regeneration. Nature. 2015;528(7583):560–4.
Jung KB, Lee HN, Son YS, Lee MO, Kim Y-D, Oh SJ, et al. Interleukin-2 induces the in vitro maturation of human pluripotent stem cell-derived intestinal organoids. Nat Commun. 2018;9(1):3039.
Kotloff KL, Nataro JP, Blackwelder WC, Nasrin D, Farag TH, Panchalingam S, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet. 2013;382(9888):209–22.
McNab F, Mayer-Barber K, Sher A, Wack A, O’garra A. Type I interferons in infectious disease. Nat Rev Immunol. 2015;15(2):87–103.
Persson BD, Jaffe AB, Fearns R, Danahay H. Respiratory syncytial virus can infect basal cells and alter human airway epithelial differentiation. PLoS ONE. 2014;9(7):e102368.
Heo I, Dutta D, Schaefer DA, Iakobachvili N, Artegiani B, Sachs N, et al. Modelling Cryptosporidium infection in human small intestinal and lung organoids. Nat Microbiol. 2018;3(7):814–23.
Workman MJ, Mahe MM, Trisno S, Poling HM, Watson CL, Sundaram N, et al. Engineered human pluripotent-stem-cell-derived intestinal tissues with a functional enteric nervous system. Nat Med. 2017;23(1):49–59.
Park CS, Nguyen LP, Yong D. Development of colonic organoids containing enteric nerves or blood vessels from human embryonic stem cells. Cells. 2020;9(10):2209.
Eicher AK, Kechele DO, Sundaram N, Berns HM, Poling HM, Haines LE, et al. Functional human gastrointestinal organoids can be engineered from three primary germ layers derived separately from pluripotent stem cells. Cell Stem Cell. 2022;29(1):36-51.e6.
Bein A, Shin W, Jalili-Firoozinezhad S, Park MH, Sontheimer-Phelps A, Tovaglieri A, et al. Microfluidic organ-on-a-chip models of human intestine. Cell Mol Gastroenterol Hepatol. 2018;5(4):659–68.
Huh D, Kim HJ, Fraser JP, Shea DE, Khan M, Bahinski A, et al. Microfabrication of human organs-on-chips. Nat Protoc. 2013;8(11):2135–57.
Lefebvre DE, Venema K, Gombau L, Valerio LG Jr, Raju J, Bondy GS, et al. Utility of models of the gastrointestinal tract for assessment of the digestion and absorption of engineered nanomaterials released from food matrices. Nanotoxicology. 2015;9(4):523–42.
Huh D, Torisawa YS, Hamilton GA, Kim HJ, Ingber DE. Microengineered physiological biomimicry: organs-on-chips Lab Chip. 2012;12(12):2156–64.
Kim HJ, Huh D, Hamilton G, Ingber DE. Human gut-on-a-chip inhabited by microbial flora that experiences intestinal peristalsis-like motions and flow. Lab Chip. 2012;12(12):2165–74.
Rodriguez-Rodriguez R, Muñoz-Berbel X, Demming S, Büttgenbach S, Herrera M, Llobera A. Cell-based microfluidic device for screening anti-proliferative activity of drugs in vascular smooth muscle cells. Biomed Microdevices. 2012;14:1129–40.
Grosberg A, Nesmith AP, Goss JA, Brigham MD, McCain ML, Parker KK. Muscle on a chip: in vitro contractility assays for smooth and striated muscle. J Pharmacol Toxicol Methods. 2012;65(3):126–35.
Zhang B, Montgomery M, Chamberlain MD, Ogawa S, Korolj A, Pahnke A, et al. Biodegradable scaffold with built-in vasculature for organ-on-a-chip engineering and direct surgical anastomosis. Nat Mater. 2016;15(6):669–78.
Fernández-Costa JM, Tejedera-Vilafranca A, Fernández-Garibay X, Ramón-Azcón J. Muscle-on-a-chip devices: a new era for in vitro modelling of muscular dystrophies. Dis Model Mech. 2023;16(6):dmm050107.
Rayhan RU, Stevens BW, Raksit MP, Ripple JA, Timbol CR, Adewuyi O, et al. Exercise challenge in Gulf War Illness reveals two subgroups with altered brain structure and function. PLoS One. 2013;8(6):e63903.
Phillips RJ, Kieffer EJ, Powley TL. Aging of the myenteric plexus: neuronal loss is specific to cholinergic neurons. Auton Neurosci. 2003;106(2):69–83.
Hanani M, Fellig Y, Udassin R, Freund HR. Age-related changes in the morphology of the myenteric plexus of the human colon. Auton Neurosci. 2004;113(1–2):71–8.
Van Norman GA. Limitations of animal studies for predicting toxicity in clinical trials: is it time to rethink our current approach? JACC Basic Transl Sci. 2019;4(7):845–54.
Karakan T, Gundogdu A, Alagözlü H, Ekmen N, Ozgul S, Tunali V, et al. Artificial intelligence-based personalized diet: a pilot clinical study for irritable bowel syndrome. Gut Microbes. 2022;14(1):2138672.
Mahurkar-Joshi S, Chang L. Epigenetic mechanisms in irritable bowel syndrome. Front Psychiatry. 2020;11:805.
Shin A, Kashyap PC. Multi-omics for biomarker approaches in the diagnostic evaluation and management of abdominal pain and irritable bowel syndrome: what lies ahead. Gut Microbes. 2023;15(1):2195792.
Camilleri M, Zhernakova A, Bozzarelli I, D’Amato M. Genetics of irritable bowel syndrome: shifting gear via biobank-scale studies. Nat Rev Gastroenterol Hepatol. 2022;19(11):689–702.
Keating D, Zundel C, Abreu M, Krengel M, Aenlle K, Nichols M, et al. Boston biorepository, recruitment and integrative network (BBRAIN): a resource for the Gulf War Illness scientific community. Life Sci. 2021;284:119903.
Gifford EJ, Vahey J, Hauser ER, Sims KJ, Efird JT, Dursa EK, et al. Gulf war illness in the Gulf war era cohort and biorepository: the Kansas and centers for disease control definitions. Life Sci. 2021;278:119454.
Brady CB, Trevor KT, Stein TD, Deykin EY, Perkins SD, Averill JG, et al. The Department of Veterans Affairs Biorepository Brain Bank: a national resource for amyotrophic lateral sclerosis research. Amyotroph Lateral Scler Frontotemporal Degener. 2013;14(7–8):591–7.
Brady CB, Robey I, Stein TD, Huber BR, Riley J, Abdul Rauf N, et al. The department of veterans affairs Gulf war veterans’ illnesses biorepository: supporting research on Gulf war veterans’ illnesses. Brain Sci. 2021;11(10):1349.
Khalil L, McNeil RB, Sims KJ, Felder KA, Hauser ER, Goldstein KM, et al. The Gulf War era cohort and biorepository: a longitudinal research resource of veterans of the 1990–1991 Gulf War era. Am J Epidemiol. 2018;187(11):2279–91.
Yates PL, Case K, Sun X, Sullivan K, Baas PW, Qiang L. Veteran-derived cerebral organoids display multifaceted pathological defects in studies on Gulf War Illness. Front Cell Neurosci. 2022;16:979652.
Yates PL, Patil A, Sun X, Niceforo A, Gill R, Callahan P, et al. A cellular approach to understanding and treating Gulf War Illness. Cell Mol Life Sci. 2021;78(21–22):6941–61.
Vahey J, Gifford EJ, Sims KJ, Chesnut B, Boyle SH, Stafford C, et al. Gene-toxicant interactions in Gulf War Illness: differential effects of the PON1 genotype. Brain Sci. 2021;11(12):1558.
Acknowledgements
All figures were created with BioRender.com.
Funding
This work was supported by the Congressionally Directed Medical Research Program Award through the Gulf War Illness Research Program (SAR, W81XWH-21–1-0477). This work was also made possible by funding from the Aviles-Johnson Doctoral Diversity Fellowship Award, and the National Defense Science and Engineering Graduate Fellowship Awards (CAC).
Author information
Authors and Affiliations
Contributions
CAC, AS, SS, and SF wrote initial drafts of the manuscript, which were critically reviewed and revised by SAR and CAC. All authors agreed on the final submission of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Collier, C.A., Salikhova, A., Sabir, S. et al. Crisis in the gut: navigating gastrointestinal challenges in Gulf War Illness with bioengineering. Military Med Res 11, 45 (2024). https://doi.org/10.1186/s40779-024-00547-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40779-024-00547-2